To evaluate the association between duration of breastfeeding (BF) and obesity in schoolchildren of Florianópolis (SC), and the role of possible effect modifiers.
MethodsCross-sectional study with a random sample of 2826 schoolchildren (7–14 years). Weight and height were measured according to standardized procedures. Data concerning BF and sociodemographic variables were obtained from a questionnaire sent to parents/guardians. Children's nutritional status was evaluated by BMI-for-age z-score for gender (WHO reference curves). Adjusted analyses were performed through logistic regression, considering a possible interaction among variables.
ResultsPrevalence of obesity was 8.6% (95% CI: 7.6–9.7%) and 55.7% (95% CI: 53.8–57.6%) received breastmilk for ≥6 months. BF was not associated with obesity, even in the adjusted analysis. Stratified analysis according to maternal schooling showed that, in children aged 7–10 years and children whose mothers had 0–8 years of schooling, the chance of obesity was lower among those breastfeed for >1 month, especially among those who received breastmilk for 1–5 months (OR=0.22; 95% CI 0.08–0.62). Among children of women with higher schooling (>8 years), the chance of obesity was 44% lower in those who were breastfed for >12 months (p-value for interaction<0.01). This interaction was not found in older children (11–14 years).
ConclusionsAmong children of women with lower schooling, BF for any period longer than 1 month is protective against obesity; however, for a higher maternal schooling, BF for less than 12 months increases the odds of obesity.
Avaliar a associação entre a duração do aleitamento materno (AM) e a obesidade em escolares de Florianópolis (SC), assim como o papel de possíveis modificadores de efeito.
MétodosEstudo transversal com amostra probabilística de 2.826 escolares de 7–14 anos. Foram aferidos o peso e a altura dos escolares, de acordo com procedimentos padronizados. Dados referentes ao AM e variáveis sociodemográficas foram obtidos por questionário enviado aos pais/responsáveis. O estado nutricional foi avaliado pelo escore-Z IMC/idade (curvasda OMS), de acordo com o sexo. Análises ajustadas foram feitas com regressão logística e foi considerada a possível interação de variáveis.
ResultadosA obesidade afetou 8,6% dos escolares (IC95%: 7,6–9,7%) e o AM por ≥ seis meses foi encontrado em 55,7% (IC95%: 53,8%-57,6%). O AM não esteve associado à obesidade, mesmo nas análises ajustadas. As análises estratificadas por escolaridade materna mostraram que, nas crianças de 7-10 anos e filhos de mulheres com até oito anos de estudo, a obesidade foi menor nos que receberam AM por qualquer período >1 mês, em especial entre aqueles que receberam AM por 1-5 meses (RO=0,22; IC95%: 0,08–0,62). Nos filhos de mulheres com maior escolaridade (>8 anos), a chance de obesidade foi 44% menor nos que haviam recebido leite materno por >12 meses (p de interação <0,01). Em adolescentes de 11–14 anos não foi verificada essa interação.
ConclusõesO AM por períodos maiores do que um mês em filhos de mulheres com baixa escolaridade protege contra a obesidade, mas quando a escolaridade materna é maior, períodos de AM menores de 12 meses aumentam as chances de obesidade.
Over the past four decades, there has been an increase of at least five fold in the prevalence of obesity among children and adolescents aged 5–19 years of both genders, in Brazil.1
Obesity is a multifactorial disease associated with several health problems2. There are several factors associated with obesity, and breastfeeding (BF) seems to protet against the disease. The evidence that BF can protect against obesity seems to be related to the fact that breastmilk has a different composition and hormonal response compared to other milks, which may also be related to the adaptation to the diet after BF.3 However, the hypothesis of this protective effect remains unclear.3–10
Few studies on this association have been carried out in middle or low-income countries, including Brazil,11,12 particularly in the age range of elementary school students. In this context, the aim of the study was to evaluate the association between duration of breastfeeding (BF) and obesity in schoolchildren from Florianópolis, state of Santa Catarina, Brazil, and the role of potential effect modifiers in elementary school students in the same city.
MethodCross-sectional study with a random sample of schoolchildren aged 7–14 years enrolled in public and private elementary schools in Florianópolis (SC). Sample size calculation and sample selection have been described in a previously published article.13 In brief, it was considered for sample size calculation a prevalence of 10% of obesity in children aged 7–10 years and 17% in adolescents aged 11–14 years, with a margin of error of 2%, design effect of 1.3 and study power of 80%. Considering these data, we estimated the number of 2800 students to be assessed. Moreover, assuming a random loss of 10%, we obtained a total of 3100 schoolchildren to be selected.
The study used a probabilistic sampling design in two phases. In the first phase, local schools were divided into four strata, according to two geographical areas (downtown/continent and beaches) and types of school (public or private). Within each stratum, schools were randomly selected. The sample included 17 schools (11 public and 6 private). In the second phase, in each included school, children were randomly selected.
The study included students aged 7–14 years that had the permission of their parents or guardians to participate, by signing the informed consent form. The study was approved by the Institutional Review Board of Universidade Federal de Santa Catarina/CCS on 24 April 2006 (Opinion 028/06).
The data collection team consisted of 10 trained and standardized examiners. A pilot study was carried out with anthropometric measurements in two schools of Florianópolis that were not included in the study sample.14
Anthropometric measurements were performed according to the protocol defined by the World Health Organization (WHO) reference curves,15 based on the recommendations of Lohman, Roche and Martorell (1988).16 Body weight was measured using an electronic Marte® scale with 180kg capacity and accuracy of 100g, and height was measured using an Alturexata® stadiometer, with accuracy of one millimeter. Data were collected between March and December 2007.
Data related to BF and other information used for the control variables were obtained through a questionnaire sent to students’ parents/guardians. Birth and childhood data of the schoolchildren (birth weight, gestational age and duration of breastfeeding), demographic data (maternal schooling and age, total monthly income, number of household members) and anthropometric data of the schoolchildren's mothers (self-reported weight and height) were collected. The covariate sexual maturation was collected only in students aged 11–14 years, through a spreadsheet containing the figures corresponding to the sexual maturation stages proposed by Tanner17 in drawings.
BF data were obtained based on the following question to the parents or guardians, “How long was the student breastfed?” This question was divided into breastfeeding time categories, which were then grouped for data analysis.
The data were processed electronically in the software EpiData 3.0 and all data were verified and received automatic checks for consistency and amplitude.
The schoolchildren's nutritional status (outcome variable) was categorized as without obesity (≤z-score +2) or obese (>z-score +2), based on body mass index (BMI) curves for age and gender, according to the WHO reference curves (2007).18 For comparative analysis, nutritional status was also classified according to the recommendation of the International Obesity Task Force (IOTF), according to Cole et al.19 The intention of this comparison was to verify whether the association results were similar, as most of the studies on the subject used a different classification than that used by the WHO (2007).18
The BF (exposure variable) was analyzed in two different ways: first, it was categorized dichotomously as “never received breastmilk/received for <1 month” or “received for ≥1 month”; then, it was categorized according to the duration of breastfeeding, “never received breastmilk/received breastmilk for <1 month,” “from 1 to 5 months”, “from 6 to 12 months” and “for >12 months.”
Schoolchildren age was classified into two groups: 7–10 and 11–14 years, and association analyses were performed independently, according to the age group. The variables used as possible confounding factors were: child gender; maternal age (20–29 years; 30–39 years; ≥40 years) and schooling (0–8 and >8 years), maternal nutritional status (underweight/normal weight, BMI<25.0kg/m2; pre-obesity, BMI=25.0–29.9kg/m2, obesity, BMI≥30kg/m2, according to WHO classification);15per capita family income in tertiles (R$25.00–220.00; R$225.00–450.00; R$446.00–6667.00); birth weight (considered as low/insufficient when birth weight≤2.999g),15 and gestational age at birth of the student (premature if gestational age<37 weeks). The sexual maturation stage was used for the students aged 11–14 years as a covariate that may influence BF associations with the outcome.
All analyses were performed using STATA statistical software, release 11.0. The bivariate analysis was performed using the chi-square test for heterogeneity or trend, according to the nature of the independent variables. Logistic regression was used for the multivariate analysis, in which the variables were included and maintained in the analyses by backward selection, according to hierarchy levels. Variables with p<0.20 in the adjusted analysis were kept in the model as potential confounders. Interaction analyses were also performed, in which the variables per capita family income, maternal schooling and nutritional status were tested as potential effect modifiers of the BF and obesity association.
The SVY command of STATA was used in all analyses to consider the sampling effect. All regression results are shown as Odds Ratio (OR) with their respective 95% confidence intervals (95% CI), considering variables with statistical significance those with p<0.05.
ResultsOf the 3100 students selected for the study, data on 2863 individuals were obtained. Of these, 37 students were excluded because they were aged <7 or >14 years, adding up 2826 participants (91.2%), which was in accordance with the minimum calculated sample size (2800 students).
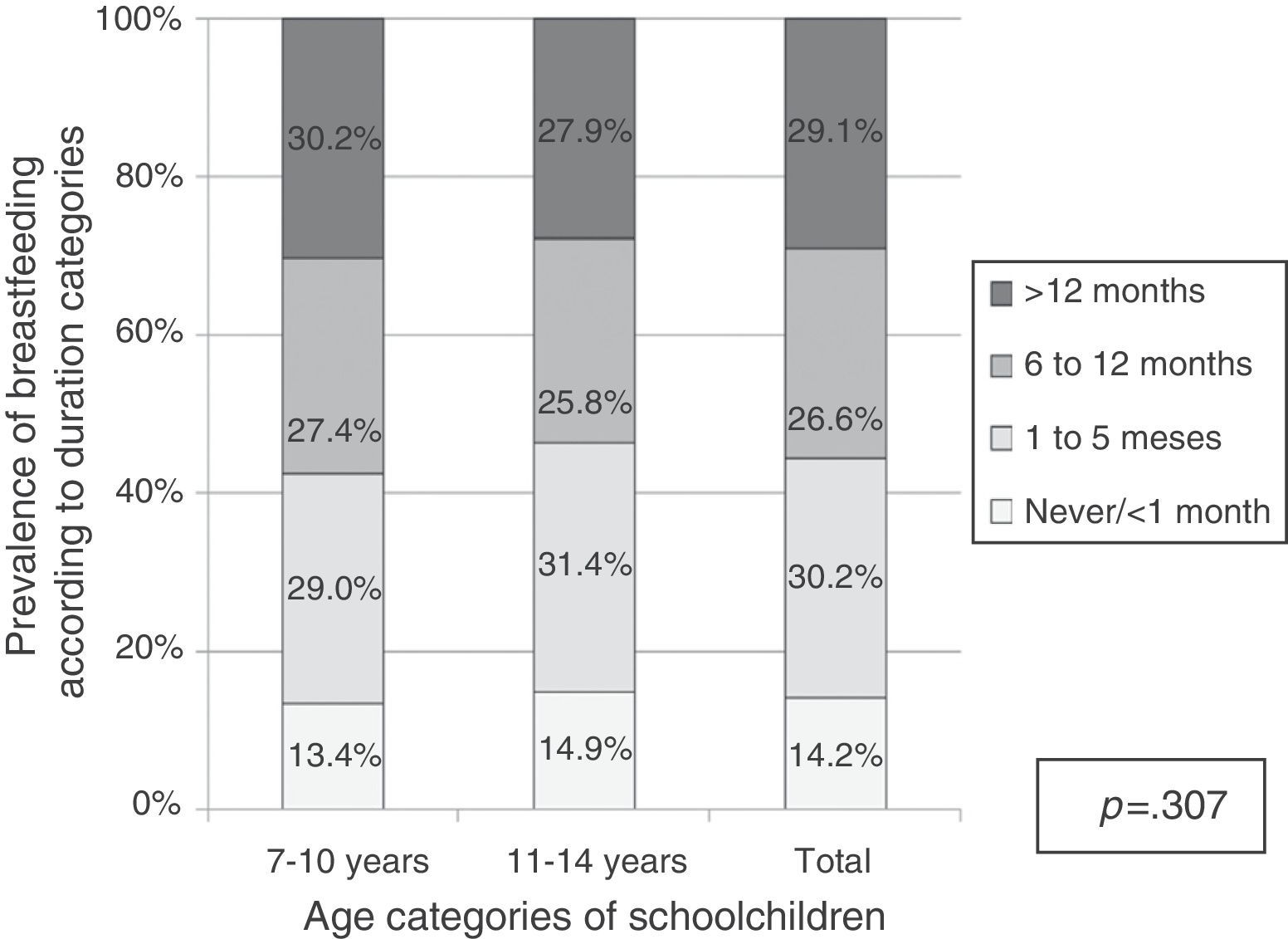
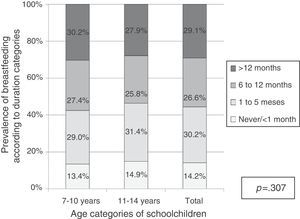
The final study sample consisted of 1232 schoolchildren aged 7–10 years and 1594 aged 11–14 years. The overall prevalence of obesity was 10.5% among children aged 7–10 years (95% CI: 8.0–12.3%) and 6.7% (95% CI: 5.7–8.3%) among children aged 11–14 years (p<0.001). Regarding BF, Fig. 1 shows that 44.4% of children were breastfed for less than 6 months, and less than a third was breastfed for more than 12 months. There was no difference in the prevalence of BF when comparing the two age groups (p=0.307).
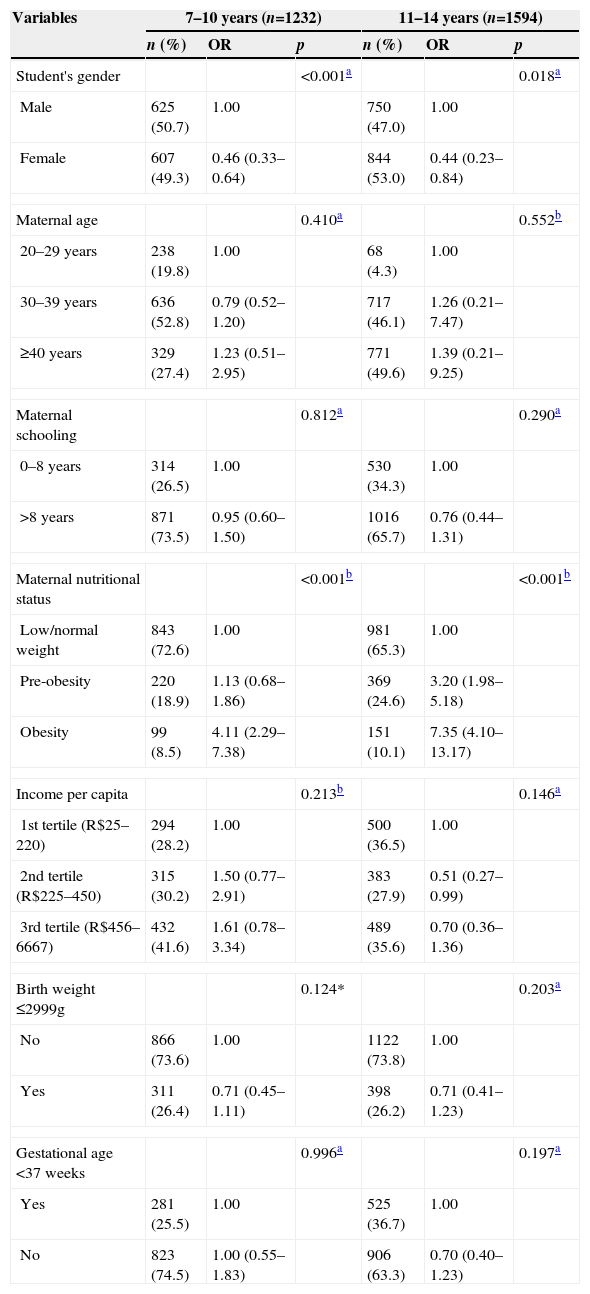
Table 1 shows the sample distribution according to the variables used as potential confounders in this study, as well as the Odds Ratio of obesity according to these variables. In the age group of 7–10 years, both genders showed similar distribution, with 50.7% of the sample being male. The prevalence of obesity in this age group was 13.9% in boys (95% CI: 11.3–16.9%) and 6.9% in girls (95% CI: 5.0–9.2%) (p<0.001). Among students aged 11–14 years, 53% were female, and the prevalence of obesity was 9.3% (95% CI: 7.3–11.6%) in males versus 4.3% (95% CI: 3.1–6.0%) in females (p=0.018).
Crude Odds Ratio (OR) for obesity according to characteristics of the students aged 7–14 years, their mothers and families. Florianópolis, SC, 2007.
| Variables | 7–10 years (n=1232) | 11–14 years (n=1594) | ||||
|---|---|---|---|---|---|---|
| n (%) | OR | p | n (%) | OR | p | |
| Student's gender | <0.001a | 0.018a | ||||
| Male | 625 (50.7) | 1.00 | 750 (47.0) | 1.00 | ||
| Female | 607 (49.3) | 0.46 (0.33–0.64) | 844 (53.0) | 0.44 (0.23–0.84) | ||
| Maternal age | 0.410a | 0.552b | ||||
| 20–29 years | 238 (19.8) | 1.00 | 68 (4.3) | 1.00 | ||
| 30–39 years | 636 (52.8) | 0.79 (0.52–1.20) | 717 (46.1) | 1.26 (0.21–7.47) | ||
| ≥40 years | 329 (27.4) | 1.23 (0.51–2.95) | 771 (49.6) | 1.39 (0.21–9.25) | ||
| Maternal schooling | 0.812a | 0.290a | ||||
| 0–8 years | 314 (26.5) | 1.00 | 530 (34.3) | 1.00 | ||
| >8 years | 871 (73.5) | 0.95 (0.60–1.50) | 1016 (65.7) | 0.76 (0.44–1.31) | ||
| Maternal nutritional status | <0.001b | <0.001b | ||||
| Low/normal weight | 843 (72.6) | 1.00 | 981 (65.3) | 1.00 | ||
| Pre-obesity | 220 (18.9) | 1.13 (0.68–1.86) | 369 (24.6) | 3.20 (1.98–5.18) | ||
| Obesity | 99 (8.5) | 4.11 (2.29–7.38) | 151 (10.1) | 7.35 (4.10–13.17) | ||
| Income per capita | 0.213b | 0.146a | ||||
| 1st tertile (R$25–220) | 294 (28.2) | 1.00 | 500 (36.5) | 1.00 | ||
| 2nd tertile (R$225–450) | 315 (30.2) | 1.50 (0.77–2.91) | 383 (27.9) | 0.51 (0.27–0.99) | ||
| 3rd tertile (R$456–6667) | 432 (41.6) | 1.61 (0.78–3.34) | 489 (35.6) | 0.70 (0.36–1.36) | ||
| Birth weight ≤2999g | 0.124* | 0.203a | ||||
| No | 866 (73.6) | 1.00 | 1122 (73.8) | 1.00 | ||
| Yes | 311 (26.4) | 0.71 (0.45–1.11) | 398 (26.2) | 0.71 (0.41–1.23) | ||
| Gestational age <37 weeks | 0.996a | 0.197a | ||||
| Yes | 281 (25.5) | 1.00 | 525 (36.7) | 1.00 | ||
| No | 823 (74.5) | 1.00 (0.55–1.83) | 906 (63.3) | 0.70 (0.40–1.23) | ||
OR, Odds Ratio.
As for the mothers of the schoolchildren aged 7–10 years, most were aged between 30–39 years (52.8%), and among the mothers of those aged 11–14 years, 40 years or older (49.6%). Regarding maternal schooling, most had more than 8 years of schooling (69.6%). Maternal age and schooling were not associated with the prevalence of obesity in both age groups. The prevalence of maternal obesity was 9.3% in the total sample, and this variable increased by at least four times the odds of obesity among schoolchildren (p<0.001 in both age groups). Regarding per capita family income, among schoolchildren aged 7–10 years, the odds of obesity was higher in higher monthly income, but this association did not reach statistical significance (p=0.213).
Regarding the birth variables, most of the schoolchildren was born weighing ≥3000g (73.7%) and were not premature (68.9%). Neither variable was associated with obesity in the schoolchildren.
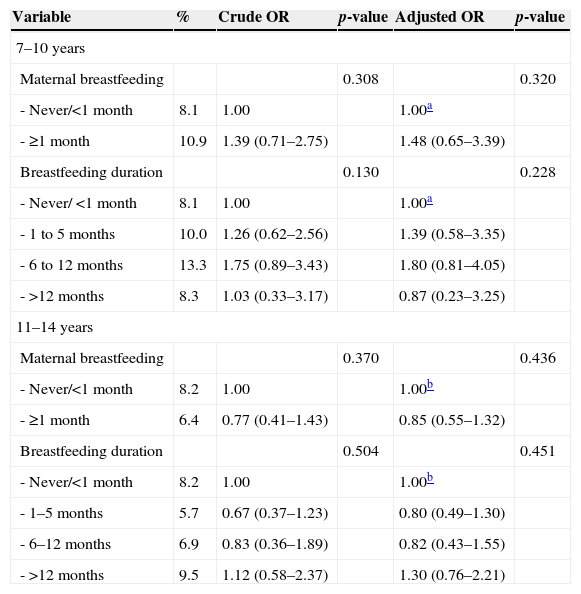
According to Table 2, the prevalence of obesity in schoolchildren was not associated with duration of BF in any of the age groups, neither in the crude analysis nor after adjustment for possible confounding factors. The same effect was observed when BF was treated as a dichotomous or polytomous variable. Nonetheless, among children aged 7–10 years, BF indicated a greater chance of obesity, while among those aged 11–14 years the association was a protective one.
Prevalence (%) of obesity, crude and adjusted Odds Ratio according to breastfeeding and breastfeeding duration categories, stratified by age. Florianópolis, SC, 2007.
| Variable | % | Crude OR | p-value | Adjusted OR | p-value |
|---|---|---|---|---|---|
| 7–10 years | |||||
| Maternal breastfeeding | 0.308 | 0.320 | |||
| - Never/<1 month | 8.1 | 1.00 | 1.00a | ||
| - ≥1 month | 10.9 | 1.39 (0.71–2.75) | 1.48 (0.65–3.39) | ||
| Breastfeeding duration | 0.130 | 0.228 | |||
| - Never/<1 month | 8.1 | 1.00 | 1.00a | ||
| - 1 to 5 months | 10.0 | 1.26 (0.62–2.56) | 1.39 (0.58–3.35) | ||
| - 6 to 12 months | 13.3 | 1.75 (0.89–3.43) | 1.80 (0.81–4.05) | ||
| - >12 months | 8.3 | 1.03 (0.33–3.17) | 0.87 (0.23–3.25) | ||
| 11–14 years | |||||
| Maternal breastfeeding | 0.370 | 0.436 | |||
| - Never/<1 month | 8.2 | 1.00 | 1.00b | ||
| - ≥1 month | 6.4 | 0.77 (0.41–1.43) | 0.85 (0.55–1.32) | ||
| Breastfeeding duration | 0.504 | 0.451 | |||
| - Never/<1 month | 8.2 | 1.00 | 1.00b | ||
| - 1–5 months | 5.7 | 0.67 (0.37–1.23) | 0.80 (0.49–1.30) | ||
| - 6–12 months | 6.9 | 0.83 (0.36–1.89) | 0.82 (0.43–1.55) | ||
| - >12 months | 9.5 | 1.12 (0.58–2.37) | 1.30 (0.76–2.21) | ||
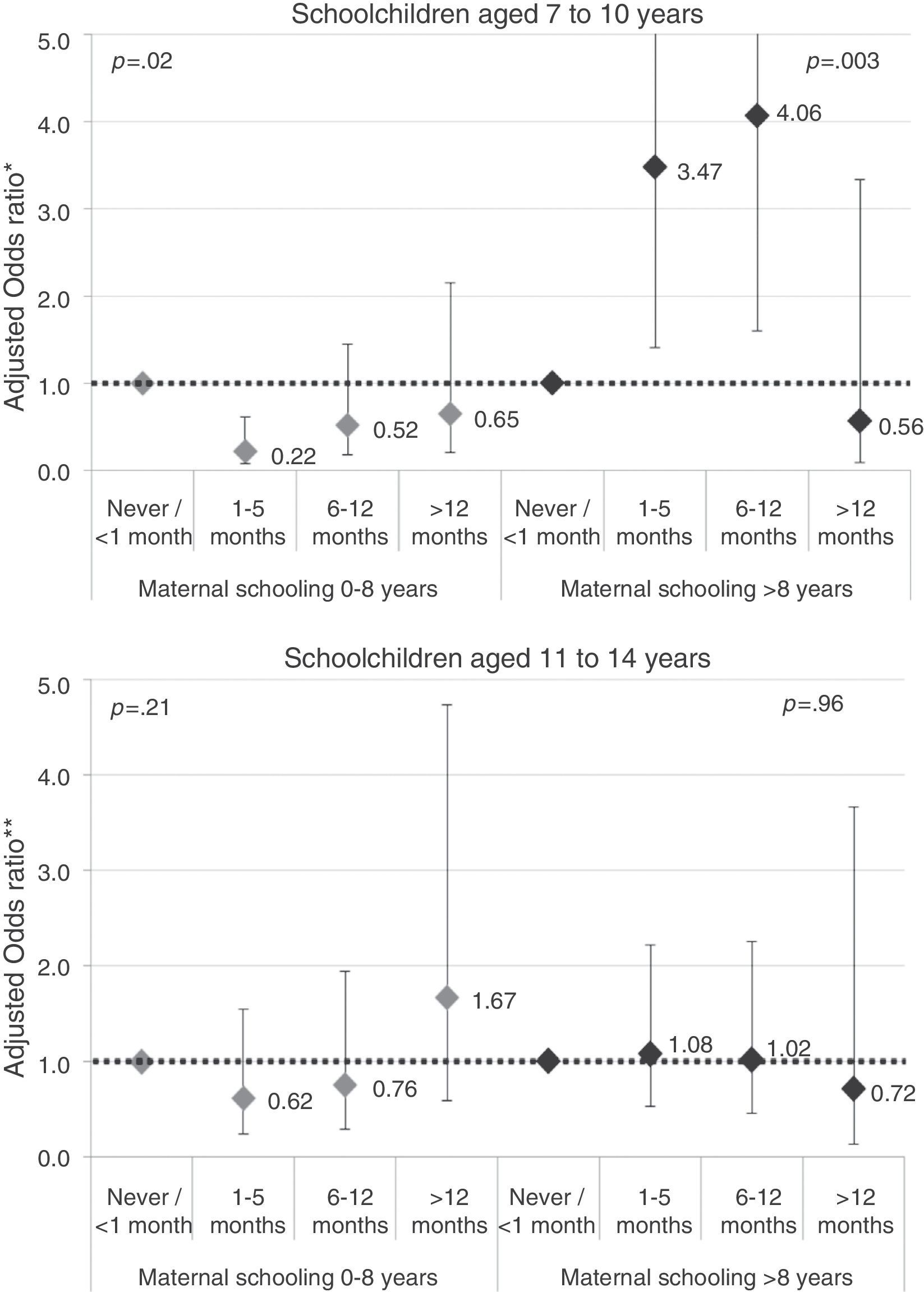
There was evidence of maternal schooling interaction in the association between BF and obesity among children aged 7–10 years. The interaction was observed with both the dichotomous and polytomous exposure (interaction p<0.01 for both analyses). Among schoolchildren aged 7–10 years with mothers with less schooling (0–8 years), BF for any length of time ≥1 month was a protective factor for obesity when compared to those who were breastfed for less than a month or never received it (OR=0.37; 95% CI: 0.15–0.94). In the case of the children of women with higher schooling (>8 years), when the BF was evaluated as a dichotomous variable, it was associated with higher chances of obesity (OR=3.43; 95% CI: 1.49–7.88). When assessing BF as polytomous variable (Fig. 2), the chance of obesity was 78% lower (OR=0.22; 95% CI: 0.08–0.62) among children of women with less schooling who were breastfed for 1–5 months, but the protective effect was also evident with longer periods of BF (p=0.02) (Fig. 2). Among children of women with more schooling, children breastfed for more than 12 months had a lower odds of obesity (OR=0.56; 95% CI: 0.09–3.33), while children who were breastfed for periods of 1–12 months showed a four-fold higher probability than the reference category (p=0.003). In the age group of 11–14 years, no statistical association was found between breastfeeding and obesity, regardless of maternal schooling (interaction p>0.2 with the two exposure variables).
Association between maternal breastfeeding and obesity according to breastfeeding duration categories, stratified by age and maternal schooling. Florianópolis, SC, 2007. * Adjusted for gender, maternal nutritional status and birth weight. ** Adjusted for gender, maternal nutritional status, maternal education, gestational age at birth and sexual maturation.
Interaction analyses were also performed with the variable per capita income and maternal nutritional status; however, no effect modification was observed (data not shown). All analyses were repeated using obesity classified according to the criteria of the International Obesity Task Force (IOTF) as outcome,19 which yielded similar results to those previously described (data not shown).
DiscussionIn the present study, the prevalence of obesity in the sample was 8.6%, being 10.5% among schoolchildren aged 7–10 years and 6.7% in the age group of 11–14 years. These findings corroborate those by the Household Budget Survey (HBS) 2008/2009,1 in which obesity was higher in children aged 7–10 years and lower among adolescents. The overall prevalence of obesity found by the HBS, considering the age group of 5–19 years, was 9.6%, similar to the present study.1
Regarding the prevalence of BF, in this study 55.7% of the sample was breastfed for 6 months or more, and 29.1% of the sample was breastfed for more than 12 months. Considering that the WHO recommends that breastfeeding should be maintained up to 2 years of age or older,20 those durations are below what is recommended. The prevalence of BF in Florianópolis, in spite of the BF distinct methodology, was similar to that found in a national-based population study, which investigated all Brazilian capitals and the Federal District and found that 52.2% of children between 9 and 12 months from Florianópolis were breastfed, the highest prevalence among the capitals of southern Brazil.21
The choice of BF or not and its duration is related to several factors; studies have shown that a longer duration of BF is directly associated with maternal age and family income.22–24 Neither of these variables was associated with BF duration in this study.
The long time of recall on the duration of BF could be responsible for the lack of association with other variables, as the questions on BF were asked at least seven years after the fact occurred. However, literature shows that questionnaires are reliable tools and applicable for the self-reporting of experiences related to breastfeeding, regardless of time of data questioning, and can, therefore, be used in this type of study.3,25
BF in this study was not associated with obesity in the crude and adjusted analyses, and this effect was also maintained when using the classification by Cole et al.19 However, when verifying the interaction of the maternal schooling variable in this association, it was observed that, among schoolchildren aged 7–10 years, the odds of obesity in children of women with less schooling was lower in those breastfed for a month or more. In children of women higher schooling, the protective effect was evident only in those who received breastmilk for more than 12 months, whereas intermediate periods of BF were associated with higher odds of obesity.
Several systematic reviews have been carried out regarding this association; among them, Arenz et al.26 showed a small, but consistent effect of BF against the risk of obesity in later childhood (OR=0.78; 95% CI: 0.71–0.85). The WHO3 also performed a systematic review in which, in addition to this study,25 three other systematic reviews and two more studies were analyzed. The result of the review indicates a small, but protective effect of BF regarding the prevalence of obesity.
Nevertheless, the literature shows controversial results for this association: some studies found null results,7,8 while others demonstrate that the type and duration of BF protect against obesity.4,5 Among the reasons for the discordant results found in the literature is the heterogeneity of the studies, with differences in the age of the individuals, the research site, and the criteria for BF and obesity assessment.6 Most of the studies were carried out in North America and Western Europe,3 with few studies being performed in lower-income countries, including Brazil–in fact, there are few studies comparing results from high-income countries with results from Brazil. The research performed by Brion et al.12 with cohorts from the UK and Brazil (Pelotas city – RS), with samples aged 9 and 11 years, respectively, found an inverse association between duration of BF and BMI only in the European cohort (β=−0.16; 95% CI: −0.22, −0.09). In Pelotas, however, in addition to not finding an association, there was a trend of BF association with higher BMI (β=0.14; 95% CI: −0.07; 0.36).
In a review of studies published from 2005 to 2012, Lefebvre and John10 concluded that this association is still unclear, especially due to the fact that several confounding factors may influence this association.
In the present study, we tried to adjust the analyses considering the main control variables in the association between BF and obesity, among which are socioeconomic and demographic factors and maternal variables.3 Nevertheless, the associations became evident only when maternal schooling was introduced in the analyses as an effect modifier. The literature shows a lower chance, as well as similar chance of obesity, according to the BF duration.4,7 There have been studies that even indicate a trend of lower chance of obesity as the duration of BF increases, with a dose–response effect in this association,4 a fact that was not observed in this investigation. Moreover, the BF dose–response effect on obesity is more evident for exclusive breastfeeding. The literature indicates that exclusive BF, when maintained for a longer period of time, protects children and adolescents from excess weight, as the composition of breast milk contributes to adequate growth.5,27 However, the exclusive BF variable was not measured in this study, and it was not possible to discuss the differences between the type of breastfeeding and its influence on excess weight.
The higher odds of obesity among children of women with more schooling who stopped breastfeeding before reaching 12 months could be related to the introduction of other types of milk and/or foods with high energy density. This hypothesis is reasonable, considering the increase in the consumption of processed foods by the Brazilian population,28 which could be influencing children's diets after weaning. However, this information was not collected in this study.
We do not know the reasons for the lack of association between BF and obesity in schoolchildren aged 11–14 years, because even after adjustment for sexual maturation, no statistically significant associations were demonstrated. New studies with longitudinal design could help in this issue.
Furthermore, there is the time limitation of the study, in which the prevalence and associations may have been different due to a cohort effect. In Brazil, the BF incentive policies started in the 1990s, and there was an increase in the median breastfeeding time between the period of 1993 and 2004.29,30 Thus, this difference in the schoolchildren's birth period would be a limitation in the analysis and could also explain the effect modification between the two age groups.
In conclusion, we emphasize that there is satisfactory evidence of the several BF benefits, which should be encouraged for the period recommended by the WHO.3 We also emphasize that studies aiming to investigate the effects of BF on the nutritional status of children and adolescents need to consider in their methodology not only the control of confounding factors, but also the possible effect modification by socioeconomic variables. Further studies should be carried out to assess this association, especially in lower-income countries, in addition to the implementation of prospective studies that will allow making a more precise inference, analyzing the association between obesity and exclusive breastfeeding, with the age of introduction of other foods.
FundingConselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) – Process n. 402322/2005-3-Edict MCT/CNPq/MS-SCTIE-DECIT/SAS-DAB 51/2005.
Conflicts of interestThe authors declare no conflicts of interest.