This is the case of a 58 year-old man with a painful tumour in his right ankle, resulting from a long development. An osteolytic injury was found in an X-ray, formed by bone or osteoid trabeculae surrounded by epithelioid osteoblasts and amongst these cells there were osteoclast-type multinucleated cells. The histogenesis of the tumour, the differential diagnosis and the treatment modalities are reported.
Se presenta el caso de un hombre de 58 años de edad con un tumor doloroso en el tobillo derecho, de larga evolución. Radiológicamente se encontró una lesión osteolítica, con un anillo de esclerosis en el astrágalo. Histológicamente el tumor, está formado por trabéculas de hueso u osteoide rodeadas de osteoblastos epitelioides y entre estas células hay células multinucleadas tipo osteoclasto. Se comenta la histogénesis del tumor, el diagnóstico diferencial y las modalidades de tratamiento.
The two clinically important varieties of osteoblastoma are: conventional osteoblastoma and epithelioid or aggressive osteoblastoma.
Conventional (CO) or ordinary osteoblastomas are low-frequency bone-forming tumours that are routinely larger than 2cm. They are formed by osteoblasts that deposit bone trabeculae.
In the Mayo Clinic series, they form 1% of bone tumours and 3.5% of benign primary bone tumours. They occur in 72% of cases in men.1,2
CO has been localised in most bones of the body but predominates in the spine 32%, femur 12%, tibia 10% and bones in the foot and ankle 9% (2). In the cases in the foot, 4.6% present in the tarsal bones.1
Patients’ ages range from 6 months to 75 years, with an average of 20 years, but 75% of patients are younger than 25 years.2 Clinically, it is characterised by pain accompanied or not by an increase in volume. The first symptom is due to the presence of axons in the tumour and the release of prostaglandins by the tumours.3,4
Radiological studies show a lesion that expands to the bone, well-defined and surrounded by a bone crust. Mineralisation is variable but generally has a lithic appearance, surrounded by a ring of sclerosis; there may be oedema and inflammation of the soft tissues. The morphological findings are best demonstrated with CT scans and MRIs.2,5
Macroscopically, the fragments of curettage are haemorrhagic, of friable consistency and with a sandy surface. When the CO is removed in block, it is seen to be very well demarcated, sometimes with cysts full of blood.
Histologically, the osteoid and bone trabeculae have a regular appearance; they are surrounded by uniform osteoblasts. The intertravecular space is occupied by vascular tissue with osteoblasts and fusiform cells. There is no permeation to preexisting lamellar bone.2
The histological varieties of CO include those with cystic changes, others with cartilaginous matrix, those with large and bizarre stromal cells with a degenerate appearance (these tumours have also been called pseudo-malignant osteoblastomas) and finally the group showing small areas of epithelioid-type osteoblastic cells. From these it is necessary to separate CO, since in the latter epithelioid areas are predominant and also have a different clinical behaviour.1,6
The treatment of CO is curettage and occasionally block resection; with curettage the recurrence is 10%–20%. Malignant transformation is rare.7
Radiation therapy or chemotherapy is not indicated in CO, even when the tumour appears to respond to chemotherapy.8
The purpose of this publication is to present the first case of epithelioid osteoblastoma or aggressive osteoblastoma recorded in the archives of the Pathology Department of the “Dr. Eduardo Liceaga” Hospital General de México. This tumour is less common than CO and so it is important to recognise it in order to make a correct diagnosis and avoid overtreatment by confusing it with osteosarcoma and performing mutilating surgery.
Case reportA 58-year-old man with no relevant history for his current condition. The current condition began 6 years before his hospital admission, with sharp pain in the right ankle, with an intensity of 3/10 on the VAS scale, pain subsided with non-steroidal painkillers; it was later associated with an increase in volume of the anteromedial side of the ankle. The pain increased in intensity up to 8/10, with flexoextension limitation of the ankle; it was under these conditions that he was admitted to hospital.
During the physical examination, the right ankle showed dorsal bending of 50° and plantar bending of 30°. The movements caused joint pain and a soft tumour was found on the anteromedial side of the ankle at the level of the tibioplasty joint, adhered to deep planes, painful to the touch and 3×3cm. The rest of the physical examination was within normal limits.
The anteroposterior and lateral radiographic study showed an osteolytic lesion at the level of the talus, of an ovoid shape and surrounded by a ring of sclerosis (Fig. 1).
Laboratory studies were within normal limits. Treatment was performed by bone curettage in the neck of the talus, without postoperative complications.
In the laboratory of the Surgical Pathology Unit, several irregular fragments of tissue were received; together they measured 3×2×1cm. One part consisted of white, hard bone fragments; other fragments were soft, friable, with a sandy surface and dark brown colour.
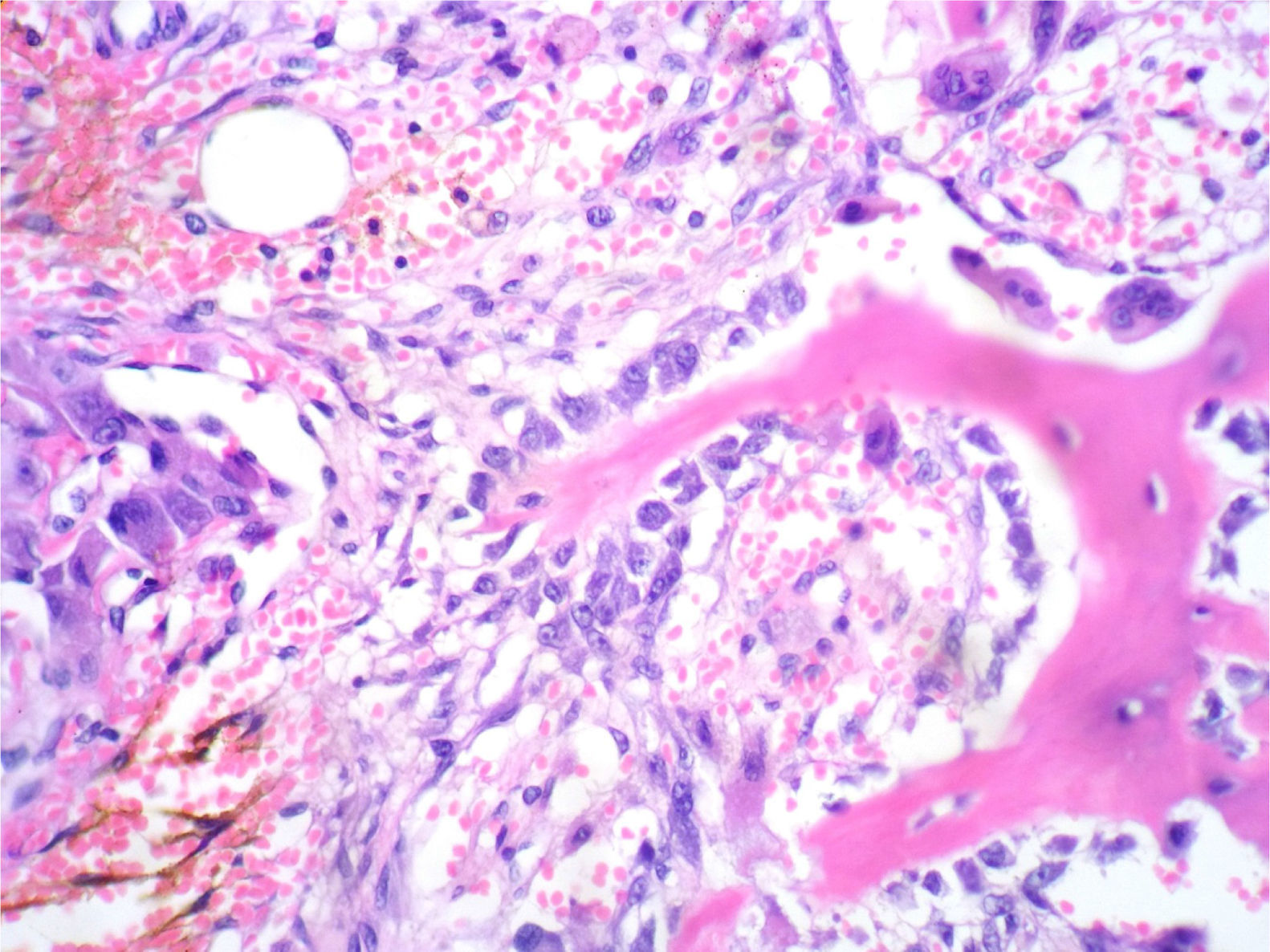
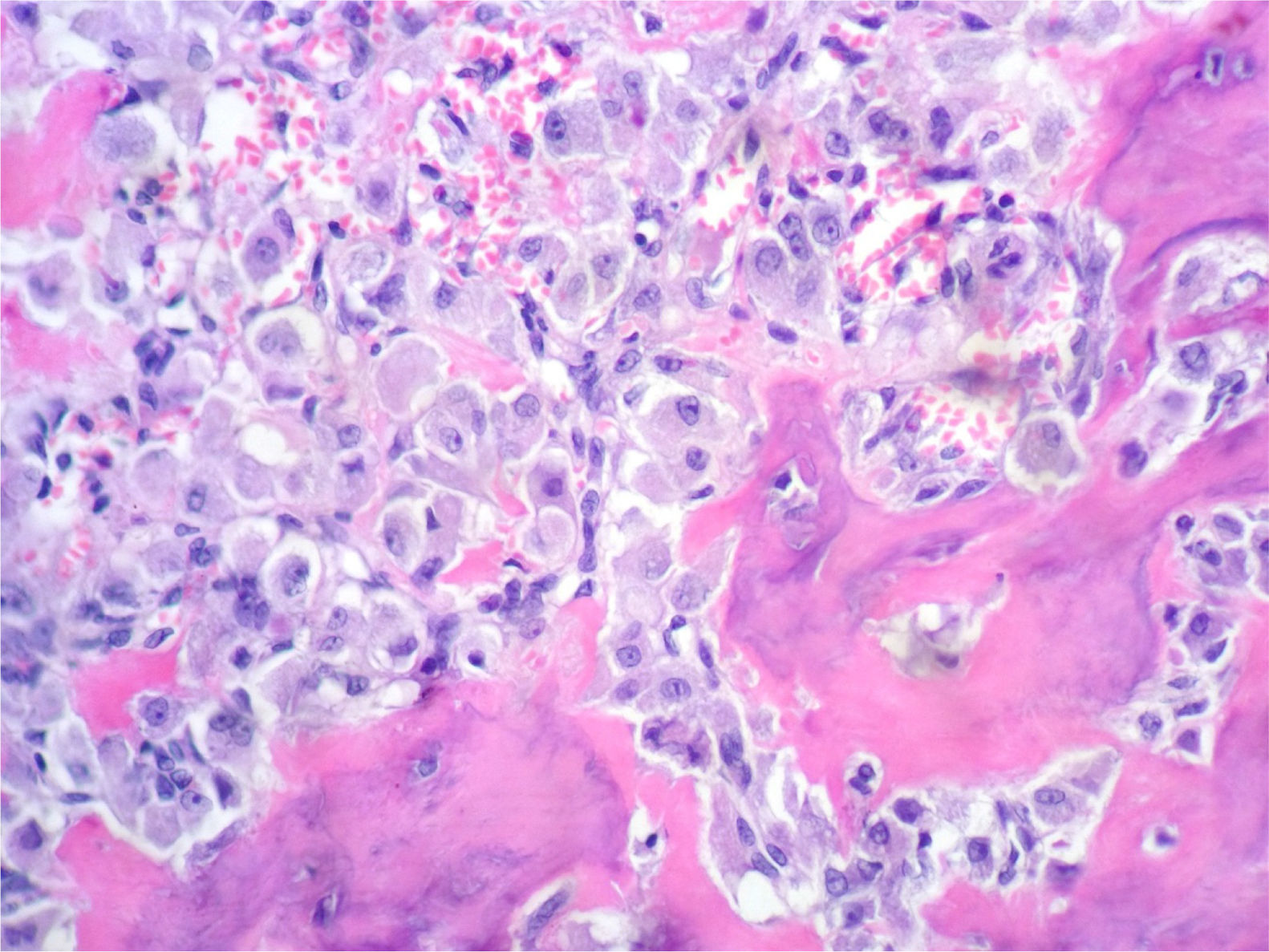
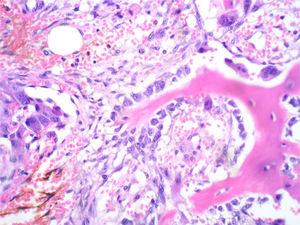
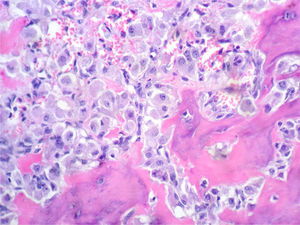
In the histological sections, there was trabecular and osteoid bone surrounded by epithelioid osteoblasts without cellular atypia or mitotic activity; the osteoblasts did not permeate the bone trabeculae or the osteoid they were forming. The stroma had a vascularised fibroblastic appearance and in this some multinucleated, osteoclast-type giant cells were observed (Figs. 2 and 3).
Osseous spicules surrounded by epithelioid osteoblasts, which do not invade newly formed bone. In the left half, there are accumulations of epithelioid osteoblasts, abundant erythrocytes and haemosiderin. In the upper right corner, there are 3 giant osteoclastic cells. The stroma is fibroblastic-vascularised. HE 200×.
Aggressive osteoblastoma (AO), a very rare tumour that represents a borderline lesion between CO and osteosarcoma. They are tumours that recur but do not metastasise. They are characterised microscopically by the presence of the so-called epithelioid osteoblasts.8
They occur between the 3rd and 4th decades, with limits between 7 years and 80 years of age. No difference has been observed between the sexes.8 The bones that it affects are similar to CO, in the axial skeleton, and the second most frequent location are the bones of the hands and feet.
The x-ray image consists of a circumscribed osteolytic defect, surrounded by a ring of sclerosis. The bone contour may be markedly expanded and has a reactive bone ring. In small bones in the hands and feet, the lesion may cross the joint space and affect the adjacent bone, giving a clear indication of its local aggressive nature.9
Macroscopically, the lesion is oval or rounded. The tissue is granular, friable, reddish and perhaps with blood during curettage due to its richly vascularised stroma. The bone surrounding the lesion is thinly expanded and with the crust focally missing. Extension to soft tissues can be observed.10
Microscopically, it shows irregular chains of trabecular bone, distributed between lax fibroblastic stroma with prominent vessels. Osteoid in some foci may not be trabecular but may take an inlay pattern surrounding individual cells. There are also large areas of osteoid involving individual epithelioid osteoblasts.
Epithelioid osteoblasts are rounded tumour-characteristic cells, twice the size of an ordinary osteoblast. They show abundant eosinophilic cytoplasm, large rounded and eccentric nucleus and prominent nucleolus. In the cytoplasm, there may be clear areas that compress and displace the nucleus.
The mitotic activity between the epithelioid osteoblasts varies from 1 to 4 mitosis by 20 fields of large increase and no atypical mitosis is detected. There is no mitosis in osteoclast-like cells that also present these tumours. Secondary aneurysmal bone cyst can be found both macro- and microscopically.10–13
Immunohistochemistry with osteocalcin is positive and demonstrates the osteoblastic nature of the epithelioid cells.14
From the cytogenetic point of view, a deletion of the long arm of chromosome 22 has been found. This alteration affects a total of 10 genes, but 4 are particularly important, since they intervene in osteogenesis and in tumorigenesis, namely the following genes: ZNRF3, KREMEN, MN and NF2.15
The differential diagnosis should be made with osteoid osteoma, CO and osteosarcoma. The difference with the first 2 are the lamellae of epithelioid osteoblasts, which fill in the intertrabecular spaces in the AO, since in the osteoid osteoma and the CO, occasionally and in an isolated form, epithelioid osteoblasts can be found.
The difference with osteosarcoma is that in the latter there is cellular atypia, a high index of mitosis, many of them abnormal, abundant osteoid and permeation to bone and adjacent soft tissues.10,16
The prognosis of AO is recurrence, which occurs in up to 50% of cases.2,5 The treatment is performed by curettage or block marginal resection; the latter is the treatment of choice to try to avoid recurrences.13,17 The transformation to osteosarcoma has been reported, mainly after multiple relapses.2
Our case combines the clinical, radiological, macroscopic and mainly histopathological characteristics to perform the diagnosis of aggressive osteoblastoma or epithelioid osteoblastoma.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors declare that they have no conflicts of interest.