Hysteroscopy is a clinical procedure that allows a gynecologist to see inside the uterus through endoscopy. This can be done for diagnosis or treatment of intrauterine conditions and as a method of surgery.
PurposeTo establish the prevalence of uterine disease in a group of healthy patients who underwent hysteroscopy as part of their gynecological examination.
Materials and methodsIt was an observational study. 18 patients who attended a regular consultation provided by the clinical services of Gynecology and Obstetrics of the General Hospital Pemex Picacho were studied; a hysteroscopy was performed in 7 (38.8%) patients who only attended a usual gynecological examination, were asymptomatic and were without known gynecological pathology.
ResultsWhen performing hysteroscopy, 6 (85.7%) patients with gynecological pathology not previously known were found. The disease most commonly found in this sample was the internal cervical stenosis (28.5%).
ConclusionsHysteroscopy showed a high prevalence of detecting uterine pathologies that were never previously described in a population of healthy women in a common sample of patients attending the outpatient Hospital Pemex Picacho.
La histeroscopía es un procedimiento clínico que le permite a un ginecólogo ver el interior del útero por medio de una endoscopia. Este procedimiento puede realizarse con fines de diagnóstico o para tratamientos de patologías intrauterinas y como método de intervención quirúrgica.
ObjetivoEstablecer la prevalencia de enfermedades uterinas en un grupo de pacientes sanas que se les realiza una histeroscopía como parte de su revisión ginecológica.
Material y métodosEstudio experimental, observacional, se estudiaron a 18 pacientes que acudieron a una consulta habitual por parte del servicio de Ginecología y Obstetricia del Hospital General de Pemex Picacho, se realizó histeroscopía a 7 (38.8%) pacientes que solo acudieron a revisión ginecológica habitual, asintomáticas y sin patología ginecológica conocida.
ResultadosAl realizar una histeroscopía se encontró a 6 (85.7%) pacientes con patología ginecológica antes no conocida. La patología más frecuentemente encontrada en esta muestra fue la de estenosis cervical interna (28.5%).
ConclusionesLa histeroscopía mostro una alta prevalencia de detección de patologías uterinas nunca previamente descrita en una población de mujeres sanas dentro de una muestra habitual de pacientes que acuden a consulta externa del Hospital Pemex Picacho.
Hysteroscopy is a clinical procedure that allows gynecologist to perform an exploration of the uterine cavity through an endoscopy. This can be done for diagnosis or treatment of diseases and as an intrauterine surgery method. First developed in 1865, the first operation performed with a hysteroscope was the removal of uterine polyps in 1869.1–3
The hysteroscope has an optical system, usually connected to a VCR and is luminogenic, with transmission by optical fibers. The gynecologist inserts a lens to view the inside of the uterus; this lens you may connect to a camera to view the image on a monitor. The camera, in turn, can be connected to a VCR, DVD recorder or other recording device video.4–8
Saline, sorbitol or dextrose solution or carbon dioxide is used to distend the uterine cavity; currently, a physiological solution is most often used. After cervical expansion, hysteroscope is guided into the uterine cavity for inspection. If abnormalities are found, it proceeds with the channel of the hysteroscope where you can introduce specialized surgical instruments, such as scissors, tweezers and bipolar electrodes, to operate in the cavity uterina.9–12
Previously, an intervention by hysteroscopy was always performed under general anesthesia, whereas diagnostic hysteroscopy using smaller caliber instruments and being non-invasive was performed without anesthesia. However, nowadays, small diameter (3mm) hysteroscopes have been developed to allow interventions in the query without the need for anesthesia, with a total duration of the procedure no more than twenty minutes.13–25
Primary objectiveTo establish the prevalence of uterine disease in a sample of healthy patients who underwent a hysteroscopy as part of a gynecological examination.
Specific objectives- 1.
To determine uterine pathology most frequently found in a group of healthy patients.
- 2.
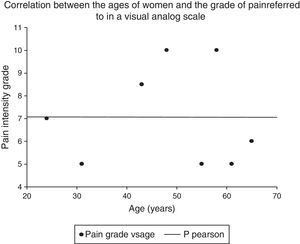
To determine the correlation between age and degree of referred pain in hysteroscopy.
- 3.
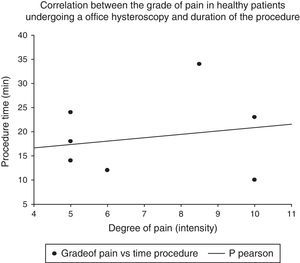
To determine the correlation between the degree of pain in healthy patients undergoing hysteroscopy with the time taken by the procedure.
It is an observational, descriptive and cross-sectional pilot study. 18 patients attending a regular consultation provided by the clinical services of Gynecology and Obstetrics General Hospital Pemex Picacho, asymptomatic and without known gynecological pathology were studied.
Selection criteria: Women over 18 years, with active sexual life and without any known uterine pathology based on a previous ultrasonography.
Exclusion criteria: Women who have undergone surgical events affecting the uterine structure as curettage, diagnostic hieroscopias, cesarean section, myomectomy and tubal occlusion.
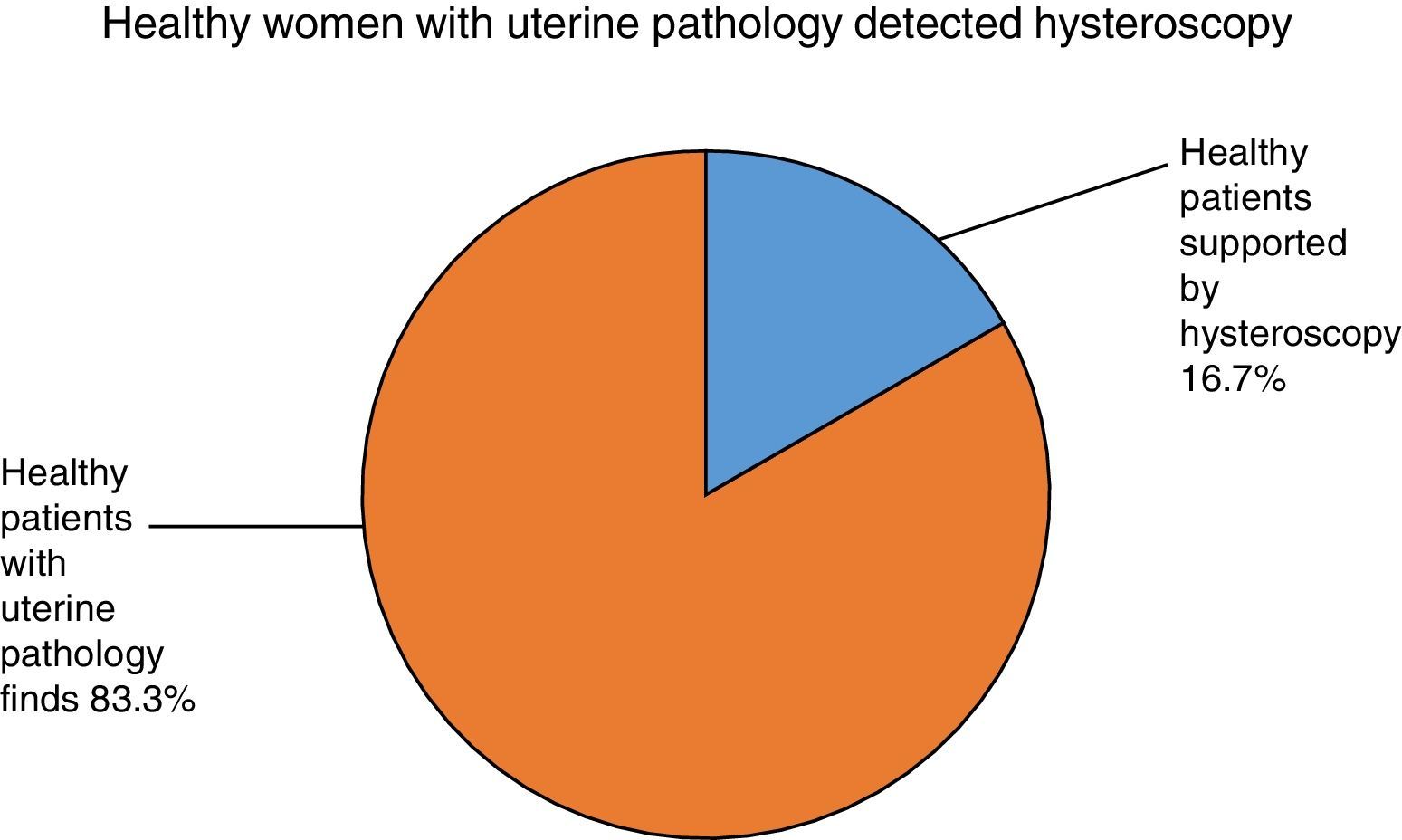
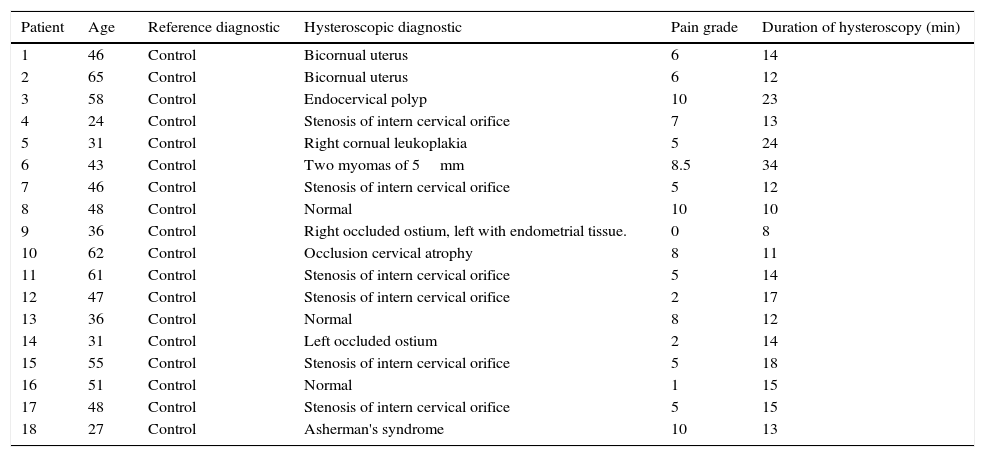
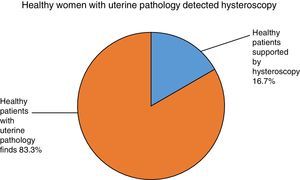
ResultsThe age range varied from 31 to 65 years and the average age was 48.1 and the standard deviation was 18.6. When performing a hysteroscopy in the clinic without sedation, experts found 15 (83.3%) patients with gynecological pathology not previously known (Table 1).
Distribution of uterine diseases discovered by hysteroscopy in a sample of healthy women.
| Patient | Age | Reference diagnostic | Hysteroscopic diagnostic | Pain grade | Duration of hysteroscopy (min) |
|---|---|---|---|---|---|
| 1 | 46 | Control | Bicornual uterus | 6 | 14 |
| 2 | 65 | Control | Bicornual uterus | 6 | 12 |
| 3 | 58 | Control | Endocervical polyp | 10 | 23 |
| 4 | 24 | Control | Stenosis of intern cervical orifice | 7 | 13 |
| 5 | 31 | Control | Right cornual leukoplakia | 5 | 24 |
| 6 | 43 | Control | Two myomas of 5mm | 8.5 | 34 |
| 7 | 46 | Control | Stenosis of intern cervical orifice | 5 | 12 |
| 8 | 48 | Control | Normal | 10 | 10 |
| 9 | 36 | Control | Right occluded ostium, left with endometrial tissue. | 0 | 8 |
| 10 | 62 | Control | Occlusion cervical atrophy | 8 | 11 |
| 11 | 61 | Control | Stenosis of intern cervical orifice | 5 | 14 |
| 12 | 47 | Control | Stenosis of intern cervical orifice | 2 | 17 |
| 13 | 36 | Control | Normal | 8 | 12 |
| 14 | 31 | Control | Left occluded ostium | 2 | 14 |
| 15 | 55 | Control | Stenosis of intern cervical orifice | 5 | 18 |
| 16 | 51 | Control | Normal | 1 | 15 |
| 17 | 48 | Control | Stenosis of intern cervical orifice | 5 | 15 |
| 18 | 27 | Control | Asherman's syndrome | 10 | 13 |
Uterine diseases most frequently encountered in these patients are described. The disease most commonly found in this sample was the internal cervical stenosis in 6 patients (33.3%).
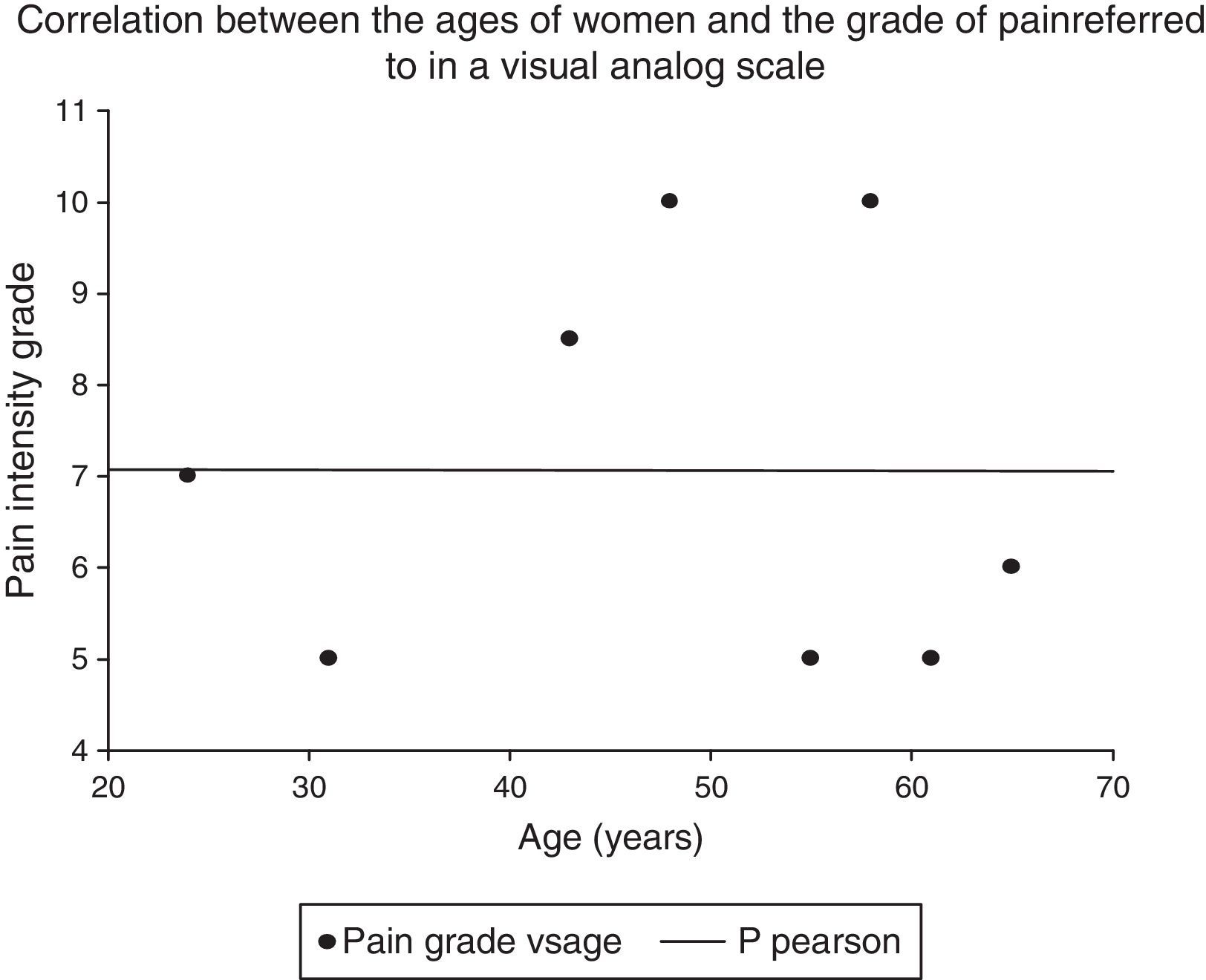
Pearson test was performed to correlate ages of healthy women with the degree of pain expressed according to a visual analog scale R=−0.002 finding and P 0.05 (Graph 1).
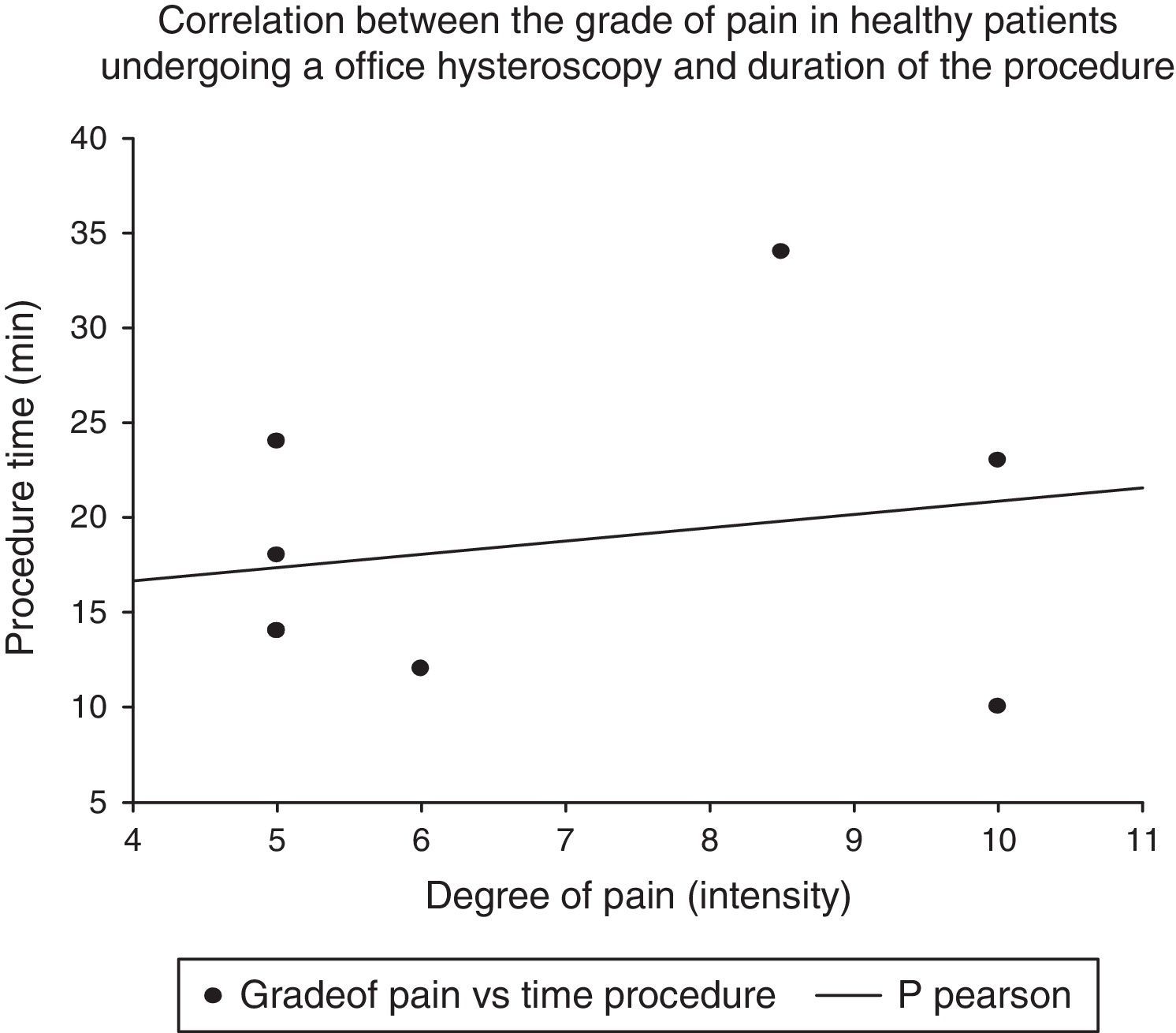
A P-Pearson test was performed to establish the correlation between the degree of pain in healthy women undergoing hysteroscopy and time taken to perform the procedure finding an R=0.20 with a P 0.05 (Graph 2).
The prevalence of uterine pathology found in a sample of healthy patients was 83.3% (Graph 3).
DiscussionIn 2012, Alanis Fuentes and colleagues published a causality detection of abnormal uterine bleeding in a group of study of 1,482 women without a clear diagnosis. In 2013, Sanchez and colleagues identified a diagnostic concordance in the diagnosis of uterine infertility in women when compared with hysterosonography and hysterosalpingography, with greater functionality to establish causality of uterine infertility. Hysteroscopy is considered only as a diagnostic tool for diseases previously diagnosed by clinical or imaging studies; however, in women who are asymptomatic and are considered healthy, uterine pathology requiring treatment can be found in our study in about 83% of the patients; patients who underwent hysteroscopy incidentally diagnosed a condition that would warrant possibly treatment. So, it should be a tool to be incorporated into routine clinical evaluation of care in gynecological patients. As for the correlation between the degree of pain and age, an inversely proportional relationship but with very weak association was found. During this study, a direct relationship was observed, but it was not significant. These last two results are due to the sample size; you must increase the number of participants to make clear if the strength of association is significant.
ConclusionsHysteroscopy showed a high prevalence of detection of uterine pathologies never previously described in a population of healthy women in a typical sample of patients attending outpatient Hospital Pemex Picacho.
Ethical disclosureProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors declare that they have no conflict of interests.