Maxillary osteonecrosis associated to biphosphonate use is an entity found in the mandible in 78% of all described cases. The present article presents the case of a female patient with breast cancer with bone metastasis, afflicted with maxillary osteonecrosis with sinus invasion. Routine imaging studies revealed a lesion in the right maxillary sinus which confirmed clinical suspicion. Lesion was surgically approached and removed with infrastructure hemimaxilectomy; oral-antral communication persistence was rehabilitated with a maxillary shutter. This allowed suitable control of the lesion and avoided its progression.
La osteonecrosis en los maxilares asociada al uso de los bisfosfonatos es una entidad descrita en el 78% de los casos en la mandíbula, aquí presentamos el caso de una paciente con cáncer de mama metastásico a hueso que cursó con osteonecrosis maxilar que invadía a seno. A la solicitud de estudios de imagen rutinarios se identificó lesión en seno maxilar derecho que confirmaba la sospecha clínica. La lesión fue abordada y extirpada quirúrgicamente con hemimaxilectomía de infraestructura, la persistencia de comunicación oroantral fue rehabilitada con un obturador maxilar, lo que permitió buen control de la lesión, evitando la progresión de la misma.
Biphosphonates are chemical composites analogue to inorganic pyrophosphate. They are modulators of bone exchange and osteoclastic resorption inhibitors. They are indicated in many bone conditions such as, among others, osteoporosis, Paget's disease, hypercalcemia, multiple myeloma and bone metastases of malignant tumor conditions. Biphosphonates exhibit high bonding degree to hydroxyapatite, they decrease cell replacement and bone remodeling, induce osteoclast apoptosis and inhibit osteocyte apoptosis; moreover, they possess antiangiogenic effect which decreases endothelial growth factor, inhibiting thus cell cycle of keratinocytes.1–12
This group of medications is used to prevent and treat diseases causing bone resorption, such as osteoporosis and cancer with bone metastasis (either with or without hypercalcemia), associated to breast and prostate cancer. They are prescribed to treat Paget's disease as well as for other conditions causing bone fragility, such as chronic renal disease treated with dyalisis.1–12
With respect to their action mechanism, it can be said that especially alendronate and risendronate are the only non-hormonal agents having shown to reduce vertebral and peripheral fractures. Biphosphonates reduce bone replacement decreasing the sites of active remodeling where excessive resoprtion takes place. The main activity mechanisms are: as soon as etidronate and clodronate are captured by osteoclasts and converted into ATP (adenosine triphosphate) toxic analogues, most current bisphosphonates act inhibiting synthase farnesyl phosphate, an enzyme from the cholesterol synthesis pathway based on mevalonate, indirectly suppressing the process of protein geranil-geranilization, which in turn inhibits osteoclastic activity.1–12
There are two ways of administration: oral and intravenous. Among drugs available to oral administration we find etidronate (single dosis of 400 mg/day in two week cycles, repeated every three months) alendronate (one daily 10 mg dose, or one 70 g weekly dose) and risedronate (one daily 5 mg dose). These drugs have shown to reduce fracture incidence in 40 to 60%. Other bisphosphonates, such as ibandronate and pamidronate also decrease frequency of vertebral fractures, although results obtained when using clodronate are doubtful. Main drug for intravenous administration is zoledronic acid-zoledronate (4 mg as single intravenous persusion during 15 minutes). They induce increase in bone mineral density, in the spine as well as in the hip, since they bond to bone matrix, decreasing osteoclastic activity and preventing bone resorption.1–12
In general terms, bisphosphonates, when suitably administered, are well tolerated drugs. Most frequent secondary effects are those related to the upper digestive system. They can slightly increase frequency of erosions and gastric ulcers, and have also been described in some cases of esophagitis and esophageal stricture. Untoward ocular effects such as conjunctivitis, scleritis or uveitis have seldom been described. Etidronate continuous administration can inhibit mineralization and cause focal osteomalacia, thus it tends to be intermittently prescribed. Modern bisphosphonates lack this effect.1–12
Biphosphonates have been associated to jaw (mandible) osteonecrosis; 60% of all these cases began after (bone) dental surgery, it is now recommended to postpone treatment until after surgical procedure in order to avoid infection. This last untoward secondary effect is much more frequent when bisphosphonates are used intravenously, generally in cancer treatments, due to their accumulative effect. Sine bones remain impregnated during long years, preventive effect of suppressing bisphosphonates is debatable.1–12
Although bisphosphonates have proven their effectiveness, recently an increase of clinical cases has been found where bisphosphonate use has been related to jaw osteonecrosis, therefore, dentists must be vigilant about possible complications in patients ingesting this drug. In this context, collaboration with oncologist and maxillofacial surgeon will be of the utmost importance when patients treated are ingesting bisphosphonates, so as to take necessary precautions to prevent osteonecrosis. These precautions could be caries control, use of non traumatic prostheses in the lingual area as well as avoidance of implants and invasive periodontal treatment.1–12
Osteonecroses possess multi-factorial origins such as alterations in bone balance, keratocyte cell cycle inhibition, angiogenesis decrease, as well as superinfection of oral bacterial flora and jaw microtrauma. It is more frequently found in females, ages ranging 56-71 years. According to different studies, lower jaw involvement is more frequent (78%), this is possibly due to the fact that this bone is less irrigated than the upper jaw, in addition to being irrigated by a terminal artery, upper jaw involvement is observed in 16%, and in both locations in 5%. Typical presentation is an area of a painless bone exposition of variable size, with adjacent soft tissue tumefaction; there can also be presence of foul smell, ulceration, tooth sensitivity, burning sensation, tooth mobility, paresthesia, deformities, difficulty in eating or speaking, oral hygiene limitations, fever and non-adhered painful submandibular adenopathies. Imaging studies are unspecific. Conventional X-rays, computerized tomography and magnetic resonance exhibit osteolytic lesions with cortical plate involvement, alternating with osteoclerosis areas, and occasionally, soft tissue edema defining its extension. Therefore, histopathological study is essential in order to emit accurate diaganosis.2–15
The present article reports the case of a clinical case diagnosed at the State Cancer Center ISSEMyM, at the Maxillofacial Prostheses Service. The case reveals an unusual anatomical variant and evolution of upper jaw osteonecrosis highlighting current concepts on the subject and assessing the importance of timely diagnosis.
Clinical caseA 62 year old female patient with diagnosis of infiltrating ductal carcinoma in the left breast, Clinical Stage IIIB. Patient had been subjected to modified radical mastectomy, with SBR (Scarff-Bloom-Richardson) of nine with 18/18 lymph nodes with metastasis. Patient had received radiotherapy and later chemotherapy based on three cycles of adriamycin-cyclophosphamide, five cycles of Gemzar-5-fluoracil, three cycles of taxotere, and six cycles of paclitaxel-carboplatin. Patient discontinued chemotherapy treatment in May 2005 due to liver toxicity and then besgan surveillance period.
In January 2008 bone metastasis were documented in the left parietal area of the skull and body of the L1 vertebra. The patient received then seven cycles of zoledronic acid.
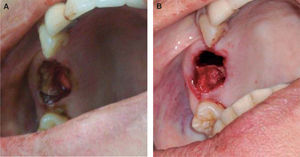
In March 2008, the patient attended the Maxillofacial Prosthesis Services (Figure 1). She exhibited a 1 cm diameter bone exposition in the right maxillary region; the lesion exhibited necrotic aspect, with erythema in surrounding tissues, and no symptoms. Orthopantomography and bone gammagram were requested in order to discard presence of metastasis. Bone washes were initiated to denude necrotic bone and perform curettage (partially eliminating it for an incisional biopsy), combined antibiotic therapy was prescribed (ciprofloxacin and clindamycin).
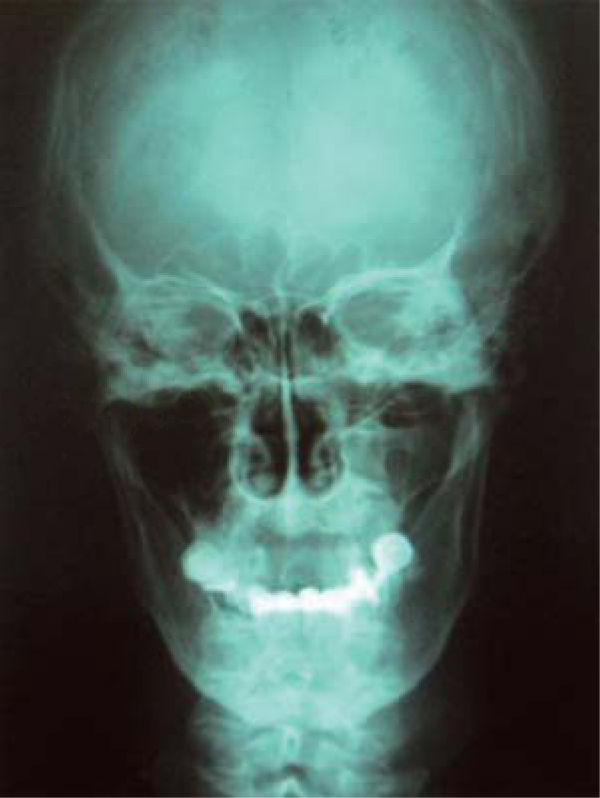
Histopathological result revealed facial necrosis with chronic inflammation and acute ulceration associated to microorganisms morphologically compatible with actynomices, compatible with chronic and acute osteomyelitis. Bone gammagram revealed increased cellular exchange compatible with inflammation. Orthopantomography and anterior posterior skull X-rays (Figures 2and3) revealed invasive lesion in the right maxillary sinus (Table I).
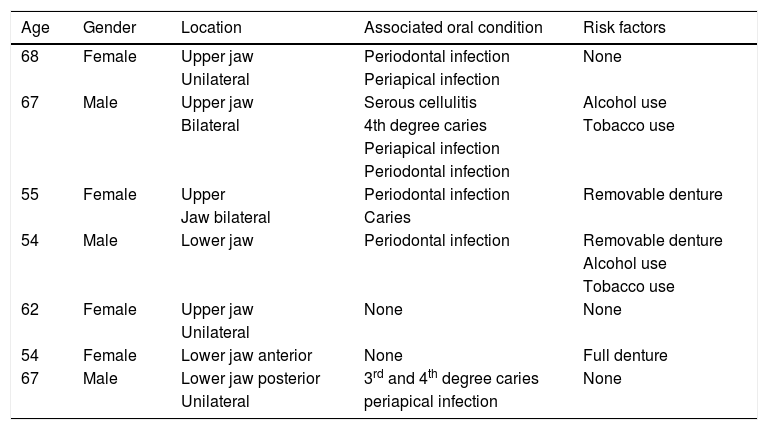
Patients’ characteristics.
| Age | Gender | Location | Associated oral condition | Risk factors |
|---|---|---|---|---|
| 68 | Female | Upper jaw | Periodontal infection | None |
| Unilateral | Periapical infection | |||
| 67 | Male | Upper jaw | Serous cellulitis | Alcohol use |
| Bilateral | 4th degree caries | Tobacco use | ||
| Periapical infection | ||||
| Periodontal infection | ||||
| 55 | Female | Upper | Periodontal infection | Removable denture |
| Jaw bilateral | Caries | |||
| 54 | Male | Lower jaw | Periodontal infection | Removable denture |
| Alcohol use | ||||
| Tobacco use | ||||
| 62 | Female | Upper jaw | None | None |
| Unilateral | ||||
| 54 | Female | Lower jaw anterior | None | Full denture |
| 67 | Male | Lower jaw posterior | 3rd and 4th degree caries | None |
| Unilateral | periapical infection |
In May 2009, the patient was subjected to extensive surgical resection (infrastructure hemimaxilectomy) with right maxillary sinus curettage with partial closure of denuded bone achieved with collagen membranes (Figure 4), and persistence of oral-antral communication which at a later point (July 2009) was rehabilitated with prosthesis and use of a maxillary shutter allowing thus suitable lesion control. Presently, the patient is at a follow-up stage, performing rinses in the dental office with material based on sterile injectable solution, as well as daily rinses with benzidine-based material. With this regimen patient remained asymptomatic and infection free.
DiscussionAccording to a meta-analysis conducted by Fresco et al, 200514–16 biphosphonate-related osteonecrosis affects females in a 66.9% proportion with mean age of 65 years.
According to different studies, most affected sites are the lower jaw (78%), upper jaw (16%), and both jaws (5%), thus the reasoning of maxillary presentation of our case along with supra-structure involvement is widely diminished, lacking any type of report.3,7,9,13–16
Reports indicate that biphosphonate-induced osteonecrosis is time-dosage dependent, with a margin of time going from 4 months after treatment initiation with incidence of 1.5% increasing to 10% after three years.3 Diagnosis of this condition in comorbid patients is based on use of clinical history and imaging studies (although these have shown to be non-specific), clinical assessment of lesion's own characteristics and conducting a histopathological study by means of a biopsy.2,5,10
The increase of incidence of bisphosphonateassociated osteonecrosis is proportional to the increment of drugs used in current medical practice due to their effectiveness in the treatment of several conditions.3,5,8 Patients who are going to be subjected to bisphosphonate treatment must be subjected to a thorough oral examination before, during and after treatment so as to decrease risk factors, achieve timely diagnosis and decrease osteonecrosis –related complications in maxillary bones. In medicine, the best treatment is still prevention3,14
Treatment of osteonecrosis has been suggested with the following regimens: rinses of 0.12% chlorhexidina digluconate, antibiotic therapy combining amoxicillin and metrodinazol clindamycin, amoxicillin with clavulanic acid, surgical intervention to eliminate necrotic bone tissue, limited debridement, use of non-steroid analgesics (ibuprofen, nimesulide, naproxen, diclofenac and ketocorolac), toothpaste and rinse with benzydamine hydrochloride and an oral antiseptic solution with neutral pH (Estericide). Osteonecrosis staging will determine the best treatment for each individual patient.6,11–13
The patient reported in our case was treated with antibiotics (ciprofloxacin, amoxicillin and clindamycin) immediately after being diagnosed with osteonecrosis. She performed rinses in the area of exposed bone with isodine plus sterile injectable solution. Symptomatology was controlled with daily rinses of benzidine; surgical removal of necrotic bone was conducted along with maxillary sinus curettage, followed by defect closure with collagen membranes, preserving oral-antral communication which was later rehabilitated with a maxillary shutter.
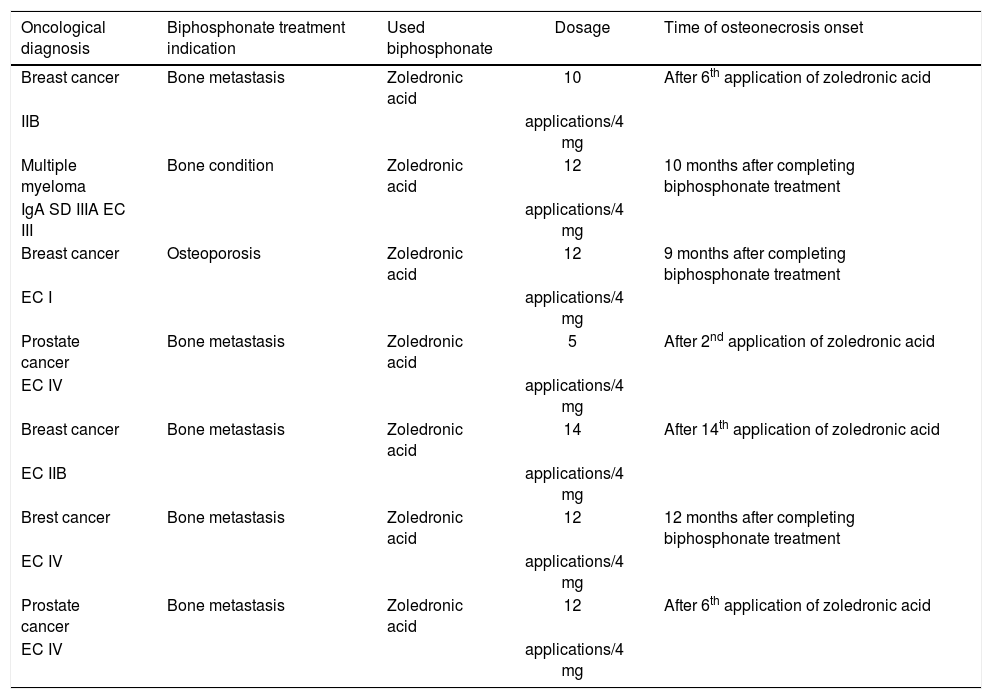
ConclusionsEvidence obtained in the present study suggests that alveolar bone can be affected before as well as independently from documented risk factors; progression of condition called bisphosphonate-use associated osteonecrosis depends on factors such as morbidity of each (Table II). Risk factors commonly associated to onset of maxillary osteonecrosis derive from dental procedures, among which the most frequent are procedures undertaken due to previous trauma, poor oral hygiene, periodontal disease or periapical infections.
Characteristics of treatment performed before osteosis.
| Oncological diagnosis | Biphosphonate treatment indication | Used biphosphonate | Dosage | Time of osteonecrosis onset |
|---|---|---|---|---|
| Breast cancer | Bone metastasis | Zoledronic acid | 10 | After 6th application of zoledronic acid |
| IIB | applications/4 mg | |||
| Multiple myeloma | Bone condition | Zoledronic acid | 12 | 10 months after completing biphosphonate treatment |
| IgA SD IIIA EC III | applications/4 mg | |||
| Breast cancer | Osteoporosis | Zoledronic acid | 12 | 9 months after completing biphosphonate treatment |
| EC I | applications/4 mg | |||
| Prostate cancer | Bone metastasis | Zoledronic acid | 5 | After 2nd application of zoledronic acid |
| EC IV | applications/4 mg | |||
| Breast cancer | Bone metastasis | Zoledronic acid | 14 | After 14th application of zoledronic acid |
| EC IIB | applications/4 mg | |||
| Brest cancer | Bone metastasis | Zoledronic acid | 12 | 12 months after completing biphosphonate treatment |
| EC IV | applications/4 mg | |||
| Prostate cancer | Bone metastasis | Zoledronic acid | 12 | After 6th application of zoledronic acid |
| EC IV | applications/4 mg |
The high incidence of these oral conditions affecting bone found in our population, must give rise to a preventive environment, since they cause dentalorigin bone infections, requiring thus greater cell exchange in the jaws, which cannot take place since it has become impaired by bisphosphonate action; moreover, these drugs exhibit anti-angiogenetic effect causing endothelium's growth factor decrease, thus deteriorating healing processes. Uncertainty on this subjects dictates its clarification through different research lines which might allow to acquire necessary knowledge to offer patients a better quality of life.2,13,16