The authors conducted a clinical-trial, uncontrolled study to determine infraorbital nerve block effectiveness.
Material and methodsNineteen adult volunteers received 1.8mL of lidocaine 2% with epinephrine 1:80,000 with an intraoral, infraorbital nerve block. Researchers used an electric pulp tester to measure pulp anesthesia in maxillary incisors and premolars. Participants reported soft tissue anesthesia and discomfort during the injection procedure; anesthesia onset time and its duration were also assessed and analyzed. Authors analyzed data using STATA statistical program 9®.
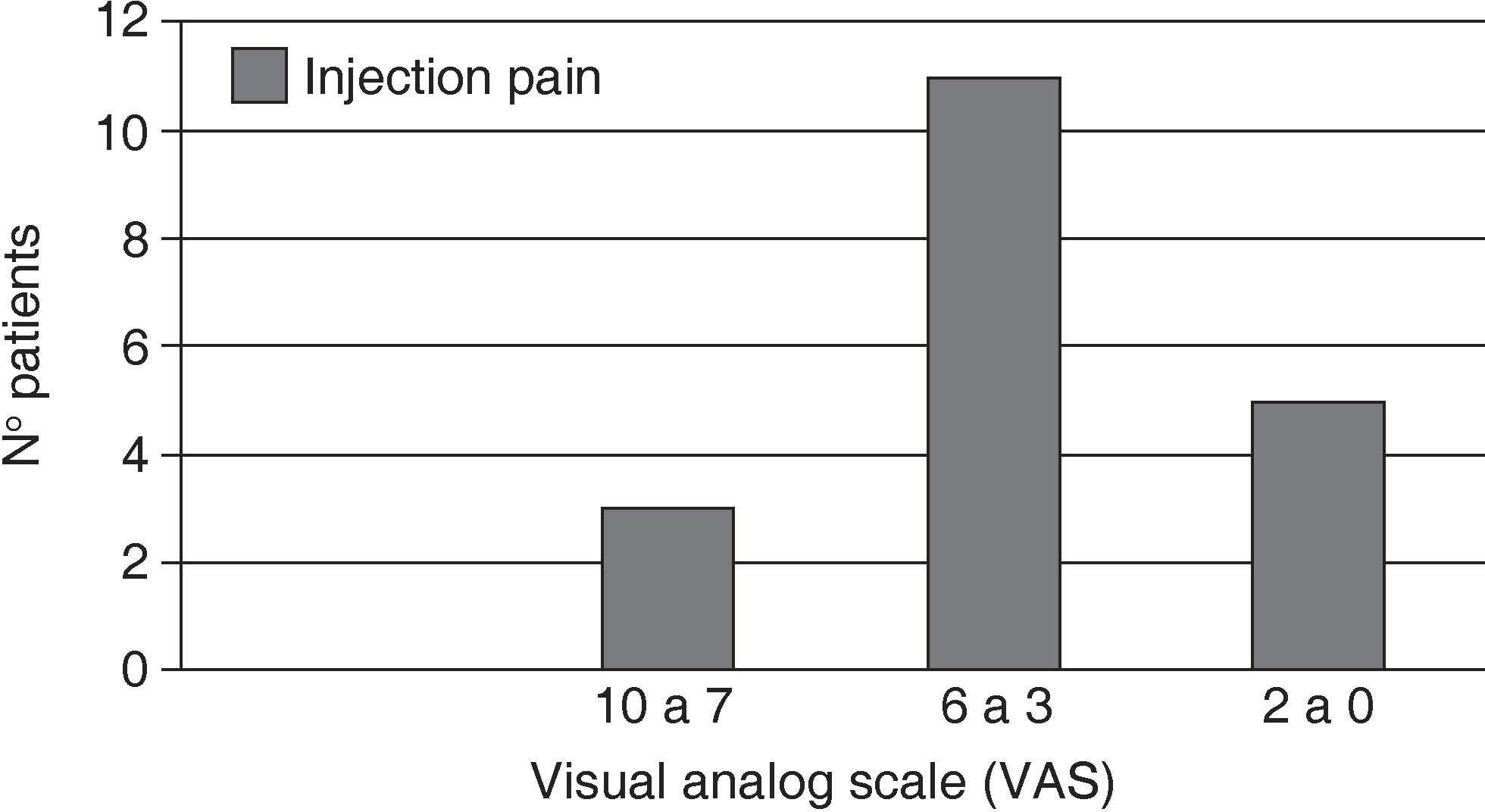
ResultsMost of the subjects in our trial were 21 years old (30%); the number of female participants (n = 12 - 60%) was greater than that of male participants. Authors evaluated pain perception when injecting anesthesia with a visual analogue scale (VAS), finding that 57.9% of patients (n = 11) categorized the pain as moderate (in a scale of 3-6). When assessing anesthesia success, it was observed that a greater number of canine teeth and first premolars (57.9%, n = 9 - CI 95%) were anesthetized. The authors also observed a significant greater number of non-response (non-anesthetized) cases in central and lateral incisors (100-84.2%, respectively). Anesthesia onset was at 12 to 19minutes, with canines exhibiting the largest number of anesthetized reports with 47.4%. There was a 100% incidence of subjective feeling of soft tissue anesthesia in lower eyelid skin, skin of the nose and skin of the upper lip. Authors noted that 100% of the subjects rated it as unpleasant (VAS).
ConclusionsInfraorbital anesthesia technique achieved successful anesthesia in only 57.9% of upper canines and first premolars; it proved ineffective for anesthetizing central and lateral incisors. This was demonstrated after these teeth were evaluated using rigorous pulp vitality testing. Soft tissue anesthesia occurred and it was classified as uncomfortable. Authors consider that usefulness of infraorbital nerve block technique in dentistry was questionable.
Los autores condujeron un ensayo clínico no controlado para determinar la efectividad de la técnica infraorbitaria, para proporcionar anestesia pulpar profunda en incisivos y premolares maxilares.
Material y métodosDiecinueve adultos voluntarios recibieron 1.8 mililitros de lidocaína al 2% con epinefrina 1:80,000 con una técnica infraorbitaria intraoral. Los investigadores usaron un electric pulp tester (vitalómetro) para medir la anestesia pulpar en incisivos y premolares maxilares. Los participantes informaron sobre anestesia en tejidos blandos, y molestias durante la inyección además de que valoraron el tiempo de inicio de la anestesia y la duración de la misma. Los autores analizaron los datos usando el programa estadístico STATA 9®.
ResultadosLa mayoría de los sujetos tenía 21 años (30%), el sexo más común fue el sexo femenino (n = 12-60%). Los autores evaluaron con escala visual análoga (VAS), la percepción del dolor al momento de aplicar la anestesia, encontrando que el 57.9% de los pacientes (n = 11) lo catalogaron como moderado (escala de 3-6). Al evaluar el éxito anestésico, observaron un mayor número de episodios en el canino y el primer premolar (57.9%, n = 9 - IC 95%), Los autores observaron un importante número de fallas en la anestesia pulpar de incisivos centrales y laterales (100-84.2%, respectivamente). El inicio de la anestesia fue a los 12-19 minutos, siendo el canino el de mayor número de reportes con un 47.4%. La incidencia de sensación subjetiva de anestesia de los tejidos blandos en piel de párpado, ala de la nariz y piel de labio superior fue del 100%, los autores observaron que el 100% de los sujetos la calificaron como desagradable (VAS).
ConclusionesLa técnica infraorbitaria produce anestesia exitosa en sólo el 57.9% de los caninos y primeros premolares maxilares; es ineficaz para anestesiar incisivos centrales y laterales, luego de ser evaluada con un riguroso test de vitalometría, se produce anestesia de tejidos blandos que es catalogada como incomoda. Los autores consideran que la utilidad de la técnica infraorbitaria en odontología es cuestionable y se deben considerar otras técnicas para los incisivos y premolares maxilares.
Many authors have reported and described that intraoral infraorbital nerve block is effective to provide deep anesthesia in upper front incisors and premolars.1 However, several clinical trials conducted to assess effectiveness of intraoral infraorbital nerve block, showed that the rate of anesthetic success in central and lateral incisors was between 15 and 30%, moreover, 100% anesthesia was not fully achieved in upper canines and premolars. Martínez MAA,2 Reed KL et al,3 Gaudy JF4 described the anatomical distribution and coverage of the infraorbital nerve, considering it responsible for the innervation of the soft tissue, skin, lips and lower eyelid, it does not innervate maxillary incisors and premolars, which are innervated by the anterior-superior alveolar nerve and uppermedial nerve respectively. Heasman PA5 reported that the origin of the upper-anterior alveolar nerve is located at a distance from infraorbital foramen, which is greater than 5 mm in 70% of specimens and greater than 20 mm in 20%. In conclusion, it can be said that the intraoral infraorbital nerve block will rarely allow diffusion of anesthetic solution to the upper-anterior alveolar nerve; therefore, anesthetic success is not guaranteed. Berberich G et al6 evaluated in 40 subjects the effectiveness of intraoral infraorbital nerve block, by comparing 2% lidocaine with 1:100,000 and 1:50,000 epinephrine with 3% mepivacaine. The research team reported that anesthesia obtained with intraoral infraorbital nerve block technique was ineffective in providing deep pulpal anesthesia in central and lateral incisors, and first molars. Success rate of anesthesia of the canines and first and second premolar ranged between 75 to 92%, when using 2% lidocaine with 1:100,000 and 1:50,000 epinephrine. Karkut B et al7 conducted a study in 40 adults to compare effectiveness of extra oral infraorbital nerve block technique and intraoral approach using 2% lidocaine with 1:100,000 epinephrine. They found that both extraoral and intraoral nerve blocks were ineffective in providing deep pulpal anesthesia in central incisors, recording only 15% of successful events; in the lateral incisors anesthesia was successful in 22% of cases, while success rate in canines was 92%; in premolars success rate was 80-90% in the first and second premolars. No statistical differences were observed between extraoral and intraoral nerve blocks. Mason et al8 evaluated the anesthetic efficacy of Lidocaine 2% with 1:100,000 and 1:50,000 epinephrine in infiltration process of maxillary lateral incisors and in first molars, using an electric pulp tester. They found that when the concentration of epinephrine was increased to 1:80,000, duration of anesthesia for the lateral incisor pulp equally increased. Authors concluded that this effect was not similar in cases of intraoral, infraorbital nerve block.
Katz et al9 evaluated the anesthetic efficacy of Lidocaine 2% with 1:100,000 epinephrine, prilocaine 4% with 1:200,000 epinephrine and 4% prilocaine in infiltration of the maxillary lateral incisor and the first molar, using an electric pulp tester. Sixty subjects received 1.8 cm3 of each anesthetic solution. There were no statistically significant differences observed either in anesthetic success or onset of pulpal anesthesia. None of the anesthetics provided one hour of pulpal anesthesia. Authors recommended infiltration of the maxillary incisors to achieve proper blocking of the anterior superior alveolar nerve branch.
The purpose of this clinical trial and uncontrolled study was to determine anesthetic success in maxillary incisors and premolars in the intraoral, infraorbital nerve block using 2% lidocaine with 1:100,000 epinephrine.
MATERIAL AND METHODSThe authors conducted a clinical trial, uncontrolled study in which anesthetic success achieved with intraoral, infraorbital nerve block was determined in maxillary incisors and premolars. Nineteen adult volunteers received 1.8 mL of 2% lidocaine with 1:80,000 epinephrine using an intraoral, infraorbital block. All subjects were healthy and not consuming any medication that would have altered pain perception. Exclusion criteria were the following: patients under 18 and over 65 years of age, with a history of allergies to amide type anesthetics, patients with any kind of restorations in maxillary incisors and premolars or who showed inability to sign the informed consent form. This study was approved by the Committee of Ethics and Research of the University of Cartagena, and informed consent was obtained from each subject.
Each subject received an intraoral, infraorbital block with 1.8 mL of 2% lidocaine with 1:80,000 epinephrine; this injection was administered by the most experienced dental researcher, following along the lines advocated by Malamed SF et al,1 Martínez MAA2 y Reed KL et al.3 Previously, the researchers had conducted a pilot study in five subjects, in order to standardize the technique and methodology proposed in this study.
Each subject randomly received the anesthetic technique, using for this purpose a randomization table made in MC Excel; authors used an electric pulp tester to measure pulp anesthesia in maxillary central incisors, lateral incisors, canines and premolars on the anesthetized side. The contralateral nonanesthetized maxillary canine was used as control in order to evaluate whether the electric pulp tester was performing properly and whether the patients responded appropriately to stimulation of the same tooth. Ninety-five teeth were evaluated and a total of 475 pulpal vitality tests were performed at a rate of 5 tests for each assessed tooth. Participants reported anesthesia in the lower eyelid skin, skin of the nose and skin of upper and lower lips; the degree of discomfort caused by the injecting procedure was also evaluated at the end of the study. Discomfort felt by participants during the injection procedure and time of anesthesia onset and duration therefore were also assessed.
Before the experiment, the anesthetic cartridge was masked, so that neither operator nor patient knew which anesthetic solution was being evaluated; thus, the experiment was blinded and protected. Anesthetic solutions used were manufactured under sterile conditions and according to highest quality standards by the company New Stetic® (2% lidocaine with 1:80,000 epinephrine; New Stetic Lab, Inc, Medellin, Colombia).
Before the intraoral infraorbital nerve block was applied, each subject was instructed on how to assess the rate of post-injection pain by using Parker's visual analog scale. Immediately after placement of the intraoral, infraorbital block, volunteers were asked about the perception of pain associated to the injection of each technique using Parker's visual analog scale which assesses absence of pain (0 mm), and the greatest pain the patient can feel (100 mm).
Pulp sensitivity was determined with an electric pulp tester (Analytic Technology, Redmond, WA, USA.). The electric pulp tester provides a digital readout from 0 to 80, which corresponds to a nonlinear voltage increase from 0 to the maximum in a 30 seconds average. Researchers performed pulp test, previous isolation of the area to assess was ensured using cotton rolls. This area was then dried with gauze, toothpaste was applied to the tip of the probe of the pulp tester and it was placed in the mid-medial zone between the gingival margin and the incisal edge of the teeth, starting at the maxillary central incisor, then the maxillary lateral incisor, the maxillary canine tooth, then the first premolar, and finally, the second premolar. Two minutes after anesthetic injection the first test was performed on all the teeth involved to evaluate pain perception, for the first 10 minutes, and then at 5 minutes intervals, completing 45 minutes of post injection testing. Before study initiation in order to validate pulp tester readings, the maxillary canine located on the opposite side of the tooth being researched was evaluated, so that the patient had knowledge of how the stimulus was perceived when there was no anesthesia. At every fourth cycle, this control tooth was tested by a battery-free pulp tester in order to test the subject's reliability. When subjects responded positively to an inactivated pulp tester, they were considered unreliable and could not be used in the study. Each reading obtained from the electric pulp tester was noted and recorded by trained personnel who had no knowledge of the solution and type of blockage being used. Radiographic evaluation was not performed, for each tooth had a vitality test with the electric pulp tester.
The infraorbital nerve block technique described by Malamed SF et al,1 Martínez MAA2 and Reed KL et al3 was used in this study. The subject was placed in a supine position with the neck slightly extended. The lefthand index finger of the professional in charge of the application of the injection was placed in the infraorbital area where the nerve packet is located, which is 5 to 10 mm below the lower edge of the orbital cavity; its location was estimated by aligning an imaginary line from the supraorbital notch, the pupil (in a forward stare), the infraorbital notch, and the long axis of the maxillary second premolar. Researchers felt with the left index finger the infraorbital notch 5-10 mm below the orbital edge, following the traced imaginary line. After locating the position of the infraorbital notch and while applying gentle pressure keeping the index finger on the area, the researcher proceeded to identify the site of intraoral puncture; the left thumb was used to lift the upper lip and maintain the deep sulcus tissues stretched. With needle bevel facing bone, the needle was inserted in the mucobuccal fold over the mesial aspect of the maxillary second premolar, a 25-gauge 11/2 inch needle was used (24 mm long with 0.40 mm of diameter), which was introduced into the previously identified zone or area of the infraorbital notch and parallel to the long axis of the upper second premolar. The needle was advanced slowly into the referenced anatomical aspects and was placed before the infraorbital notch. Before injecting the anesthetic, blood aspiration was performed; the anesthetic solution was deposited at a rate of 1.8 milliliters of Lidocaine 2% with epinephrine 1:80,000 in a period of 2 minutes. The left index finger was used to gently massage the external area of injection for 30 seconds after injection. Two minutes after anesthetic injection, the first pulp test was performed in the maxillary central and lateral incisors. At 4 minutes after the injection, the pulp test was conducted in the upper canine tooth and the upper two premolars. These pulpal evaluation cycles were repeated during the first 10 minutes and then at 5 minutes intervals until 45 minutes of testing were completed. At the end of the first 5 minutes testing cycle, subjects were asked about the subjective feeling of anesthesia in the soft tissues at the time of sensitivity testing, stimulating the skin of the periorbital region, skin of the nose and the area of the corner of upper lip skin with a sharp instrument; subjects had to answer «yes», or «no» to the temporary stimulus perceived in each of the aforementioned anatomical regions. Evaluation of comfort that the subject described with anesthesia of the soft tissues was assessed by Parker's visual analog scale (VAS), this was conducted after 45 minutes of having completed the last cycle of probing with a sharp object testing. Perception of pain associated to the injection procedure was evaluated using Parker's visual analog scale (VAS) five minutes after having completed the first cycle of sharp probe testing.
The fact that there was no response to maximum stimulation with the electric pulpal tester (80 readings), in two or more consecutive readings, was used as a criterion for successful pulpal anesthesia. The start of the pulpal anesthesia was described as the first episode of no response to maximum stimulation in two consecutive readings performed with the electric pulp tester.
The research team considered that the duration of the anesthetic effect began when the first reading of no response to the maximum stimulation occurred and until the beginning of two or more readings of response within maximum stimulation or to the end of the 45 minutes of the test.
Data were included in recollection standardized instruments and tabulated in an MC Excel database. For statistical analysis, descriptive statistical tests, frequency tables.and variable crosses were applied. χ2 test with Yates correction was applied assuming a decision limit of 0.05 using the STATA 9® statistical program.
The study took place at the Dental School of the University of Cartagena between January 2012 and July 2013 after it was approved by the local ethics committee.
RESULTSTwelve females and seven males, ages ranging 21-26 years, with average age of 21 years (30%), participated in this study. The female group was predominant averaging 60% (n = 12).
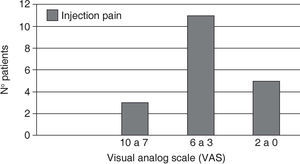
Figure 1 shows the percentages of pain perception during the anesthetic injection procedure when using Parker's visual analog scale (VAS); 57.9% of subjects (n = 11) reported moderate pain, and this pain was cataloged on a scale between 6-3 and 26.3% as mild pain (VAS 2-0).
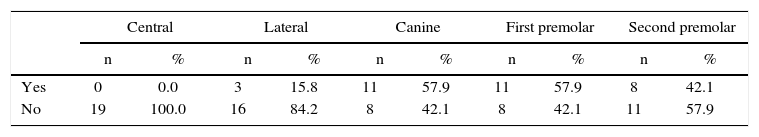
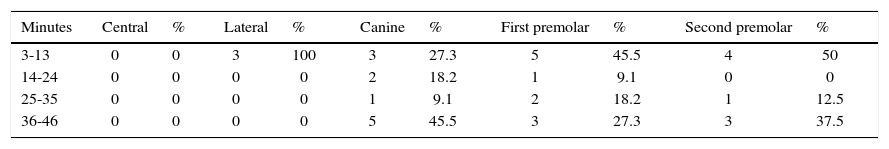
Percentages of successful pulpal anesthesia are presented in table I. Success rate of pulpal anesthesia for the maxillary canine and first premolar was 57.9% (n = 11, 45%-CI 95%). Success rate of pulpal anesthesia for the maxillary second premolar was 42.1%. Central and lateral incisors exhibited a successful rate of pulpal anesthesia ranging from 0-15.8%.
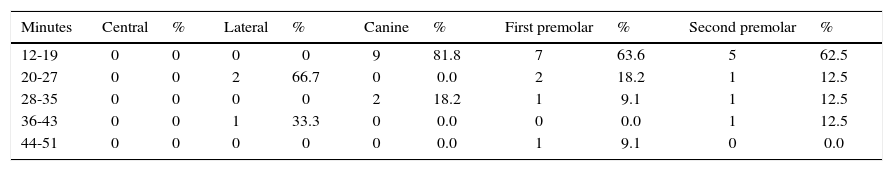
Onset of pulpal anesthesia (Table II) ranged from 12-19 minutes for the maxillary canine (81.8%) and first premolar (63.6%). The maxillary lateral incisor and the second premolar ranged from 36-43 minutes.
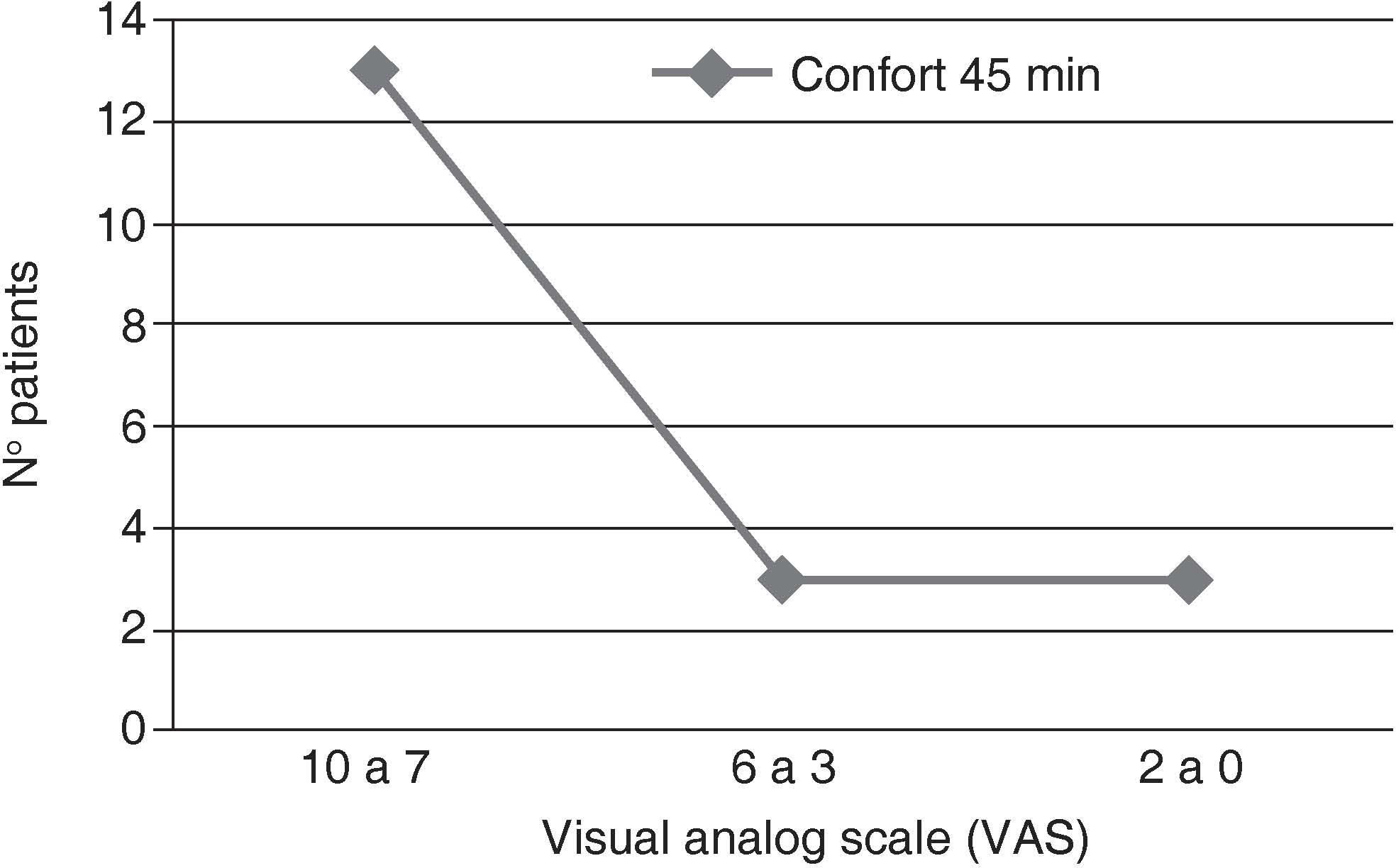
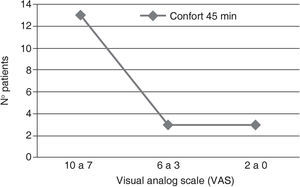
The perception of comfort that the patient felt and mentioned at the moment of feeling the soft tissue anesthesia is shown in figure 2; 68.4% of subjects (n = 13) cataloged and mentioned soft tissue anesthesia as uncomfortable (VAS = 10-7), 100% (n = 19-CI 95%) of the subjects reported anesthesia in lower eyelid skin, skin of the nose and the skin of the corner of the upper lip. Duration of the anesthetic effect ranged from 36-46 minutes for the canine tooth (Table III), duration of the anesthetic effect on the first premolar and second premolar ranged from 3 to 13 minutes.
DISCUSSIONIn order to perform dental procedures in the maxillary incisors and first and second premolars, a successful infraorbital nerve block must be chosen. Anatomical distribution of the infraorbital nerve and the anterior, medial and superior alveolar nerve must be well known and taken into account for this purpose. Malamed SF,1 Martínez MAA,2 Reed KL et al,3 and Gaudy JF4 describe anatomical distribution of infraorbital nerve ramifications, reporting that this nerve is responsible for innervating the soft tissue, skin, lips and lower eyelid and does not supply innervation to the anterior teeth and premolars, which are innervated by the anterior superior alveolar nerve and medial superior nerve, respectively.
Due to the aforementioned reasons, use of infraorbital nerve block in dental procedures in maxillary incisors and premolars is questionable. Berberich G et al6 conducted a double blind clinical trial to determine the effectiveness of the application in infra-orbital nerve block of the anesthetics 2% lidocaine with 1:100,000 epinephrine, 2% lidocaine with 1:50,000 epinephrine and 3% mepivacaine. Forty subjects were enrolled in this study to receive the infraorbital nerve block with three anesthetic solutions in separate appointments; each event took place with a week interval between appointments. A full cartridge (1.8 mL) was used for each case, and maxillary incisors, premolars and first molars were evaluated using an electric pulp tester after the application of the anesthetic solutions, with a rate of four cycles for 60 minutes. Additionally, this study, like ours, showed that the infraorbital technique was ineffective in providing deep pulpal anesthesia in maxillary central and lateral incisors, and first molars; that the success rate of anesthesia of the maxillary canine as well as first and second premolars ranged between 75 to 92%, using 2% lidocaine with epinephrine 1:100,000 and 1:50,000; in our study, success rate in maxillary canines was 60 and 15% in first premolars.
Karkut B et al7 conducted a study in 40 adults to compare the effectiveness of the extra-oral, infraorbital block and intraoral approach using 2% Lidocaine with epinephrine 1:100,000. They found that both extra-oral and intraoral blocks were ineffective in providing deep pulpal anesthesia in central incisors (15% successful events), in the lateral incisors it was successful only in 22% of all cases; while success rate was 92% in canine teeth; in the first and second premolars success rate was 80-90%, with no statistical difference found between the extra- and intraoral nerve block; these results are similar to the results in our study regarding the inefficiency of infraorbital nerve block for anesthetizing maxillary centrals and laterals since observed success rate was 10 and 30% respectively. Success rate in upper canines was 60% and in the upper first and second premolars anesthesia success was 15%, both studies confirming that the intraoral, infraorbital nerve block technique may be ineffective to anesthetize upper central and lateral incisors, and that anesthesia in premolars is variable.
Corbett IP et al10 conducted a study to compare the effectiveness of middle superior alveolar block and infraorbital block in order to obtain pulpal anesthesia in maxillary anterior teeth. Twenty-eight subjects were given shots of 2% lidocaine with 1:80,000 epinephrine, for both kinds of blockage, using electronic anesthesia equipment. Evaluation was performed with a pulp tester to determine whether successful anesthesia was significantly higher with superior alveolar block when compared to infraorbital block in maxillary central and lateral incisors; nevertheless, success rate of anesthesia in the upper central incisor was 42.9% with medial superior alveolar blockage. The authors observed a large number of non-response episodes in maxillary canine and premolars after using infraorbital nerve block. The incidence of lip anesthesia was 100%, with twofold numbness when using the infraorbital block (p = .019). When comparing both techniques, no significant differences in the feeling of comfort could be observed. These authors concluded, just like we did, that infraorbital nerve block produced successful anesthesia in maxillary canines, and was not as efficient in central and lateral incisors, in addition to the fact that the feeling of comfort in soft tissues is a subjective trait, evident when using this technique. Our study showed varying successful anesthesia in premolars, which was non constant in addition to the fact that 45% of our patients categorized the soft-tissue anesthesia in the infraorbital nerve block technique as uncomfortable (EVA = 10 to 8).
CONCLUSIONIn conclusion, the intraoral, infraorbital nerve blocking technique was ineffective in providing deep pulpal anesthesia in maxillary central and lateral incisors; its success rate was 10-30% respectively. The success rate of pulpal anesthesia, after using intraoral, infraorbital block occurred in the maxillary canine, with 60% of successful episodes. In the maxillary first and second premolars, anesthesia was variable, showing a success rate of 15%. Intraoral, infraorbital nerve block produced 95% of successful anesthesia in the corner of mouth and lips, skin of the nose, cheek and lower eyelid; 45% of patients considered it unpleasant. Pain after placement of the infraorbital nerve block technique was classified as moderate by 25% of patients. Authors believe that the infraorbital nerve block is ineffective in providing deep and long-lasting pulpal anesthesia in the upper maxillary incisors, thus, use of another more effective technique such as anterior-superior and medial-superior alveolar nerve block must be considered when performing a procedure in upper anterior teeth and premolars. Soft-tissue anesthesia is uncomfortable for patients and predisposes them to suffer injuries in those tissues, therefore, when using intraoral, infraorbital nerve block, it is necessary to guarantee and ensure full sensitivity recovery of the patient’ s affected soft tissues areas before they leave the dental office.
This article can be read in its full version in the following page: http://www.medigraphic.com/facultadodontologiaunam
Professor, Department of Oral Medicine, School of Dentistry, University of Cartagena, Cartagena-Colombia.