Subjects with Down syndrome present hypotonia, stomatognathic alteration system, such as small oral cavity, macroglossia and malocclusions, may suggest a higher risk for temporomandibular disorders.
AimTo evaluate the temporomandibular joint of Down syndrome subjects with, to verify temporomandibular disorders prevalence and possible postural associations.
Material and methodsForty subjects was included in this study. Temporomandibular joint was evaluated across functional physical screening and questions about daily habits. After, the subjects was submitted a postural evaluation through photographic registers in front of a crisscross space.
ResultsMost subjects was presented temporomandibular disorders (77.5%). The most common signs and symptoms found were bite alterations and parafunctional habits. Moreover, parafunctional habits and pain were positively correlated to temporomandibular disorder in these subjects (p=0.038 and p=0.016 respectively). Postural alterations were not significant correlation with temporomandibular disorder.
ConclusionsTo verified a high prevalence of temporomandibular disorder and important relationship between parafunctional habits and pain in subjects with Down syndrome.
Los sujetos con síndrome de Down (SD), presentan hipotonía, disfunciones en el sistema stomatognático, como cavidad oral disminuida, macroglosia y maloclusiones, aumentando la prevalencia de desórdenes temporomandibulares.
ObjetivoEvaluar la articulación temporomandibular de sujetos con SD, a fin de verificar la prevalencia de desórdenes temporomandibulares y posibles relaciones con la postura.
MétodosCuarenta individuos con SD se incluyeron en este estudio. La articulación temporomandibular fue evaluada a través de examen físico funcional y preguntas sobre os hábitos diarios de cada participante. Posteriormente, los sujetos fueran fotograbados delante de un posturógrafo y sus posturas evaluadas.
ResultadosLa mayoría de los participantes presentó disfunción de la articulación temporomandibular (77,5%). Los signos y síntomas más frecuentes fueran alteración en el tipo de mordida y hábitos parafuncionales, con una correlación significativa con la presencia de disfunción temporomandibular (p=0.038). Todos los participantes que manifestaban dolor presentaban disfunción articular (p=0.016). Las alteraciones posturales encontradas no tuvieran correlación con la presencia de disfunción temporomandibular.
ConclusiónSe observó una alta prevalencia de disfunción temporomandibular en los individuos evaluados y una importante relación entre la disfunción y la presencia de hábitos parafuncionales y dor en sujetos con SD.
Down syndrome (DS) is a genetic alteration caused by a trisomy of the chromosome 21.1–3 Individuals with DS present specific motor disorders, such as generalized muscular hypotonia and hypermobility joint. Moreover, DS subjects also present stomatognathic modifications system, such as small oral cavity and relative macroglossia mainly due to incorrect anterior tongue position and malocclusions.2 These characteristics may suggest a higher risk for temporomandibular disorders (TMD).1
TMD is characterized by functional and structural changes of stomatognathic system, the most frequent symptoms being temporomandibular joint (TMJ) and/or masticatory muscles pain (among others), and parafunctional habits such as bruxism,4 which is a common condition in subjects with DS.1,2 Interestingly, postural alterations are also frequently described in individuals with TMD, mainly related to the head, cervical spine, shoulder posture.1,5
The early diagnosis of postural alterations or TMJ could help on the treatment or TMD prevention. However, to date studies which studied the relationship among DS morphophysiological changes and the prevalence of TMD in this population are still incipient. Therefore, the aim of this study was to evaluate the TMJ of DS subjects with, to verify TMD prevalence and possible postural associations.
MethodsParticipantsForty participants were recruited for a DS specialized institution, localized in Porto Alegre-RS, Brazil. The inclusion criteria for this study were: (1) aged between 10 and 60 years old; (2) ability to stand up for at least 60min; and (3) a responsible companion during the measurements. Participants with neurological disorders that could interfere in the evaluations were excluded.
In order to make de homogeneous sample, the subjects were divided by age in three different groups: (1) aged between 10 and 19 years old, (2) aged between 20 and 29 years old and, (3) aged ≥30 years.
After a meeting to explain the study objectives and methods, a written inform consent was signed by a responsible. The study was approved by the research ethics committee of the Centro Universitário Metodista – IPA.
AssessmentsThe assessments were performed in a single day. Prior to the initial examination, a full historical examination was perform to identify: (1) past medical history of subjects, (2) episodes of TMJ pain, (3) parafunctional habits such as bruxism, continuous gum chewing, and nail biting, or chewing on writing implements (pencils, pens).
After, a physical therapist and a dentist realized a TMJ functional physical screening. The dentition, chewing, type of bite, tongue, craniofacial profile, TMJ range of motion, opening and closing mouth (whit or without deviation), pain through muscle palpation in the relevant muscles to TMJ and presence of TMJ bias were examined according to previous literature.6 The participants were also submitted a postural evaluation through photographic registers for posterior analysis by a physical therapist. The patients were positioned in front of a crisscross space according to Souza et al.7
Statistical analysesThe Statistical Package for Social Sciences for Windows (SPSS, version 17.0, Chicago, IL, USA) was used for data analysis. Data were analyzed using descriptive statistics and were tested to compare independent group means. The non-parametric Chi-square test and Fisher's exact test were applied to compare dichotomic categorical data. The Student t test was used to compare the TMD among genders, and the Person's correlation coefficient was applied for correlation between TMD and the other parameters. An alpha level of 5% (p<0.05) was considered as significant.
ResultsThe sample was divided in three groups according to age, (group 1) was composed by 11 subjects, seven men and three women (14.3±2.8 years old), (group 2) was constituted by 14 subjects, among this 11 men and three women (24±2.4 years old), and (group 3) was composed by 15 subjects, among this seven men and eight women (37.9±8.8 years old).
Considering that no differences among groups or gender were found on the measured parameters, male and female were included in the same groups.
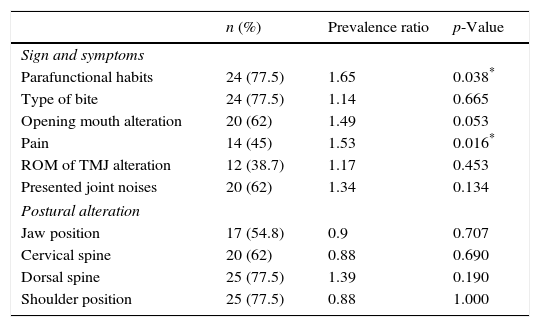
The TMD was found in 31 subjects (77.5%), and the most common signs and symptoms found were: (1) bite alterations on 24 subjects (77.5%), with anterior open bite as the most prevalent (50%), and (2) parafunctional habits presented on 24 participants (77.5%) with bruxism 17 (40.8%) and nail biting 11 (26.4%) as the most common descriptions, as presented on Table 1. Moreover, parafunctional habits and pain were positively correlated to TMD in these subjects.
Correlations of temporomandibular disorders parameters (n=31).
| n (%) | Prevalence ratio | p-Value | |
|---|---|---|---|
| Sign and symptoms | |||
| Parafunctional habits | 24 (77.5) | 1.65 | 0.038* |
| Type of bite | 24 (77.5) | 1.14 | 0.665 |
| Opening mouth alteration | 20 (62) | 1.49 | 0.053 |
| Pain | 14 (45) | 1.53 | 0.016* |
| ROM of TMJ alteration | 12 (38.7) | 1.17 | 0.453 |
| Presented joint noises | 20 (62) | 1.34 | 0.134 |
| Postural alteration | |||
| Jaw position | 17 (54.8) | 0.9 | 0.707 |
| Cervical spine | 20 (62) | 0.88 | 0.690 |
| Dorsal spine | 25 (77.5) | 1.39 | 0.190 |
| Shoulder position | 25 (77.5) | 0.88 | 1.000 |
n, subjects number; (%), percent; p, significance level; ROM, range of motion; TMJ, temporomandibular joint.
Similarly to the total sample, no differences among gender and age were found for TMD. Regarding the posture, most of the TMD patients showed changes in the jaw positioning (54.8%). The prognathic craniofacial profile was most prevalent (46.5%). In addition, these patients showed changes in the cervical spine (62%) among hiperlordosis were most prevalent (48.6%). Dorsal spine alterations was presented by 77.5% subjects with TMD, among hipercifosis was most common (88%). Regarding to shoulders positioning, 77.5% participants presented alteration and shoulder protrusion was most common (92%), as seen on Table 1.
DiscussionThe aim of this study was to evaluate TMJ of DS subjects in order to verify the TMD's prevalence. Most of the participant subjects presented TMD, probably related to the hypotonic, hyper flexibility and laxity joint1 that characterizes DS.
Signs and symptoms associated with TMD can include TMJ pain, decreased jaw mobility, joint noises (clicking, crepitus), headaches, otalgia, inability to fully open and close the mouth.4,6 In a study with 4528 TMJ patients, pain was frequently reported (96.1%).8 Also, compromised mandibular movements, sounds and dental changes probably due to parafunctional habits, often accompanied pain.8 In our study similar results were found. The type of bite alteration and parafunctional habits were the most frequent signs and symptoms among DS subjects, and all the subjects with pain presented TMD, corroborating with previous studies.4,6,8
Studies including child and teenagers without DS verified the relation of parafunctional habits, such as bruxism, with related TMD pain.9,10 In the present study, bruxism was the most prevalent parafunctional habit. According to Macho et al., this parafunctional habit is common in subjects with DS throughout life, increasing the incidence in anxiety, malocclusions and TMD.1
Malocclusions generally result from the complex interaction of many factors. In subjects with DS could be explain by abnormal posture and function of tongue to interfere the eruption of the teeth enough to cause anterior open bite and influence the shape of the dental arch and the position of the teeth, this is often related to hypotonia.11 Moreover, malocclusions could be associated with abnormal posture.12
Therefore, postural assessment of patients with TMD is most important, whereas the jaw position is directly related with cervical spine posture and shoulders position.12
Hence, a TMD results in head position alterations on, that compromises jaw position. Thus, jaw alterations promote hyperactivity on chewing and cervical spine muscles. Consequently, changes on shoulder muscles are followed, resulting in postural alterations for neck, shoulders, and head adjustments in cases of mandibular retrognathism or prognathism.12,13 Although no correlation between postural changes and TMD was found in the present study, most of the DS subjects presented mandibular prognathism, shoulder protusion, cervical hyperlordosis, and dorsal hyperkyphosis, corroborating previous studies.14
LimitationsThe limitations of this study must be taken into account when analyzing the results. First, the sample size, which consisted of 40 participants, can be considered a small sample. Second, the absence a control group, maybe if possible a strong correlation. Third, the evaluation should be realized through specific posture evaluation software. Finally, was the lack of studies relating TMJ, TDM and posture in subjects with DS. However, we find important and relevant dates about physical and orthopedics characteristics in this population.
ConclusionsIn this study, we a high prevalence of TMD in subjects with DS was verified, as well as some relevant postural alterations related with TMD.
Highlight the importance of more researches in this area, since this subjects have specific muscles features, needing postural corrections. Thus it most important inclusion the global postural reeducation on multidisciplinary treatment of patients, not only the early stimulation, but also throughout developmental, with aimed to reduce and prevent postural alteration or TMD manifestation.
Conflict of interestAll authors have read the journal's policy on disclosure of potential conflicts of interest and confirm that there is no competing financial conflict of interest.
FundingAll authors have disclosed any financial or personal relationship with organizations that could potentially be perceived as influencing the described research.
The financial support by FAPERGS is gratefully acknowledged.