A 58 year-old-woman with no medical history presented to the emergency department complaining of chest pain and dyspnea. An ECG was performed, which showed ST-segment elevation in precordial leads from V1 to V5; elevated values of troponin I serum levels were found. Cardiac catheterization did not show obstructive coronary lesions, however hypokinesis of the apex and left ventricular segments were observed, with sparing of the basal segments. Afterwards a stressor precipitant was identified. The patient was diagnosed of takotsubo cardiomyopathy. Takotsubo cardiomyopathy probably accounts for 1–2% of all cases of suspected acute myocardial infarction, its true prevalence is unknown because of under diagnosis. The pathophysiological aspects of the disease are still a matter of debate and a standard treatment consensus is lacking.
Una mujer de 58 años de edad, sin antecedentes médicos se presentó en la sala de urgencias quejándose de dolor torácico y disnea. Se realizó un electrocardiograma, el cual mostró elevación del segmento ST en las derivaciones precordiales de V1 a V5; los niveles séricos de troponina se encontraron elevados. El cateterismo cardiaco no mostro lesiones coronarias obstructiva, sin embargo se observó hipocinesia del ápex y los segmentos medio-ventriculares, sin afectación de los segmentos basales. Posteriormente un factor de estrés fue identificado. La paciente fue diagnosticada de cardiomiopatía de takotsubo. La cardiomiopatía de takotsubo representa aproximadamente del 1 al 2% de todos los casos de infarto agudo al miocardio, su verdadera prevalencia se desconoce a causa de un infra diagnóstico. Los aspectos fisiopatológicos de la enfermedad son aun sujetos de discusión y se carece de un consenso para tratamiento estándar.
In the early 1990s, Japanese authors reported a reversible cardiomyopathy that seemed to be precipitated by acute emotional stress.1–8 Patients were usually postmenopausal women and developed signs and symptoms of an acute coronary syndrome associated with a transient apical and mid-ventricular wall motion abnormality despite the lack of obstructive coronary artery disease at the time of emergent coronary angiography, which usually recovers from weeks to months.1,2
The shape of the ventricle at end systole resembled the Japanese fisherman's octopus pot – the takotsubo – from which the syndrome derives its original name.1–3
It is now recognized that takotsubo cardiomyopathy (TC) stressor is not just an acute emotional stress, but also acute intracranial events, including intracranial bleeding, head trauma and ischemic stroke; acute medical illness, including sepsis and surgical procedures; overproduction of endogenous catecholamines (pheochromocytoma); and administration of exogenous catecholaminergic agents can be precipitant factors for the disease. TC has been acknowledged by the ACC/AHA as a unique form of reversible cardiomyopathy.1
Clinical caseA 58 year-old-woman with no medical history, presented to the emergency department complaining of oppressive chest pain of moderate intensity accompanied by dyspnea 6-h lasting.
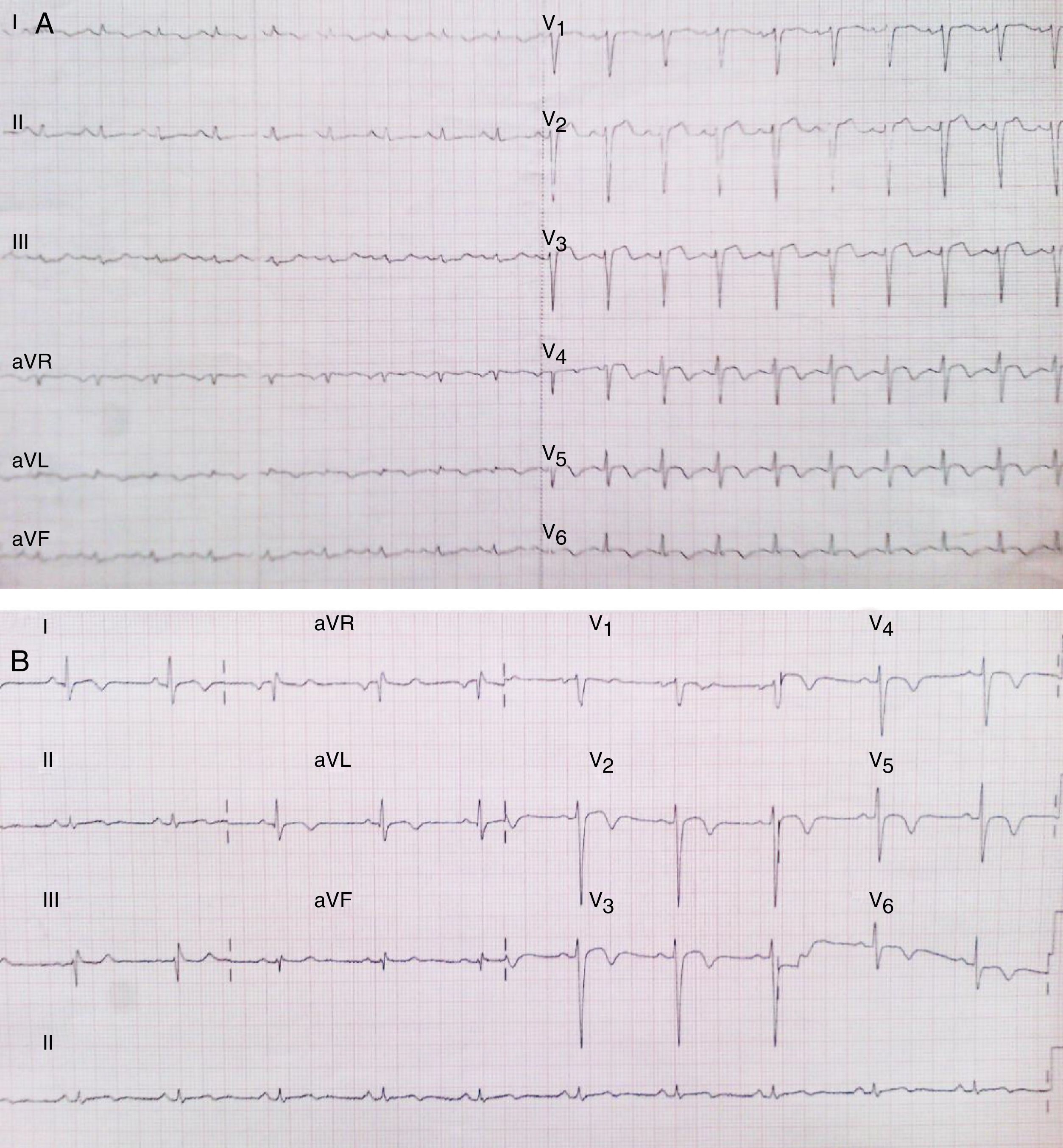
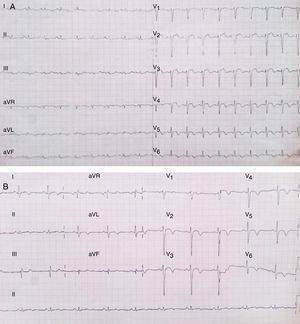
An electrocardiogram (ECG) was performed on admission, which showed ST-segment elevation in precordial leads from V1 to V5, and T-wave inversion from V4 to V6 (Fig. 1A). Initial troponin I determination showed a value of 3.7ng/ml which was above the 99th percentile upper reference limit.
(A) ECG recording at presentation which shows ST-segment elevation in precordial leads from V1 to V5 and T-wave inversion in V4–V6. (B) ECG recording at the third day of hospitalization showing progression from ST segment elevation to inverted symmetrical T-waves in all precordial leads.
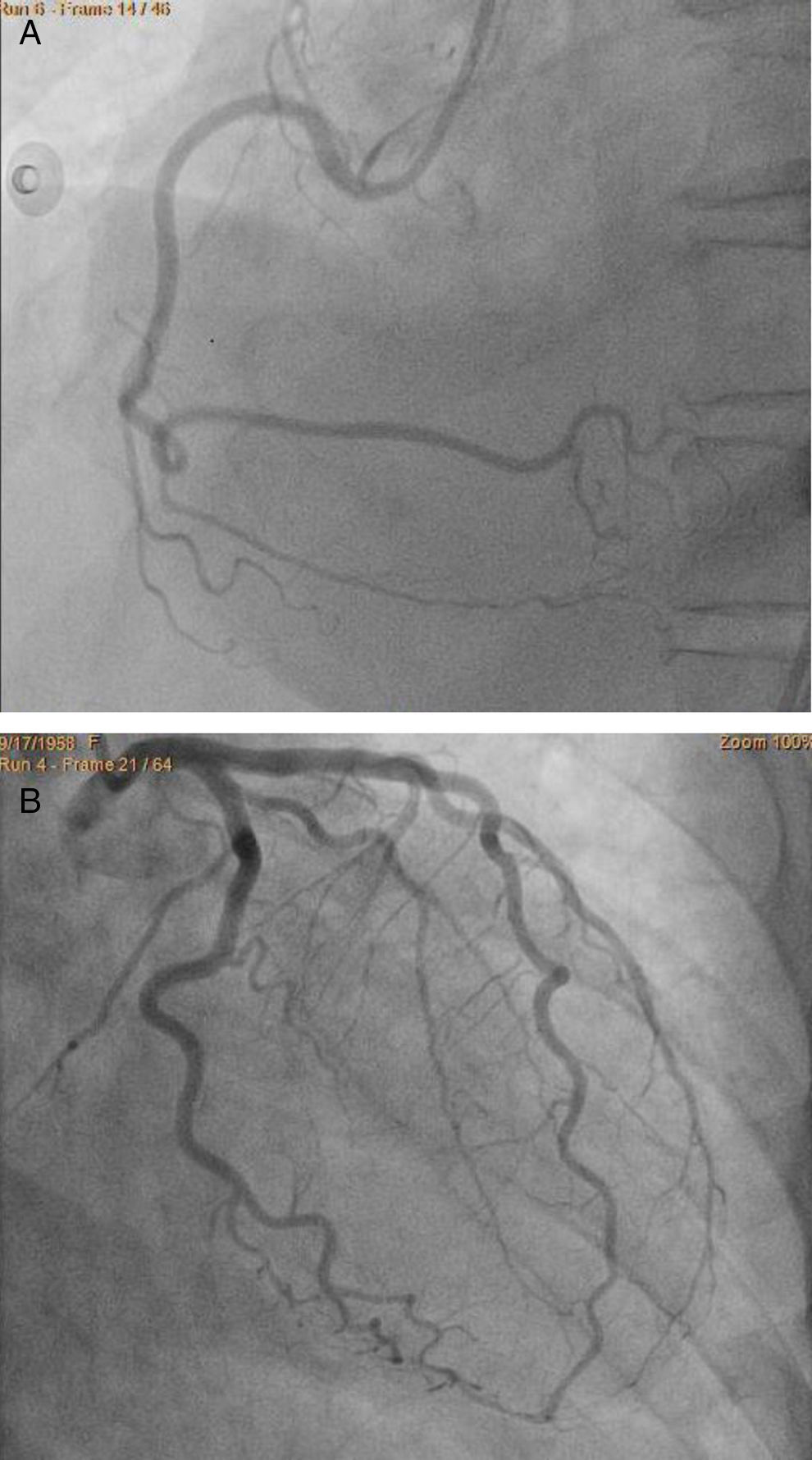
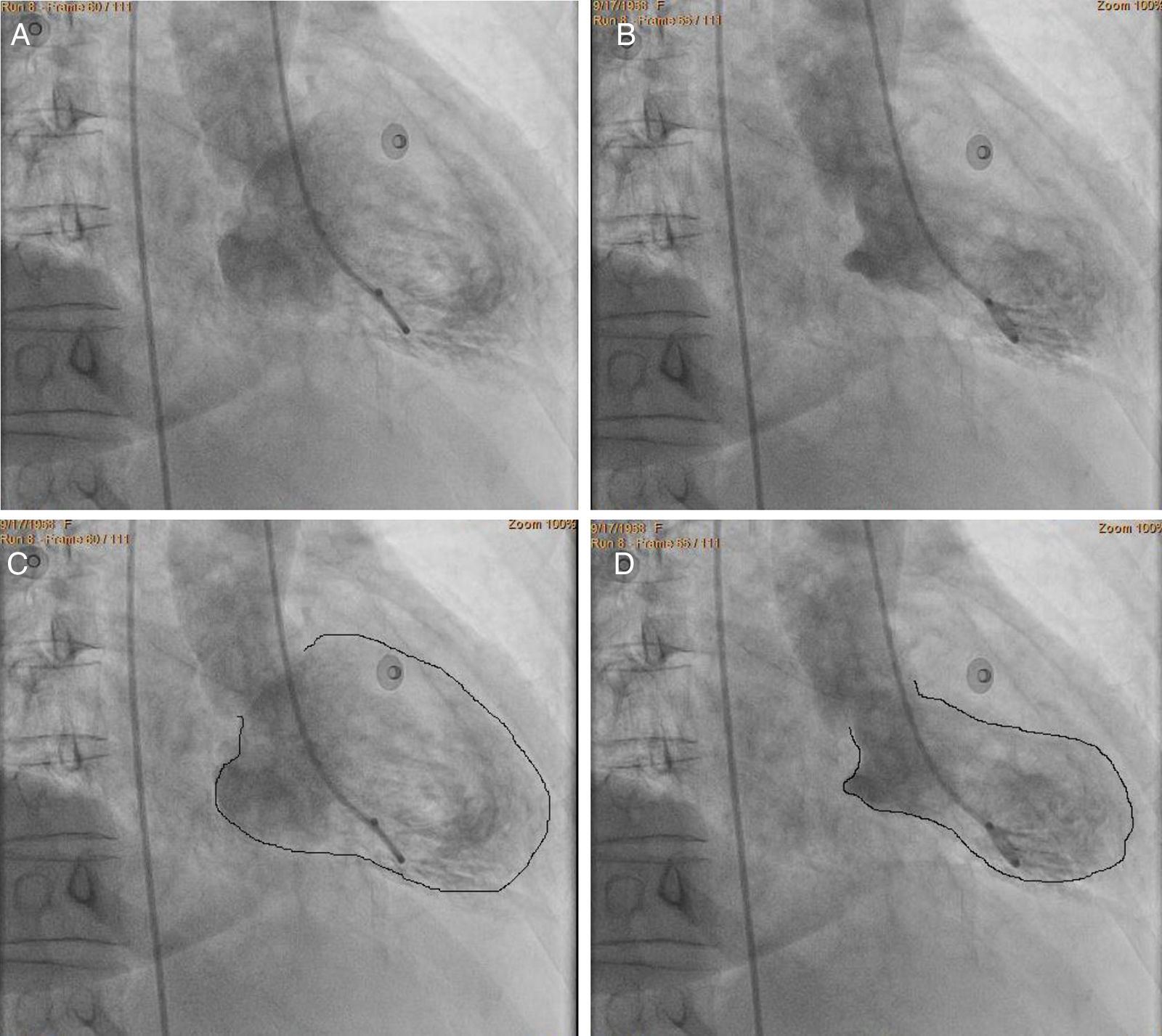
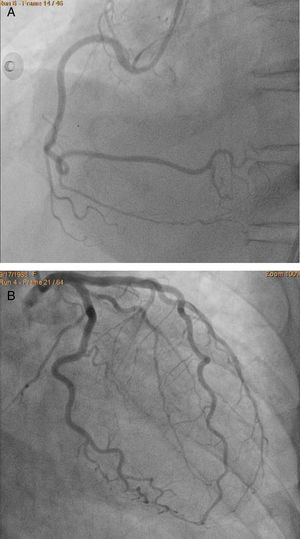
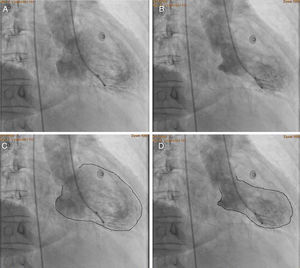
ST-segment elevation acute coronary syndrome was first considered and an invasive approaching was implemented. Cardiac catheterization showed no evidence of obstructive lesions in the coronary arteries (Fig. 2). The ventriculography showed an atypical pattern of myocardial contraction, with hypokinesis affecting the mid ventricular and apical segments; whereas the motion in the basal segments was spared (Fig. 3).
Ventriculography in RAO view showing motion abnormalities of the left ventricle. (A) end-diastole, (B) end-systole, (C) the same image seen in A but with enhanced endocardial border which shows normal cavity contours, and (D) the same image seen in B but with enhanced endocardial borders showing a pattern of apical ballooning, impaired mid-ventricular contractility and normal motion of the basal segments.
The following troponin serum levels were 2.9ng/ml and 1.3ng/ml, which were lower than those expected for the magnitude of ST segment elevation.
By means of a new anamnesis the patient referred that she had lost both of his parents in the last month. No other relevant data was gathered. Stress takotsubo cardiomyopathy was suspected and further research was warranted.
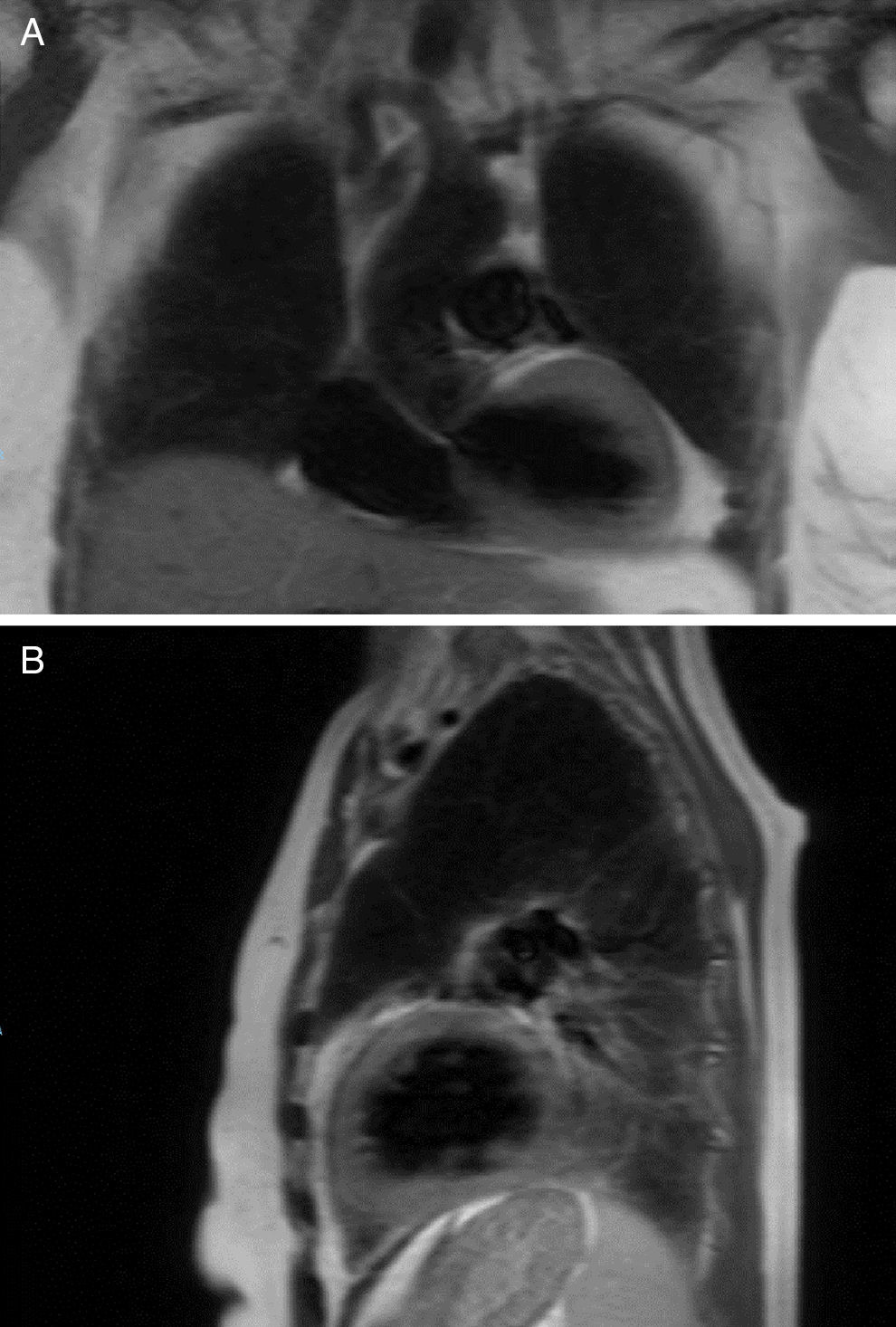
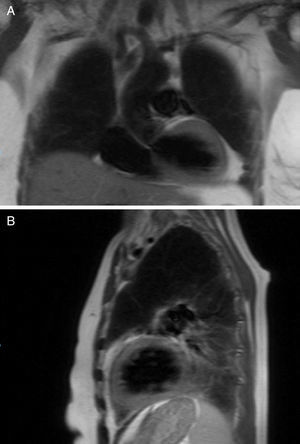
A T2 weighted cardiac magnetic resonance imaging (MRI) was performed to evaluate the presence of myocardial edema as a marker of an inflammatory process, no abnormalities suggestive of this entity were found (Fig. 4). A late gadolinium enhancement protocol was not performed because of the presence of acute renal failure. Normal urinary test with a negative determination of metanephrines and the absence of suprarenal masses on MRI helped us to reject the presence of pheochromocytoma. Takotsubo cardiomyopathy was diagnosed and evidence-based medical therapy implemented.
During hospitalization the patient had impairment of dyspnea and signs of congestive heart failure, serum determination of brain natriuretic peptide was 1205pg/mL (normal values <100pg/mL), creatinine levels was 1.9mg/dL. Low dose loop diuretic was administered with good clinical response. There was no need of use of inotropes.
Following ECG recordings showed progression from ST-segment elevation to symmetric T-wave inversion which was present now in all precordial leads (Fig. 1B).
DiscussionPatients with TC are most commonly postmenopausal women. In a systematic review, women accounted for 82–100% of patients with an average age of 62–75 years, although cases have been described in individuals aged 10–91 years.1 Accordingly to recent reports, this condition probably accounts for 1–2% of all cases of suspected acute myocardial infarction.2 However its true incidence is unknown, since out of Japan there have been relatively few reported cases. Till 2001 there had been reported just 2 TC cases in non-Japanese people.4 The first case reported in Mexico was in 2004 and then in 2011 two more cases were reported in just one year. Therefore it is suggested that a lack of awareness about the disease is one of the reasons of underdiagnosis.4,5
TC is considered to be among stress-related cardiomyopathies, which occur during times of enhanced sympathetic tone and can be precipitated by excessive endogenous or exogenous catecholamine stimulation of the myocardium, a condition that is also seen in cases of intracranial hemorrhage, ischemic stroke, head trauma, pheochromocytoma, and in critically ill patients.1 Several mechanisms have been implicated in its pathophysiology: multivessel epicardial coronary artery spasm, coronary microvascular impairment, direct catecholamine cardiotoxicity and neurogenic stunned myocardium, though none of them can wholly explain the wide expectrum of the disease.2 A different hypothesis is that high levels of circulating epinephrine trigger a switch in intracellular signal trafficking, from Gs (stimulating) protein to Gi (inhibitory) protein signaling through the β2 adrenoreceptor, producing a negatively inotropic effect that is greatest at the apical myocardium, in which the density of β-adrenoceptors is the highest.3 Overall, a catecholamine-implicated mechanism seem to be the one with the best background.1–10
The most frequent clinical symptoms of TC on admission are chest pain and dyspnea resembling acute myocardial infarction. Moreover, the ECG findings on admission often include ST elevation in precordial leads. Subsequent T-wave inversion and Q-wave formation also are frequently found. However coronary angiography, which is the best single tool to diagnose this condition, shows no flow-limiting lesions.2,3
There have been identified different morphological patterns of left ventricular (LV) affection, which includes: apical and mid-ventricular dysfunction, isolated mid-ventricular and basal dysfunction or isolated mid-ventricular dysfunction (apical-sparing), isolated basal dysfunction, global hypokinesis, and other non-coronary distribution wall motion abnormalities.1
Researchers at the Mayo Clinic proposed diagnostic criteria in 2004, which included: (1) transient akinesis or dyskinesis of the left apical and mid-ventricular segments with regional wall-motion abnormalities extending beyond a single epicardial vascular distribution, (2) absence of obstructive coronary disease or angiographic evidence of acute plaque rupture, (3) new electrocardiographic abnormalities (either ST-segment elevation and/or T-wave inversion) and (4) absence of all of the following: recent significant head trauma, intracranial bleeding, pheochromocytoma, obstructive epicardial coronary artery disease, myocarditis, and hypertrophic cardiomyopathy.6
However, evidence now indicates that coronary artery disease and TC can coexist, and takotsubo is particularly common in patients with pheochromocytoma or intracranial lesions.6 Accordingly 10% of patients with acute intracranial injury have acute ischemic electrocardiographic changes, the same clinical picture is seen in patients with elevated catecholamine levels secondary to pheochromocytomas.3
Mayo clinic criteria were modified in 2008, considering the next: (1) transient hypokinesis, akinesis, or dyskinesis in the left ventricular mid segments with or without apical involvement; (2) regional wall motion abnormalities that extend beyond a single epicardial vascular distribution; and frequently, but not always, a stressful trigger; the absence of obstructive coronary disease or angiographic evidence of acute plaque rupture; (3) new ECG abnormalities (ST-segment elevation and/or T-wave inversion) or modest elevation in cardiac troponin; and (4) the absence of pheochromocytoma and myocarditis. All four must be present to make the diagnosis.1–6
In these modified criteria, the presence of intracranial lesions no longer excludes patients from a TC diagnosis. However, patients are still excluded from receiving a TC diagnosis if pheochromocytoma or coronary artery disease is present.6
Since the first Mayo criteria were published in 2004, several groups have suggested their own diagnostic criteria, some of which have subsequently been refined: The 2007 Japanese Takotsubo Cardiomyopathy Study Group proposal, the 2011 Gothenburg criteria, the 2012 Johns Hopkins criteria, the 2013 revised Gothenburg criteria, and the 2014 Takotsubo Italian Network proposal are some them. However the 2008 modified Mayo clinic criteria remain the most widely used at present.6
The short-coming prognosis is well known but there is a paucity of data from large and prospectively identified patient cohorts studied for extended periods of time following the initial event.7,8
Although not a common pattern, the right ventricle (RV) is also affected in some patients, being the most frequently affected segments: the apico-lateral, the antero-lateral, and the inferior segment; with all right ventricular wall-motion abnormalities showing improvement or disappearing in the patients who underwent a follow-up cardiac MRI study. LV ejection fraction was significantly lower in the cases with RV affection, as well as pleural effusion was more common in patients with RV involvement.9
Right and/or left ventricular thrombi and embolic events have been identified in some patients (predominantly by cardiac MRI). It has been reported that all-cause mortality during follow-up exceeds a matched general population with most deaths occurring in the first year. Nonfatal recurrent stress cardiomyopathy events have been also reported.7
Emotional triggers have been found to be not as common as physical triggers. Moreover in some patients no evident trigger has been found. However patients with TC have been found to have higher prevalence of neurologic or psychiatric disorders than those with an acute coronary syndrome.8
The best imaging study to make the diagnosis of TC is cardiac catheterization, however cardiac MRI allows complete anatomical information and may help to distinguish TC from other acute cardiac syndromes. Many recent studies have reported that the number of patients with mid-ventricular dysfunction is increased compared with the initial description of the disease. The atypical presentation with apical sparing and affection only in the basal segments is not rare.2,3,10
Cardiac MRI imaging helps in excluding the differential diagnoses of myocarditis or aborted myocardial infarction, and defining the ventricular abnormalities in patients with poor echogenicity, while nuclear cardiac imaging is useful for the detection of viable myocardium and the functional abnormalities.10
There are no specific treatments for the left ventricular failure of TC because cardiac function is normalized within a few weeks. The use of long-term adrenoceptor blocker therapy seems rational to prevent recurrence, although its use in the acute phase of TC is still a matter of debate. Treatment with a combined alpha and beta blocker seems rational, so as we do not leave alfa-activity with an unopposed effect, favoring vasoconstriction. However beta-blocking drugs not always have provided absolute protection against recurrent events.1,2,7
Hypotension after the initiation of an angiotensin-converting enzyme inhibitor, angiotensin receptor blocker, or diuretics has been reported as a result of potentiation of a dynamic LV outflow tract obstruction. A short duration of anticoagulation with warfarin may be considered for patients with persistent, significant reduction in LV function to prevent LV thrombus formation and embolization.1,7 The use of angiotensin-converting-enzyme inhibitors or angiotensin-receptor blockers has been associated with improved survival at 1 year.8 Treatment with a catecholamine is usually not indicated since sympathetic activation is believed to be the basis of the pathogenesis of TC. Intraaortic balloon pump is useful when shock occurs.1,2
The prognosis of patients with TC is generally favorable1,10; however some complications such as pulmonary edema, intraventricular pressure gradients, acute mitral regurgitation, right ventricular involvement with pleural effusion, intraventricular thrombi resulting in stroke or arterial embolism, atrial fibrillation, malignant ventricular arrhythmias, and cardiogenic shock and left ventricular free wall rupture can occur. Heart failure, with or without pulmonary edema, is the most common clinical complication. In-hospital mortality ranges between 1 and 2% of patients2,10
The recurrence rate has been suggested to be in the range of 2–10% in the first few years after the presentation of TC. Recurrence rates may be lower if adrenergic blockade is maintained, assuming the central role of catecholamines in the pathogenesis of the syndrome.1
In the case of our patient, a takotsubo stress cardiomyopathy was diagnosed, after having found: apical and mid-ventricular hypokinesis with sparing of the basal segments; abnormal left ventricular wall motion affecting more than one epicardial coronary artery distribution, with normal coronary arteries on angiography, and an identified stressor factor; new ECG alterations accompanied by a modest increment of troponin I serum levels; and absence of myocarditis and pheochromocytoma as documented by cardiac MRI and urinary metanephrines respectively. All of the four modified Mayo clinic criteria were satisfied.
Acute coronary syndrome pharmacologic treatment as per guidelines was implemented, although cardiac MRI did not show evidence of intracavitary thrombus formation, treatment included parenteral anticoagulation till hospital discharge. There was precaution with the use of beta-blockers (BB) and angiotensin-converting-enzyme inhibitors (ACEI). The first dose of oral beta-blocker carvedilol, which has an alpha and beta-adrenergic suppression in a 1:1 relationship; and ACEI were started on the fifth day of the initiation of symptoms, once we considered there was a low risk of mechanical and hemodynamic complications. A good clinical response was observed to implemented treatment for heart failure and hospital discharge was possible on the seventh day of initiation of symptoms.
Ethical disclosureProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThere is no conflict of interests.