The dysbetalipoproteinemia is a rare genetic disorder which usually requires the presence of a metabolic factor for expression of their phenotype. We report a patient with this disease in an age group different from usual, probably triggered by a postpartum hypopituitarism. This association is described in just a few case reports in the medical literature.
A disbetalipoproteinemia é uma desordem genética rara que usualmente requer a presença de um fator metabólico para a expressão do seu fenótipo. Reportamos uma paciente com esta doença em uma idade diferente da usual, provavelmente desencadeada por um hipopituitarismo pós-parto. Esta associação tem poucos relatos de caso na literatura médica.
Genetic hyperlipidemias are relatively rare, but prompt recognition and treatment can prevent serious complications, such as atherosclerosis. Multiple palmar xanthomas are essential to diagnose dysbetalipoproteinemia (type III hyperlipoproteinemia), an uncommon genetic disorder of the lipoproteins metabolism.1 This rare disease is more frequent in men than women, who usually manifest it after menopause.2 We describe a premenopausal woman whose presenting features of dysbetalipoproteinemia were triggered by postpartum hypopituitarism (Sheehan syndrome).
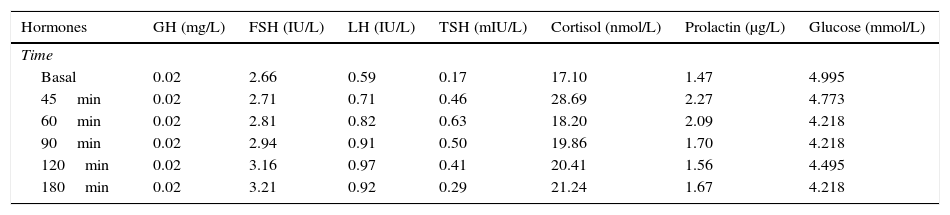
Case reportA 39-year-old woman was referred to the endocrinology outpatient clinic by severe hypercholesterolemia. She had an episode of post partum hemorrhage eight years ago, and since then reported chronic fatigue, weight gain and changes in menstrual cycles. Her gynecologist reported oligomenorrheic cycles during those years and amenorrhea for three consecutive months, when ethinylestradiol plus cyproterone were prescribed. She was taking these hormones in the last six months. She denied alcohol abuse or cigarette smoking, and underwent cholecystectomy for gallstones. Physical examination showed BMI of 28.7 and xanthomas striata palmaris on both hands (Panel A, Fig. 1). Xanthelasma palpebrarum was not seen in her eyelids. All medications were stopped, and a laboratory workup showed total cholesterol (TC) of 15.51mmol/L, and triglycerides (TG) of 21.18mmol/L. Lipoprotein electrophoresis depicted alpha lipoproteins (HDL) 11.2% (22.3–53.3%); pre-beta lipoproteins (VLDL) 51.9% (4.4–23.1%); beta lipoproteins (LDL) 36.9% (38.6–69.4%), confirming the diagnosis of dysbetalipoproteinemia. Blood glucose levels, urinalysis, serum aspartate aminotransferase, and alanine aminotransferase were normal. Free thyroxine (T4): 1.67pmol/L (6.94–15.95pmol/L); cortisol: 16.55nmol/L (149–690nmol/L); follicular stimulant hormone (FSH): 2.66IU/L (23–116IU/L); luteinizing hormone (LH): 0.59IU/L (15.90–54IU/L); prolactin: 1.9μg/L (1.9–25μg/L); growth hormone (GH): <0.02mg/L (<5mg/L); IGF-1: 65.3μg/L (101–267μg/L); ACTH: 1.98pmol/L (2.2–13.2pmol/L). Sella turcica magnetic resonance image (MRI) was normal. A hormonal profile after insulin plus TRH (thyrotropin releasing hormone) plus GnRH (gonadotropin-releasing hormone) was carried out; although hypoglycemia has not been obtained, the test was highly suggestive of pituitary hormonal deficiencies (Panel B, Table 1). Transvaginal ultrasound showed uterus and ovaries compatible with the patient's age. Echocardiogram showed mild hypertrophy of the left ventricule and mild mitral insufficiency. Doppler of carotid arteries did not show any significant abnormalities. She was treated with levothyroxine 88mcg/day, prednisone 5mg/day, atorvastatin 40mg/day, and ciprofibrate 100mg/day. After six months of follow-up, there was clinical improvement, complete resolution of the xanthomas palmaris and marked improvement of the lipid profile (TC: 4.06mmol/L; HDL: 1.42mmol/L; LDL: 1.52mmol/L; TG: 2.44mmol/L).
Panel B: hormonal profile after TRH plus GnRH plus insulin infusion.
| Hormones | GH (mg/L) | FSH (IU/L) | LH (IU/L) | TSH (mIU/L) | Cortisol (nmol/L) | Prolactin (μg/L) | Glucose (mmol/L) |
|---|---|---|---|---|---|---|---|
| Time | |||||||
| Basal | 0.02 | 2.66 | 0.59 | 0.17 | 17.10 | 1.47 | 4.995 |
| 45min | 0.02 | 2.71 | 0.71 | 0.46 | 28.69 | 2.27 | 4.773 |
| 60min | 0.02 | 2.81 | 0.82 | 0.63 | 18.20 | 2.09 | 4.218 |
| 90min | 0.02 | 2.94 | 0.91 | 0.50 | 19.86 | 1.70 | 4.218 |
| 120min | 0.02 | 3.16 | 0.97 | 0.41 | 20.41 | 1.56 | 4.495 |
| 180min | 0.02 | 3.21 | 0.92 | 0.29 | 21.24 | 1.67 | 4.218 |
Dysbetalipoproteinemia is a rare lipid disorder characterized by high levels of serum cholesterol and triglycerides.1–3 Cholesterol levels usually range from 300 to 600mg/dL. Triglycerides concentrations are usually greater than 400mg/dL and may exceed 1000mg/dL. HDL cholesterol levels may be normal or decreased. The disorder develops because both, a decreased ability to convert very low-density lipoprotein (VLDL) and intermediate-density lipoprotein (IDL) to low density lipoprotein (LDL) particles in the blood, and a decreased clearance of chylomicron remnants.2,4
Dysbetalipoproteinemia primarily affects older adults (men more than women) and is rare in children and premenopausal women.1 Estrogen therapy increases the clearance of VLDL remnants, improving dysbetalipoproteinemia in some postmenopausal women.
More than 90% of patients with dysbetalipoproteinemia are homozygous for apoE2.5 Homozygosis for the apoE2 isoform occurs at a frequency of about 1 in 100 in the general population. Despite this high frequency, dysbetalipoproteinemia is relatively rare, occurring in about 1 in 20 apoE2 homozygotes, with an overall prevalence of 1 in 10,000.6,7
Clinical manifestations of this hyperlipoproteinemia appear to require the presence of a secondary factor, such as a metabolic derangement.6 It can be caused by lipoprotein overproduction syndromes, such as obesity, diabetes mellitus, or alcohol abuse,4,5,8 or by disorders that further impair lipoprotein clearance, such as hypothyroidism.5,6,8 In conditions characterized by VLDL overproduction, the increased generation of remnant particles through catabolism of VLDL overwhelms the ability to clear these remnants from the plasma. Because the clinical manifestations are highly sensitive to factors that increase hepatic lipoprotein production, this disorder is usually responsive to therapeutic modalities directed at decreasing hepatic lipoprotein production, such as dietary modifications, weight loss, and alcohol consumption cessation.5
All patients with lipoprotein disorders should undertake a comprehensive clinical evaluation for the presence of corneal arcus, corneal opacification, xanthelasma palpebrarum, and xanthomas in the extensor tendons, including palms, elbows, knees, and Achilles tendons.9 Xanthomas are skin lesions that are present in more than half of affected subjects. Xanthomas palmaris are orange-yellow discolorations of the palmar creases, considered pathognomonic for dysbetalipoproteinemia,4,7 but found in only 20% of patients.5
In the absence of palmar or tuberous xanthomas, the specific diagnosis is more difficult and requires lipoprotein electrophoresis to demonstrate the broad beta-band that denotes beta-VLDL.4 The VLDL cholesterol/triglycerides ratio is a useful screening test as well; in type III hyperlipoproteinemia, when hyperlipidemia is present, this ratio is usually greater than 0.3.4 The normal VLDL cholesterol/triglycerides ratio is typically about 0.2.5
Dysbetalipoproteinemia accounts for 1.0% of the lipid disorders associated with myocardial infarction.10 Thus, a careful history should be obtained to find out other modifiable risk factors for atherosclerosis, such as smoking and hypertension. Peripheral vascular disease is as prevalent as coronary artery disease in this patient's group.4 Because this disorder is most commonly autosomal recessive, there is often no family history of hyperlipidemia or premature cardiovascular disease. First-degree relatives should be screened for hyperlipidemia as well as have their risk stratified for cardiovascular diseases.
Patients should be aggressively treated to decrease the risk of cardiovascular disease.1 Dysbetalipoproteinemia has a good therapeutic response to lipid lowering agents. Drugs of choice for severe hypertriglyceridemia include fibric acid and high-dose omega-3 fatty acids.1 Although statins are not the drugs of choice to treat dysbetalipoproteinemia, their use may be necessary if the response to a fibrate is poor.
We describe a patient in that a careful history and physical examination were essentials to make the correct diagnosis and to identify the underling etiology of dysbetalipoproteinemia. Xanthoma striata palmaris is pathognomonic and can be the only apparent sign of a potentially ominous disease.11 Thus, its clinical recognition is paramount, and should direct the work-up for dysbetalipoproteinemia.6 The obstetric history of this patient suggested the diagnosis of Sheehan syndrome, hypopituitarism with cortisol and growth hormone deficiencies, and secondary hypothyroidism. These hormonal deficiencies could have accelerated systemic atherosclerosis.3 She was treated with hormonal replacement therapy, atorvastatin, and ciprofibrate with improvement of the lipid profile. As a premenopausal woman she has developed this disease in an unusual age. As far as we known, there are only two case reports in the literature with the association of Sheehan syndrome and dysbetalipoproteinemia.3,7 Despite our patient had no known cardiovascular disease, she was encouraged to begin an aerobic exercise program and to engage a healthy diet oriented by a certified nutritionist.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Conflicts of interestThe authors have no conflict of interest to declare.