The tympanic membrane perforation is generally caused by infection or trauma. It is a condition that can cause hearing loss; its incidence varies between 1 and 3% of the population in the United States, and even less than 1% in the world population.
ObjectiveThis study is to conduct a pilot test in which the effectiveness of conservative treatment was measured and compared by applying phenytoin or platelet-rich plasma to close tympanic perforations and the healing period of the same.
Patients and methodsTen patients were included and all of them fulfilled the selection criteria: Age over five years-old, indiscriminate sex with a diagnosis of perforated eardrum, eardrum perforation between 30 and 60% and presence of tympanic remnant; and no previous surgical treatment. Elimination criteria were those patients with marginal eardrum perforations, patients who were not on antiplatelet drugs or anticoagulants, poor response to platelet-rich plasma after 6 weeks, patients with known autoimmune, active neoplastic, atopic otic conditions and those currently under immunosuppressive treatments. Participants were randomized into two groups according to treatment: phenytoin (0.2mg) or platelet-rich plasma (0.2–0.5cc).
ResultsTen patients with unilateral tympanic perforation were recorded whose average age was 26.9±14.9 years; the sex distribution was 1.5:1 male predominance. In treatment A, the average closing time was 3.8±0.836 weeks; meanwhile, in the treatment B the closure time was 5.2±0.836 weeks.
La perforación de la membrana timpánica generalmente es producida por alguna infección o traumatismo; es un padecimiento que puede causar hipoacusia, y su incidencia oscila entre el 1 y 3% de la población en los Estados Unidos, siendo aún menor al 1% en la población mundial.
ObjetivoSe realizó una prueba piloto en la cual se midió y comparó la eficacia del tratamiento mediante la aplicación de difenilhidantoína o plasma rico en plaquetas para el cierre de perforaciones timpánicas y el tiempo de reparación de la misma.
Pacientes y MétodosSe incluyeron diez pacientes quienes cumplieron los criterios de selección: Edad mayor a 5 años, sexo indistinto, diagnóstico de perforación timpánica entre 30-60%; presencia de remanente timpánico sin tratamiento quirúrgico previo. Criterios de eliminación: perforaciones marginales de tímpano, pacientes con terapia anticoagulante o anti-agregante e inmunosupresora; pobre respuesta al tratamiento tras 6 semanas. Asimismo, pacientes con historial de procesos autoinmunes, neoplásicos o atópicos.
ResultadosSe obtuvieron diez pacientes con perforación unilateral, con edad promedio de 26.9±14.9 años y proporción de 1.5:1, con predominio masculino. En el tratamiento A, el tiempo promedio de cierre fue 3.8±0.836 semanas; mientras que, en el tratamiento B, el tiempo de cierre fue 5.2±0.836 semanas.
Generally, the tympanic membrane perforations (TMP) are produced by severe infections or traumatisms. It is a condition that can cause hearing loss, and its incidence varies between 1 and 3% of the population in the United States, and even less than 1% in the world population. However in Mexico there is no clear data for this condition.1,2
Most (78.7%) of the TMP heal spontaneously over a period of 7–10 days with few functional consequences, but the risk of failure of spontaneous curing results in very factual persistent perforation.1–4
One factor influencing to chronicity (over three months) of the TMP is the persistent infection; other factors related to this phenomenon include the nutritional and immune status of the individual, shape and dimensions of the perforation; and therefore prior application of the topical agents, mostly corticoesteroids.1,3,5
Regeneration of the tympanic membrane, after perforation, is a complex biological process involving epithelial proliferation and migration, with fibroblast proliferation and angiogenesis which finally ends with the remodeling of the tissue.6,7
After three to six weeks of presentation, surgical management must be considered; in the experimental field, a perforation is considered chronic when its development time ranges from eight to fifteen weeks.5,6
In Mexico there is no protocol for conservative treatment of tympanic perforations, the therapeutic method of choice is surgery, where tympanoplasty with autogenous connective tissue is the treatment of choice in most cases, due to the demonstration of high success rates (88–95%).7,8
Before 1950, the usage of surgical treatment for tympanic membrane perforation was focused to eliminate the cause, but any reconstructive action or procedure was not planned. In 1952, Wullstein made the first description of a new functional procedure using grafting materials such as fascia, perichondrium, periosteum, vein, dura mater and cartilage. However, was Zöllner who popularized and established the principles for this technique in 1955; but due to the disadvantages of tympanoplasty (general anesthesia, longer postoperative rest time, limitation of the normal activities for the patient, making incisions to expand the surgical exposure) a less abrasive approach is sought.1,3,9
Nowadays, thanks to advances in microsurgical technology and the implantation of prosthetic ossicular counterparts, the procedure has suffered important changes; many authors agree that a satisfactory approach for tympanic perforations treatment would be the administration of a topical and bio-absorbable agents, which favor the closure, by the disruption of the epithelial edge of the perforation with no side-effects and an ambulatory way of placement, without requiring further intervention.8
According to Garzón-Arruel et al.10 there are a wide variety of techniques to prevent removal of the squamous epithelium and trigger a reparative fibroblastic reaction in the middle fibrous layer of the tympanic membrane, including chemical (phenytoin, vitamin c, trichloroacetic acid, etc.), mechanical and suspension of “physiological” characteristics (superficial temporal fascia, amniotic membrane, bovine collagen, etc.)
The procedures associated with bio-absorbable agents (paper patches, absorbable gelatin film, hyaluronic acid, etc.) favor its closure without the complications related to surgery; however, some are still being studied (autologous serum enriched with growth factors).11 One of the advantages associated with these new methods for closing the persistent TMP is, profuse microsurgical skills are not required by the treating physician and can be used on an outpatient basis through consultations.8
Phenytoin (DFH) was introduced in 1937 for the control of seizures, is an anticonvulsant drug with chemical structure similar to that of barbiturates, has resulted in gingival hyperplasia as a side effect; it is widely used as a conservative treatment applying powder directly to the wounds to promote healing, especially stimulates the vascular healing of ulcers in patients with diabetes, or leprosy under increased granulation tissue by direct stimulus on fibroblastic-genesis and consequent formation of epithelium; however, studies about its effect on tympanic membrane perforations are rare.3,12–14
The fibroblasts originated from hyperplasia induced by using DFH, show increased synthesis of sulfated glucosamine glycans. In turn, inhibit collagenase and stimulate expression of growth factor derived keratinocytes.3 It has a limited use due to side effects that have been associated with it, primarily in the central nervous system. Also, its use is related to cardiotoxicity, nausea, vomiting and liver damage when administered systemically. Currently, there are no studies or reports in the medical literature that talk about the side effects by topical application.5
The high concentration of various trophic factors contained in platelets granules, have led to suggestions that the application of platelet-rich plasma (PRP) in the treatment of skin ulcers, because of the ability of protein synthesis and as a modulator of inflammation, which favors cell proliferation and synthesis of extracellular matrix, promoting cicatrization.15 It is precisely these functions in addition to their antimicrobial activity, which have led to propose the use of autologous PRP as a better alternative for the repair and regeneration of various tissues.11,16
The aim of this study was to conduct a pilot test in which the effectiveness of treatment compared by applying phenytoin or platelet-rich plasma to close tympanic perforations and the healing period of the same.
Patients and methodsTen patients were included and all of them fulfilled the selection criteria: Age over five years, indiscriminate sex, diagnosis of perforated eardrum between 30 and 60%, presence of tympanic remnant and no previous surgical treatment.
Elimination criteria were those patients with: cholesteatoma, upper respiratory tract infection, marginal eardrum perforations, patients on antiplatelet drugs and anticoagulants not related to their ear disease and poor response to platelet-rich plasma after 6 weeks of treatment, autoimmune disorders, active neoplastic and atopic otic conditions, and those currently under immunosuppressive treatment. Patients were assigned randomly to treatment, where two groups of similar features were selected.
In each patient, ear canal cleaning was performed prior to the application of topical tetracaine (6 drops). After 20min the ear canal was cleaned again using cotton and mechanical revival of the edges of the perforation with a otic sickle knife until bleeding was noted and approximately 0.2mg of diphenylhydantoin powder (treatment A) or 0.2–0.5cc of autologous plasma rich in platelets (treatment B) was applied using a hyssop or an insulin syringe, according to the study group.
Finally, rice paper and gelfoam® was placed on the perforation site as synthetic material for wound closure, also a cotton ball is sited to avoid the exit and the exposure of the medication. The patients underwent weekly monitoring by otoscopy and tympanometry in each case; there was no use or analgesic, antihistaminic or antibiotic after both maneuvers.
Platelet-rich plasma, is obtained by extracting 10cc of peripheral blood, via venipuncture, without any anticoagulant; which is then centrifuged at 1200 rpm and 2000 rpm at room temperature for 10 and 7min respectively. In the second centrifugation (2000 rpm) a clot with fibrin of greater density was isolated and then applied on the eardrum edges using a sterilized insulin syringe.
Meanwhile, for patients with phenytoin treatment, due there is no formulation for topical application, the drug should be obtained from pulverized tablet or capsule contents (100mg) and combined with an inert oily base for application.
Statistical analysisDescriptive statistic was used in order to show demographics features and non-parametric statistical analysis was applied to hypothesis test (χ2). Output results were considered as closure or non-closure, so was a dichotomy variable. Time of closure was evaluated with t-paired test.
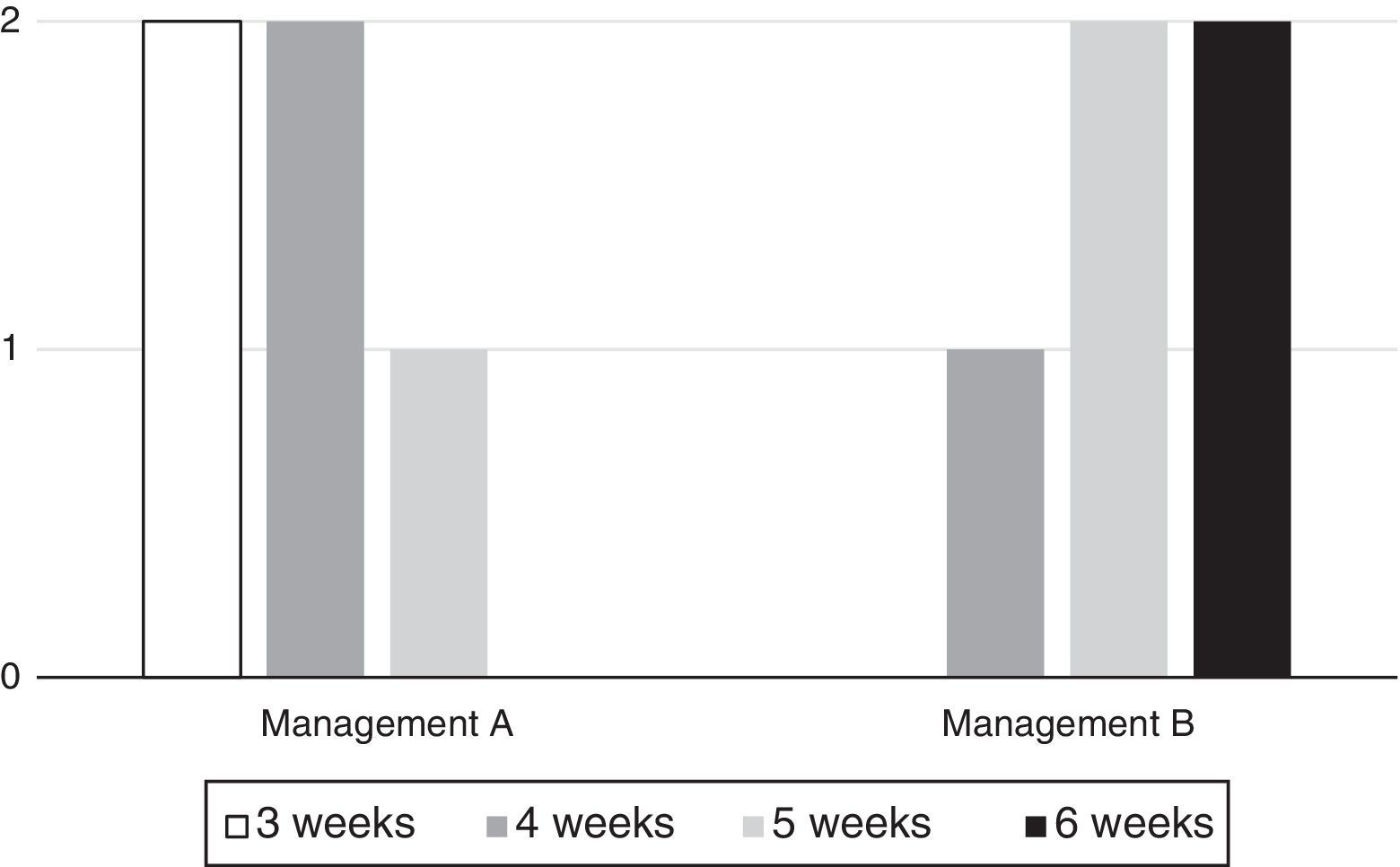
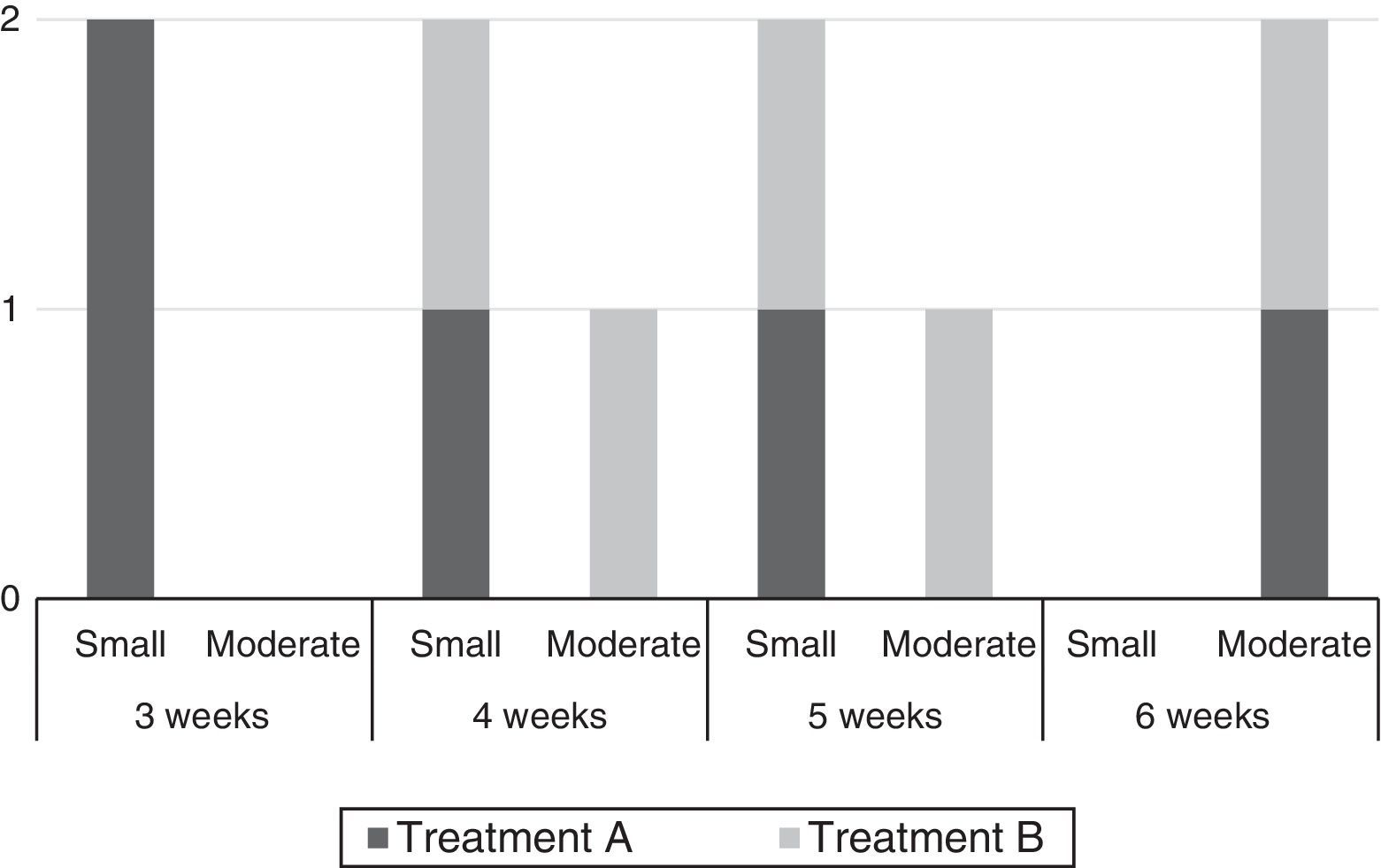
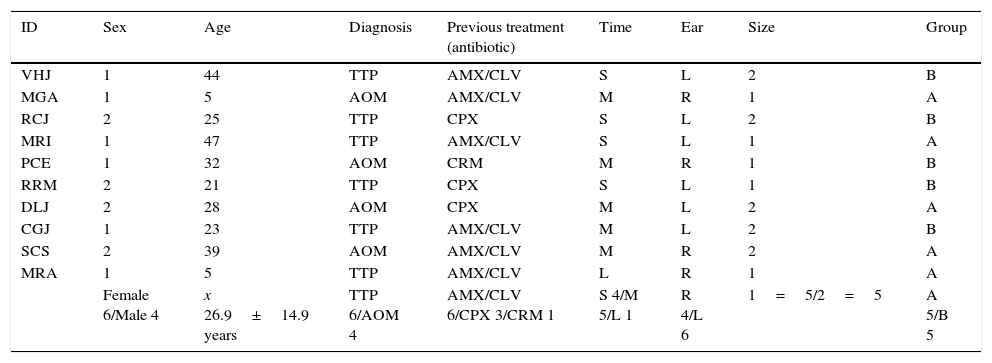
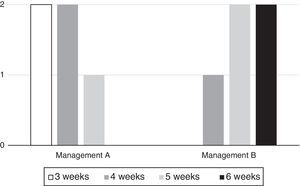
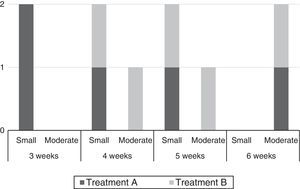
ResultsTen patients with unilateral tympanic perforation were recorded (Tables 1 and 2) whose average age was 26.9±14.9 (SD) years; the sex distribution was 1.5:1 male predominance. Six patients had previous treatment with amoxicillin/clavulanate, 3 with ciprofloxacin and 1 with clarithromycin. In general, were four small sized perforations (one quadrant or less of the total area of the tympanic membrane) and six of moderate size (covering two quadrants of the tympanic membrane); the curative rate was 100% at six weeks (Figs. 1 and 2).
Demographic table with sex men (1) women (2). Antibiotic treatment: amoxicillin/clavulanate (AMX/CLV), ciprofloxacin (CPX) and clarithromycin (CRM). Evolution period: 1–20 days (S), 20–40 days (M) and 40–60 days (L). Affected ear: right (R) or left (L). Perforation size: small (1) or medium (2); and treatment group: diphenylhydantoin (A) or platelet-rich-plasma (B).
| ID | Sex | Age | Diagnosis | Previous treatment (antibiotic) | Time | Ear | Size | Group |
|---|---|---|---|---|---|---|---|---|
| VHJ | 1 | 44 | TTP | AMX/CLV | S | L | 2 | B |
| MGA | 1 | 5 | AOM | AMX/CLV | M | R | 1 | A |
| RCJ | 2 | 25 | TTP | CPX | S | L | 2 | B |
| MRI | 1 | 47 | TTP | AMX/CLV | S | L | 1 | A |
| PCE | 1 | 32 | AOM | CRM | M | R | 1 | B |
| RRM | 2 | 21 | TTP | CPX | S | L | 1 | B |
| DLJ | 2 | 28 | AOM | CPX | M | L | 2 | A |
| CGJ | 1 | 23 | TTP | AMX/CLV | M | L | 2 | B |
| SCS | 2 | 39 | AOM | AMX/CLV | M | R | 2 | A |
| MRA | 1 | 5 | TTP | AMX/CLV | L | R | 1 | A |
| Female 6/Male 4 | x 26.9±14.9 years | TTP 6/AOM 4 | AMX/CLV 6/CPX 3/CRM 1 | S 4/M 5/L 1 | R 4/L 6 | 1=5/2=5 | A 5/B 5 |
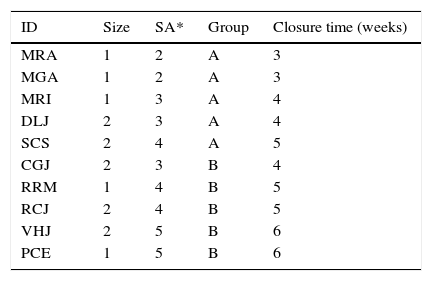
Group A shows that the shortest period of closure was 3 weeks, meanwhile in group B was 4 weeks; in general the closing result was obtained in longer period in group B, but if we compare the statistical mode of both groups, the greater perforation size is noted in group B. Non statistical difference was observed with χ2 (p=0.527).
| ID | Size | SA* | Group | Closure time (weeks) |
|---|---|---|---|---|
| MRA | 1 | 2 | A | 3 |
| MGA | 1 | 2 | A | 3 |
| MRI | 1 | 3 | A | 4 |
| DLJ | 2 | 3 | A | 4 |
| SCS | 2 | 4 | A | 5 |
| CGJ | 2 | 3 | B | 4 |
| RRM | 1 | 4 | B | 5 |
| RCJ | 2 | 4 | B | 5 |
| VHJ | 2 | 5 | B | 6 |
| PCE | 1 | 5 | B | 6 |
SA*: surgical abrasion.
Graphics shows the distribution for both treatment groups in relation to the closure time expressed in weeks. As in Table 2, it is possible to observe that there is no appropriate closure time with treatment B until the 4 week.
In the treatment A, five patients were recorded with a mean age of 24.8±19.2 (SD) years; three of whom were diagnosed with tympanic perforation secondary to acute otitis media and two were of post- traumatic origin. The most frequent time of evolution of perforation was 35 days (range 20–40) and 60% of patients had a small perforation size. The rest of the cases were of moderate type. The average closing time in this group was 3.8±0.836 (SD) weeks.
Meanwhile, the treatment B included five patients whose average age was 29±9.354 years and 80% had traumatic eardrum perforation, the rest was of post-infectious etiology. The perforation time was of 20 days (range 20–40) and the closure time was 5.2±0.836 (SD) weeks. Also, the predominant size of the perforation was the smaller size (60%).
Both the groups were performed tympanometry at the end of the study; normal hearing curve was obtained from each patient, for which motive the “functional” closure of the perforation in each of these patients was confirmed. No adverse effects and complications were presented in any case.
The treatment results showed that the effect of PRP in treating moderate-sized perforations was significantly superior to that in treating small-sized perforations. Namely, the smaller perforations of tympanic membrane were, the easier the wounds healed by phenytoin.
DiscussionThe purpose of this study was to clarify the effectiveness of conservative treatment by applying DPH or PRP; where both therapeutic options proved excellent therapeutic options for closing tympanic perforations due to favorable increased number of fibroblasts, collagen synthesis, and new blood vessels. Similarly microbicides and modulating actions promote inflammation, inducing cell proliferation; for which they accomplish the repair of wounds and other tissue damage. The results of this study did not show difference between both treatments in a short period time of monitoring; both options demonstrated be suitable for repairing small and middle sized tympanic membrane perforation. The curative effects are satisfying without complications and there was also direct influence induced by the lesion size for early closure.
The effects of topical application of phenytoin for repairing eardrum perforations in 6 experimental animal models (white rabbits) informed by Kuran et al.17 were no satisfactory; in their trial do not found any difference when compared to isotonic saline for traumatic tympanic membrane perforation in terms of inflammation, vascularization and fibroblastic reaction under histological examination; but they results may differ from many other studies.
The results exposed in the study conducted by Taboada-Saavedra et al.3 showed the closure of 90% of study subjects after one week of 12.5mg of phenytoin application and 100% of success rate with 50mg as dose in same conditions.
In our study, the effectiveness of phenytoin for healing TMP was evident due the chronic features of the condition in every patient, in where the evolution range were between 20 and 40 days and was not previous spontaneous closure.
Alvaro Navarrete et al.18 in their pilot study assessed three patients with an inactive central perforated eardrum. They used PRP to close the perforation without elevating annulus or entering the middle ear. According to the results the PRP allowed successful closure in these patients, but they did not report any functional recovery nor time of exposure to the topical agent.
We obtained similar results as Saynes-Marín,19 who showed a success rate of closure about 88.5% after 6 week of follow up with functional improvement in 24 patients (70%) and were not reported side-effects or hearing loss using PRP as treatment. In our trial were 100% success rate at week six with no complications Also, Garin et al.20 informed functional results between 3 and 6 weeks after the application of platelet-rich fibrin comparing the audiometry performed within 2 weeks prior to the procedure and after it.
Erkilet et al.21 conducted a perforation in the tympanic membrane of 44 rats, they found that the PRP was effective in accelerating closure of the perforation with a statical significance on days three and seven after histopathological evaluation of tympanic membrane perforation healing.
ConclusionDespite the limitations presented by this study, due to its low sample, it was shown that in all patients who suffered tympanic membrane perforation closure of the injury is achieved, regardless of age or etiology; however, it is possible to infer that age is a predicting factor of the early closure of the injury, this is due to the intrinsic ability of each organism to healing, where at an early age there are many pro-inflammatory components and triggers the coagulation cascade being positive modulators for closure.
It is recommended that phenytoin and platelet rich plasma as topical treatment options for closing tympanic membrane, and the closure time was similar for both.
Ethical disclosureProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors declare that they have no conflict of interests.