Gastrointestinal stromal tumours (GISTs) are the most common mesenchymal tumour in the gastrointestinal tract. More than half of these originate in the stomach, the rest in the small intestine, colon, rectum and oesophagus, and rarely in the omentum.
Case reportA 48-year-old woman, with painful abdominal growth developing over two years. Radiological studies showed a heterogeneous solid lesion in the pelvis, so she underwent surgery and the omentum was resected, no evidence of a tumour was found in the gastrointestinal tract. The omentum measured 50cm×30cm×15cm. Its surface was heterogeneous and showed multiple nodules of varying sizes. A microscopically diffuse pattern of spindle cells was observed, some of them epithelioid, with three mitoses in 50 high-power fields. The immunohistochemical study is positive for CD117 and DOG-1.
E-GIST should be considered for the differential diagnosis of patients with multinodular lesions in the omentum and mesentery.
El tumor del estroma gastrointestinal (GIST) es el tumor mesenquimatoso más frecuente del tubo digestivo. Más de la mitad de estos se originan en estómago, el resto en intestino delgado, colon, recto y esófago; excepcionalmente en epiplón.
Caso clínicoMujer de 48 años con crecimiento doloroso abdominal de 2 años de evolución. Los estudios radiológicos mostraron una lesión sólida heterogénea en pelvis, por lo que fue intervenida quirúrgicamente y se resecó epiplón, no se encontró evidencia de tumor en el tracto gastrointestinal. El epiplón midió 50×30×15cm. Su superficie es heterogénea, presenta múltiples nódulos de diferentes tamaños. Microscópicamente se observa un patrón difuso de células fusiformes, algunas de ellas epitelioides con 3 mitosis en 50 campos de alta resolución. El estudio de inmunohistoquímica es positivo para CD117 y DOG-1.
El E-GIST, se debe considerar en el diagnóstico diferencial de pacientes con lesiones multinodulares en epiplón y mesenterio.
Gastrointestinal stromal tumours (GISTs) are the most common primary mesenchymal tumour in the gastrointestinal tract, with an incidence of 11–15 people per every 100,000. They account for 1% of gastrointestinal neoplasms, and most present in adults and in men,2 but there are cases reported in children.3 Most of the reported E-GIST cases are described in elderly patients.4–6
More than 50% of GISTs are found in the stomach, 25–30% in the small intestine (jejunum and ileum), 5% in the colon and rectum, and 1% in the oesophagus. Cases have been reported in the mesentery and omentum,1,2 as well as in other organs, such as the pancreas,7 uterus8 and vaginal wall.9 They originate from the interstitial cells of Cajal and present mutations in the c-KIT genes and platelet-derived growth factor receptor (PDGFRA) which leads to tyrosine kinase activation.10 The clinical presentation of these tumours depends on their location and size; however, in advanced stages, they occur with abdominal pain, ileus, bleeding, anaemia and weight loss.7
The importance of this case of primary E-GIST in the omentum involves its location and unusual presentation, since there are few cases reported in the literature; thus there is no reported incidence.
Case reportA 48-year-old woman who was admitted to the Oncology Department of the Hospital General de México, with symptoms starting two years prior characterised by repeated urinary tract infections, treated with antibiotics and analgesics with little response. An increase in her waist circumference occurred later on with colic-like pain predominantly in both iliac fossae, which did not ease when analgesics were administered, accompanied by episodes of fever, with no weight loss. No signs of intestinal occlusion or any other gastrointestinal symptoms were reported. A well defined, mobile tumour in the pelvis was palpated during a physical examination, located up to 3cm above the navel, which was impossible to rule out on palpation to examine the rest of the abdominal/pelvic organs. Therefore, a clinical diagnosis of ovarian cancer was established. Serum tumours markers were negative, and a computerised tomography scan showed a solid, heterogeneous lesion in the pelvis, which was multi-lobulated with cystic degeneration and calcifications measuring 17cm×12cm×6cm with 636 cubic cm of fluid. There was also mesenteric lymph node growth. The omentum that was surgically resected was described as a “cluster of grapes” with implants with the same characteristics in the surface of the mesocolon, uterine surface, both ovary surfaces and uterine tubes. In the gastrointestinal tract, only an ileal occlusion was reported due to a superficial tumour implant, thus the superficial ileum implant and the rest of the implants were surgically resected and sent to the Surgical Pathology department for pathological study along with the omentum.
In the surgery, the liver and stomach did not show any macroscopic abnormalities in their morphologies, nor any superficial implants in the omentum tumour. As mentioned above, the established clinical diagnosis was undifferentiated omentum carcinoma. It is important to mention that, in the imaging studies and during the surgery, no evidence was found of a tumour in the gastrointestinal tract.
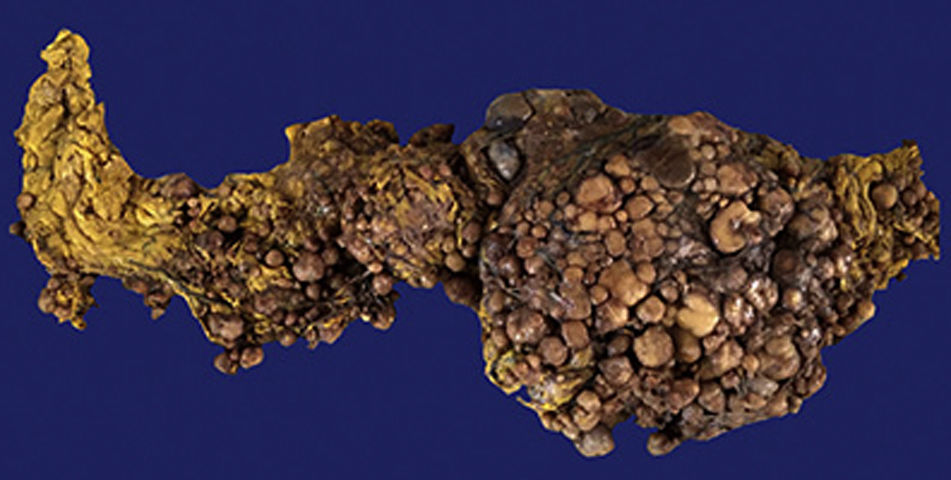
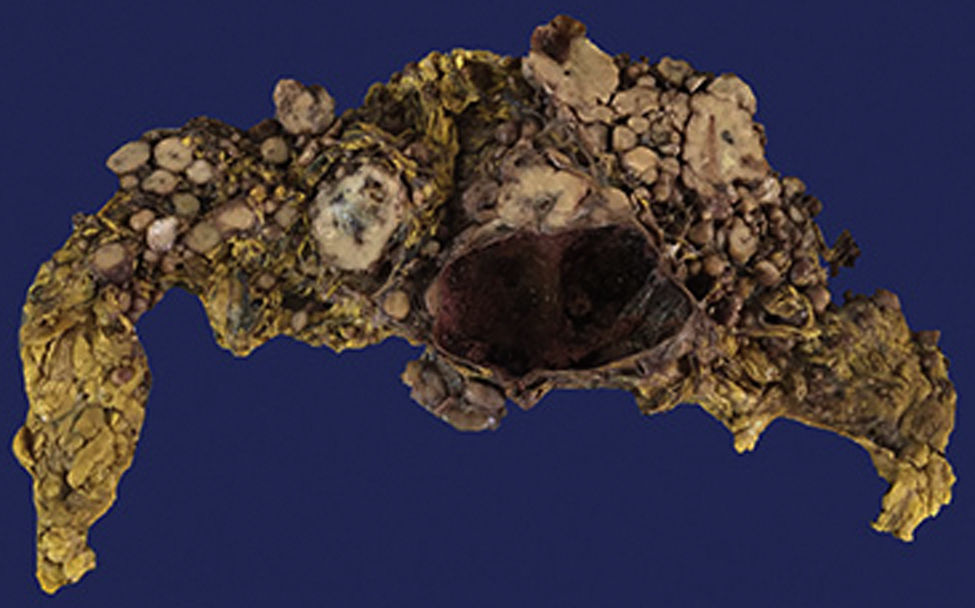
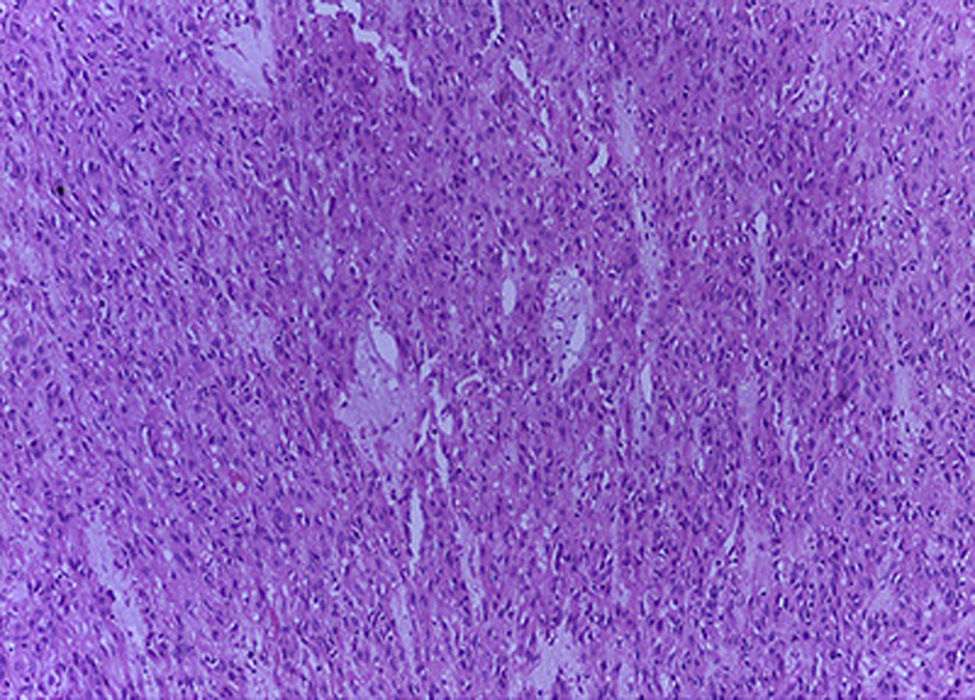
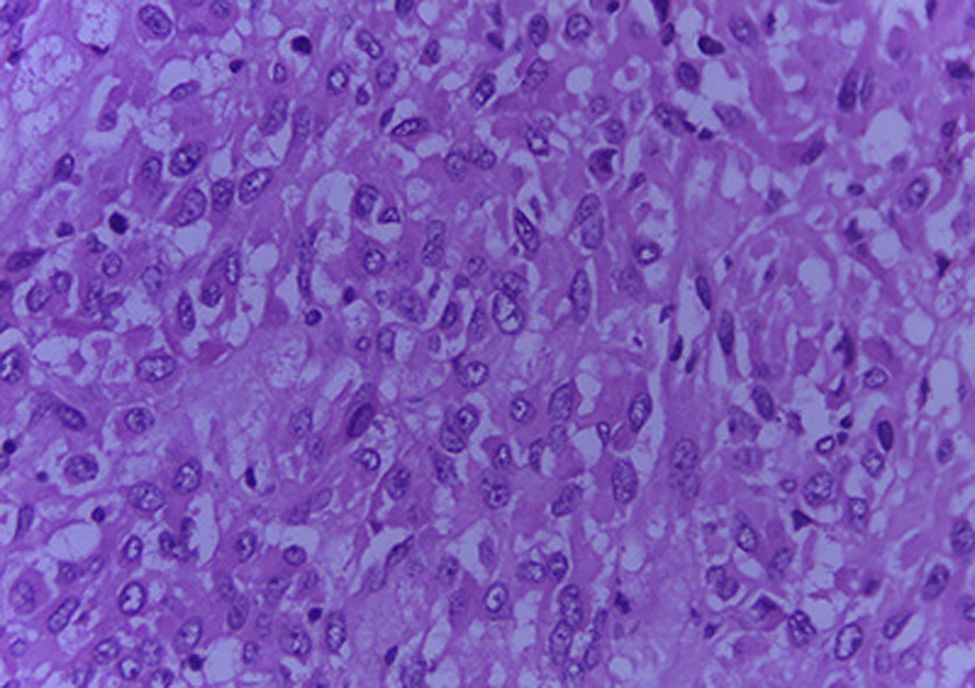
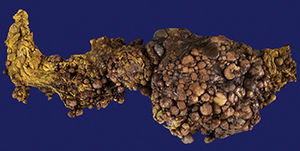
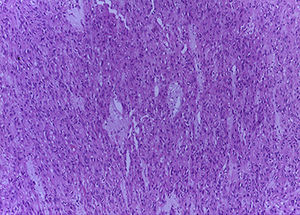
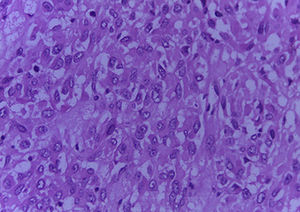
The Surgical Pathology department received the omentum (Fig. 1), which measured 50cm×30cm×15cm and weight 3,500g. Its exterior surface presented multiple, well-defined nodules measuring from 1 to 15cm on the major axis that were light yellow in colour. On the slice surface, most of the nodules were solid, some with necrosis and haemorrhage, and one was cystic with blood inside (Fig. 2). Implants with the same characteristics were found on the round ligaments and the ileal serosa. There were no macroscopic abnormalities to the ovaries. A diffuse neoplasm composed of spindle cells and some epithelioid cells with clear cytoplasm and prominent nucleoli was found in the microscopic study, with 3 mitoses present in 50 high-power fields (Figs. 3 and 4). There were areas of haemorrhage and liquefactive necrosis. The ovaries did not show microscopic abnormalities; therefore, a primary lesion of the ovaries was ruled out.
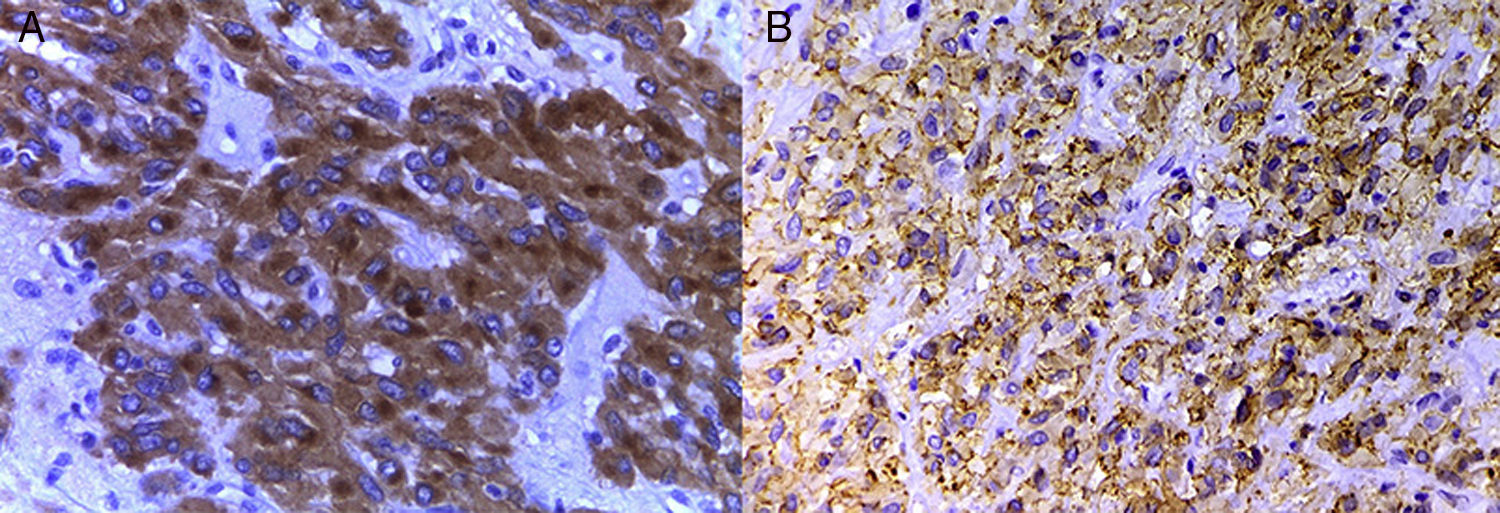
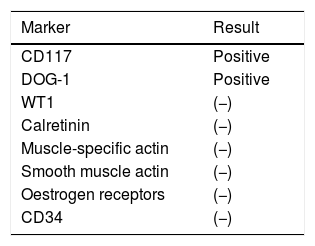
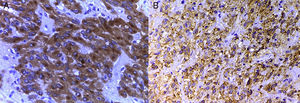
Immunohistochemical studies were ordered with the following markers (Table 1), which were positive for CD117 and DOG-1 (Fig. 5A and B). With all the above information, a primary extra-gastrointestinal stromal tumour in the omentum was diagnosed. Peritoneal leiomyomatosis was ruled out since the smooth muscle actin and muscle-specific actin markers were negative, as well as spindle cell peritoneal mesothelium since the calretinin and WT1 markers were negative.
The patient progressed adequately, with no signs of intestinal obstruction and no abdominal pain, with no clinical or laboratory signs of urinary tract infection. She was discharged 10 days after the surgery due to improvement. She later started treatment with imatinib as she was a candidate since the CD117 marker was positive. Three months later, she reported episodes of bleeding when defecating, bone pain, and “hot flushes” which stopped, and she continued the treatment with imatinib. At four months, she presented with signs of drug-induced grade IV neutropenia, as well as late, postprandial colic-like pain, with no signs of peritoneal irritation and the treatment was discontinued. One week later, she recovered from the neutropenia, and reported dysuria on one occasion and pain in the left flank near the kidneys. The last follow-up was at 5 months, and she reported generalised pain. No palpable tumour was found during the physical examination nor were any signs of clinical tumour activity, with signs of grade II neutropenia. Plans were made to reinitiate treatment with imatinib.
DiscussionMacroscopically, GISTs present as nodules in the stroma or subserosa in the gastrointestinal tract.2 The E-GISTs reported in the literature are very similar to that of our case, and are described as a large tumour with multiple nodules, some red in colour, others a light yellow, with areas of haemorrhage and necrosis.1,2,4,6,11,12
Microscopically, these tumours can be classified as spindle cell (70%), epithelioid (20%), and mixed (10%).9 This case was classified as mixed since she had both types of cells. Some had enlarged nuclei and were hyperchromic which is associated with higher tumour aggression. The mitosis can vary from little to abundant, and some can present atypical mitoses.2
These tumours are characterised by c-KIT gene mutations, or PDGFRA mutations; both genes lead to tyrosine kinase activation.10 The cases with c-KIT mutation are positive for the CD117 marker,1,2 and adequately response to imatinib therapy.10 Cases with PDGFRA mutations are usually negative for the CD117 marker and are called “wild-type”. In these cases, another marker such as DOG-1 (discovered in GIST-1) has been found to have a higher specificity and sensitivity than CD117,13 and is used to confirm GIST diagnosis.2,10 It cannot be stated that CD117 or DOG-1 are expressed exclusively in GISTs, since although they are highly specific for them, they are also rarely expressed in other tumours such as leiomyosarcomas, leiomyomas, and leiomyoblastomas, among others.14 The CD34 marker can also be used in GISTs, but it is not specific and is only expressed in 25% of cases.2,5,12 In E-GIST cases where the CD34 marker test has been performed, the results have been reported to be negative,5,12 as in our case.
Risk stratification in these tumours has been classified based on the tumour size (0.1, 2, 5, 10, 15 and 25cm), the number of mitoses (0, 2, 5, 10, 15, 25 and 50 mitoses in 50 high-power fields) and primary tumours site (gastric with or without rupture, non-gastric with or without rupture, and extra-gastrointestinal with or without rupture).2 In this case, due to the large size over 10cm, with fewer than 5 mitoses and being extra-gastrointestinal without rupture, it was considered high risk. The treatment of choice is surgical resection and treatment with tyrosine kinase inhibitors such as imatinib.1,2,15 In advanced cases, liver metastasis is present most of the time, whereas metastasis occurs less frequently in other organs such as in the ovaries. Metastasis in the lymph nodes is rare.1,2 In this case, the patient presented multiple superficial abdominal implants.
The risk of recurrence has been associated with the loss of the c-KIT gene.2 It usually occurs in the first two years,1 involving the liver and the peritoneal surface.3
The literature describes primary carcinoma of the peritoneum as a rare tumour that originates in the pelvic and abdominal peritoneum. It is believed to come from a secondary Müllerian system that triggers the start of a primary carcinoma resembling serous papillary carcinoma of the ovary in its histological appearance, spread, treatment and prognosis.16 In this case, the initial focus was as a primary neoplasm of the omentum with a spindle cell pattern. It was thought to be a diffuse peritoneal leiomyomatosis due to the predominance of spindle cells, low mitotic count and no pleomorphism. This was ruled out with the negative markers for smooth muscle actin and muscle-specific actin.17 It was also thought to be peritoneal spindle cell mesothelioma, which was ruled out with the negative markers for calretinin and WT1, which are macroscopically very similar and present as peritoneal nodules.18 As in this case, carcinomas and leiomyosarcomas should be ruled out for large tumours in the omentum.2 Since there is little information about this tumour, it should be considered in the differential diagnosis of patients with large, multi-nodular, primary lesions of the mesentery and omentum.1
As for patient symptoms, there is no correlation with GISTs in the gastrointestinal tract.
ConclusionE-GISTs are very rare. This group of tumours are not well known and involve a large number of diagnostic and therapeutic issues due to the lack of information about their behaviour. Despite generalised knowledge about gastrointestinal stromal tumours, there is a lack of data on patients with E-GIST. Therefore, this type of publication can help to provide useful information on its diagnosis, prognosis and treatment. The diagnosis was of great importance since the treatment changes from one tumour (peritoneal leiomyomatosis or peritoneal mesothelioma) to the next (E-GIST).
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of interestThe authors declare that they have no conflict of interests.