Continuation and maintenance electroconvulsive therapy (c/m-ECT) is a therapeutic option after an acute ECT course. Although it is widely used, both duration and the outcome of patients when ECT-c/m is discontinued is not yet well established. The aim of the study was to evaluate the recurrence rate and associated clinical factors when c/m-ECT is discontinued.
Materials and methodsRetrospective evaluation of 73 patients who were discontinued from c/m-ECT. The minimum evaluation time was one year. The need of hospital admission or a new acute course of ECT was considered a relapse. The recurrence rate was calculated as a percentage and the estimated time to recurrence was analyzed through a survival analysis. Possible associations between clinical variables and recurrence were analyzed by univariate and multivariate Cox analysis.
ResultsThirty-six patients (49.3%) relapsed: 61.1% of them relapsed during the first year after the c/m-ECT discontinuation (36.1% during the first 6 months). The estimated time to recurrence was 38.67 months. Fifty percent of patients who relapsed required a new acute course of ECT and 44.4% of them restarted c/m-ECT. Patients with an interval between sessions of less than one month and those with more previous episodes showed a higher risk of recurrence.
ConclusionsThe risk of recurrence should be considered before the discontinuation of c/m-ECT. After the discontinuation, almost half of the patients relapsed, most of them within the first year. Close monitoring should be conducted in these patients and the discontinuation is not recommended when it is administered at intervals between sessions of less than a month. Further studies are required to identify risk groups for relapse.
La terapia electroconvulsiva de continuación/mantenimiento (TEC-c/m) es una opción terapéutica tras la TEC aguda. Aunque es ampliamente usada, tanto su duración como la evolución de los pacientes tras su discontinuación no están bien establecidas. El objetivo del estudio fue evaluar la tasa de recidivas y los factores clínicos asociados a la misma tras discontinuar la TEC-c/m.
Material y métodosEvaluación retrospectiva de 73 pacientes a los que se les discontinuó la TEC-c/m. El tiempo de evaluación mínimo fue de un año. Se consideró recidiva la necesidad de ingreso o de nueva tanda aguda de TEC. La tasa de recidivas se determinó como porcentaje y el tiempo estimado hasta la recidiva se analizó a través de un análisis de supervivencia. Posibles asociaciones entre la recidiva y variables clínicas se analizaron mediante análisis univariado y multivariado de Cox.
ResultadosTreinta y seis pacientes (49.3%) recidivaron. El 61.1% lo hicieron durante el primer año tras la discontinuación de la TEC-c/m (36.1% durante los primeros 6 meses). El tiempo estimado hasta la recidiva fue de 38.67 meses. El 50% de los pacientes que recayeron precisaron una nueva tanda aguda de TEC y el 44.4% reiniciaron TEC-c/m posteriormente. Los pacientes con un intervalo entre sesiones inferior a un mes y aquellos con más episodios previos presentaron mayor riesgo de recidiva.
ConclusionesAnte la discontinuación de la TEC-c/m debe considerarse el riesgo de recidiva. Tras la discontinuación, casi la mitad de los pacientes recidivaron, la mayoría en el primer año. Es recomendable realizar un seguimiento estrecho tras la discontinuación de la TEC-c/m y no es aconsejable su retirada cuando se administra con intervalos entre sesiones inferiores a un mes Se requieren nuevos estudios para identificar grupos de riesgo para la recidiva.
Electroconvulsive therapy (ECT) is a highly effective treatment for depression, manic episodes and psychosis.1–5 However, the relapse rate (relapses and/or recurrences) after an acute course of ECT is high despite using a correct pharmacological strategy of continuation and maintenance.6–8 Long-term ECT could be a treatment option to maintain remission.9–15
Continuation ECT (C-ECT) is treatment with ECT carried out for the first 6 months, with the aim of preventing recurrence of an episode, and maintenance ECT (M-ECT) is treatment given beyond 6 months, with the aim of preventing a new episode (APA, 2001).9 However despite this distinction, in this manuscript we will refer jointly to continuation/maintenance ECT (C/M-ECT).
Although it is considered that there is no maximum period of time for M-ECT,9 the guidelines do not cover how much time treatment should last, which is why it is recommended to individualise and review the prescription every 6 months.9 Similarly, there is little literature on the progress of patients after discontinuation of C/M-ECT. In the follow-up study at one year after discontinuation of C/M-ECT by Huuhka et al. (2012) a relapse rate of 44% was estimated, all of which occurred in the first 8 months, with a higher risk in patients with a diagnosis other than major depressive disorder.16
The study objectives will be: 1) to study the progress of patients whose C/M-ECT was discontinued, with respect to relapses and time to relapse; and 2) to analyse possible clinical factors associated with relapse, with the aim of identifying risk groups.
Material and methodsSamplePatients >18 years of age in the Corporació Sanitària Parc Taulí of Sabadell were included retrospectively in the study, whose C/M-ECT had been withdrawn over the period between January 2009 and December 2016. For the study, C/M-ECT was considered the administration of ECT for at least one month after clinical recovery with an acute course of ECT (n=85).
Two possible reasons for withdrawal or discontinuation of C/M- ECT were considered: 1) remission for 6 months or more; and 2) other reasons (withdrawal of consent by the patient or other medical reasons, such as increased anaesthetic risk, onset of intercurrent somatic complications or during the procedure or objective cognitive intolerance). In patients who had received C/M-ECT that been discontinued on more than one occasion during the study period (n=7) only the first discontinuation was considered for the analysis. In the end 5 patients were excluded due to a lack of follow-up data: one patient moved to their country of origin, one patient was admitted to another sector’s long-stay unit and 3 patients died due to medical causes shortly after discontinuing treatment with C/M-ECT. A total of 73 patients were included.
The indication for C/M-ECT was established following clinical guidelines, therefore all patients prescribed C/M-ECT, had, at least, responded clinically to a standard course of acute ECT.9,17 ECT (acute and C/M-ECT) was administered to all the patients by means of the Thymatron™ System IV, with bilateral placement (bifrontotemporal). The dose administered at the beginning of the C/M ECT was the same as that used at the end of the acute course. The patients were followed up in their corresponding mental health units, where each psychiatrist determined the frequency of visits. The C/M-ECT sessions were administered at weekly or longer intervals. The intervals between sessions were assessed by the referral psychiatrist and were adjusted individually according to clinical progress. All the patients received concomitant pharmacological treatment during and after the C/M-ECT.
The data collected in the clinical histories were analysed retrospectively. The study protocol was approved by the Ethics Committee of the Corporació Sanitària Parc Taulí of Sabadell.
Clinical variables and follow-up measuresThe demographic data (age and gender), clinical data (diagnosis, presence of psychotic symptoms, age of onset and duration of illness, previous episodes, past use of ECT (number of acute courses and use of C/M-ECT throughout duration of disease), data on the C/M-ECT (reason for withdrawal, age at time of discontinuation, duration of C/M-ECT, number of sessions of C/M-ECT, interval between sessions at time of withdrawal, programme of C/M-ECT) and data on pharmacological treatment (use of antidepressants, antipsychotic drugs, benzodiazepines and/or mood stabilisers) were collected through a review of clinical histories.
The minimum follow-up time for patients was 12 months. Recurrence was considered to be admission to an acute unit or having received a further acute course of ECT (either on an outpatient or an inpatient basis). An acute course of ECT was considered the need to increase the frequency to 2–3 sessions a week, without establishing a minimum number of sessions. Completed suicide was also considered relapse. The date of relapse, in cases where it was not available, was estimated as the date of admission or the start date of acute outpatient ECT or the date of suicide.
Statistical analysisA descriptive analysis was made of the sample. The categorical variables were shown in absolute frequencies and percentages (%) and the quantitative variables were described in means (standard deviation) or medians, as appropriate. The relapse rate (1st relapse —whether relapse or recurrence) was determined as a frequency in percentage (%). A Kaplan-Meier survival analysis was performed to estimate the time to relapse. A univariate Cox analysis was performed to identify potentially influential factors. The variables that showed an association in the univariate analysis (p<.05) were entered into a multivariate Cox regression model. SPSS for Windows v. 19.0 (SPSS, Chicago) was used for the data analysis. A p value <.05 (bilateral) was considered statistically significant.
ResultsCharacteristics of the sampleOf the sample, 56.2% were female (41/73) and the mean age at the time of data collection was 62.21 (±15.08). The follow-up time of the patients was 52.13±26.19 months (13.08–100.99).
Of the patients, 43.8% (32/73) had been diagnosed with an MDD, 27.4% (20/73) with bipolar disorder and 28.8% (21/73) with schizophrenia or another psychotic disorder. Of the sample, 82.2% had had psychotic symptoms (60/73) in the previous acute episode. The (mean) age of onset of the disorder was 34 (13–82) and duration of the disease was 20.97 (±14.68). The median of previous episodes was 4 (1–20). The patients had received a median of 2 acute courses of ECT (1.13) throughout the course of the disease. The mean sessions in the acute course that preceded the indication for C/M-ECT was 11.37 (±4.64).
In 39.7% of the patients (29/73) C/M-ECT was discontinued due to remission of symptoms for 6 months or more. In the rest of the sample, discontinuation was due to situations other than this remission: withdrawal of consent by the patient in 31.5% of cases (mostly due to cognitive complaints and due to non-conformity with treatment requirements) and other medical decisions in 28.8%.
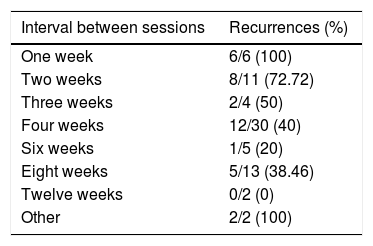
The mean age at the time of discontinuation of C/M-ECT was 57.93 (±15,6). The duration of the C/M-ECT was 12.5 months (1.15–116.11), with a median of 18.5 sessions (4–247). The mean number of sessions per month was 1.85 (±0.85). The interval between C/M-ECT sessions was a median of 4 weeks (1–16): 28.8% of the patients (21/73) received C/M-ECT with an interval of less than one month and the rest (71.2%) with a monthly interval or more. Specifically, the frequency of the sessions was weekly in 8.2% of the patients (6/73), fortnightly in 15.1% (11/73), every 3 weeks in 5.5% (4/73), monthly in 41.1% (30/73), every 6 weeks in 6.8% (5/73), bimonthly in 17.8% (13/73), quarterly in 2.7% (2/2) and other intervals were also used in 2.7% of the patients. C/M-ECT was administered with a pulse amplitude of 1ms in 78.1% of the patients (57/73) and of .5ms in the rest of the cases. The main clinical characteristics, according to the diagnosis group, are specified in the supplementary data (Appendix B Table 1 of Annex 1).
All the patients received concomitant pharmacological treatment with one or more drugs, 75.8% of the patients (50/66) were treated with antidepressants, 84.8% with antipsychotics (56/66), 56.1% with benzodiazepines (37/66), and 47% with mood stabilisers (31/66).
Recurrence rateDuring follow-up, 49.3% of the patients (36/73) relapsed after discontinuing treatment with C/M-ECT. In the patients who relapsed, the mean time to relapse was 13.39±11.78 months (median of 9.95 months [1.38–47.01]).
Of the relapses, 86.1% (31/36) required admission to the acute psychiatric unit, 11.1% (4/36) required a new acute course of ECT on an outpatient basis, and in 2.8% of cases (1/36) the relapse resulted in completed suicide. The percentage of relapses according to the interval of C/M-ECT sessions is specified in Table 1. In total, 50% of the patients who relapsed (18/36) received an acute course of ECT. C/M-ECT was reintroduced in 16 (44.4%) of these patients.
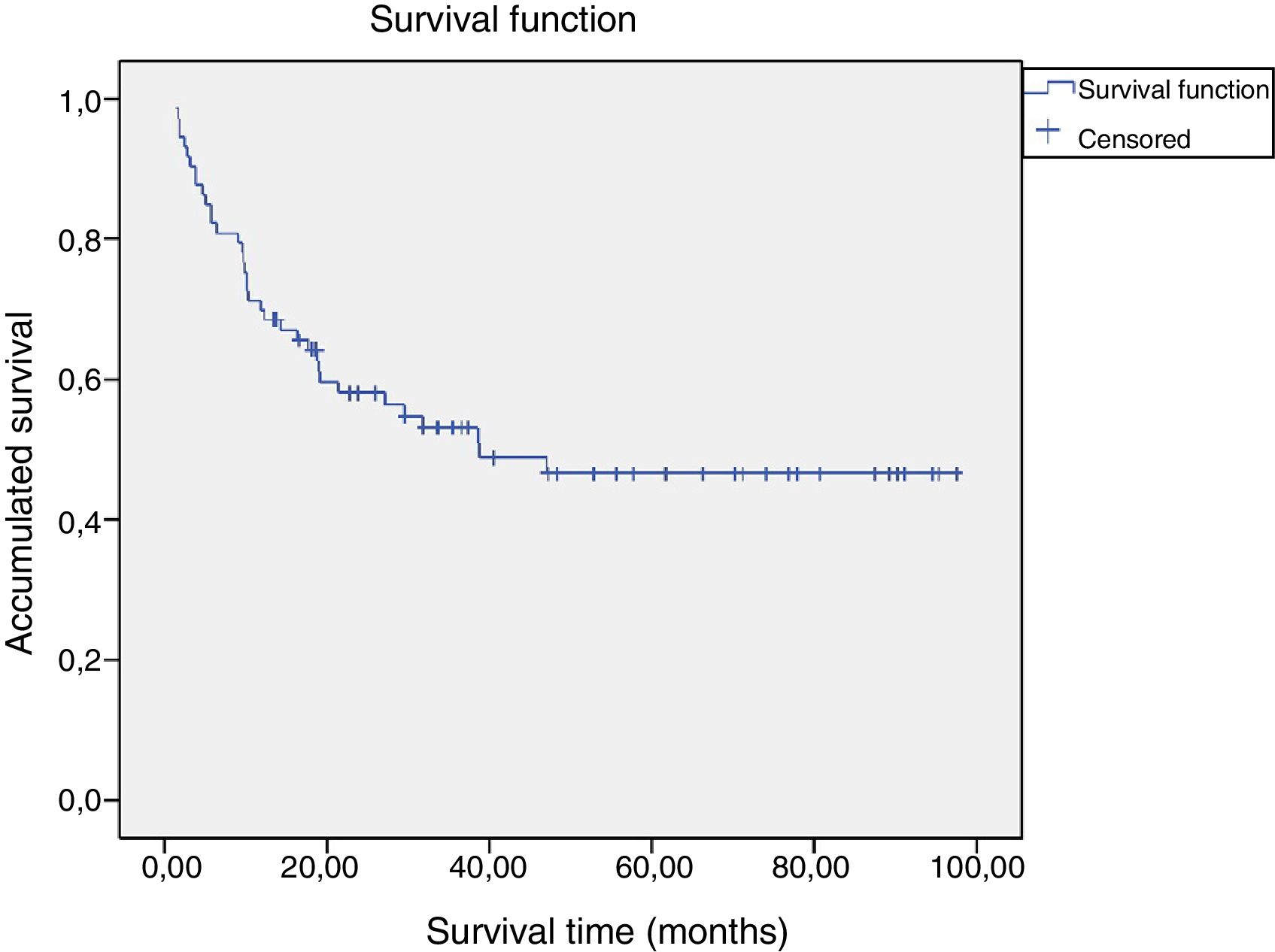
Survival analysisAccording to the survival analysis (Fig. 1), the estimated mean time to recurrence for patients who discontinued treatment with C/M-ECT was 38.67 months (median). Of the patients who relapsed, 36.11% (13/36) did so during the first 6 months and 61.1% (22/36) during the first year after withdrawal of C/M-ECT. The rest of the patients who relapsed did so from the second year following discontinuation: 8 in the second year, 3 in the third year and another 3 in the fourth year. There was no relapse beyond this time (Fig. 1).
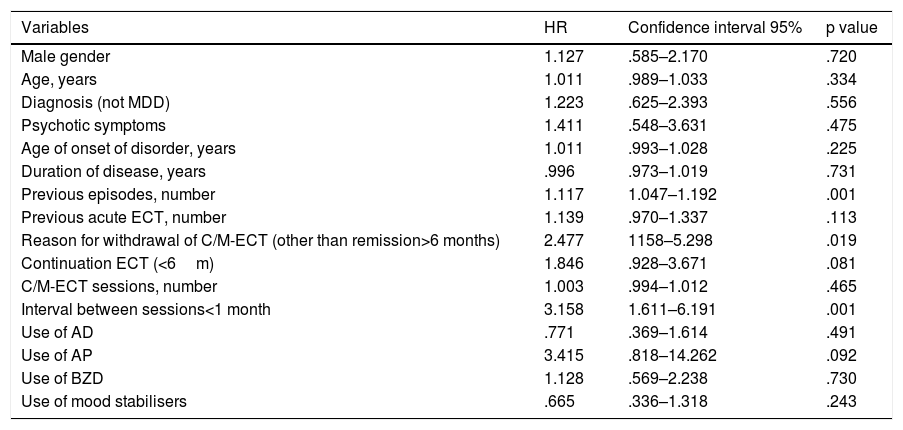
Risk factors for recurrence. Univariate and multivariate Cox analysisIn the univariate Cox analysis (Table 2), the number of previous episodes (HR 1.117; 95%CI: 1.047–1.192; p=.001), reason for discontinuation of C/M-ECT(HR 2.477; 95%CI: 1.158–5.298; p=.019) and the interval between sessions of C/M ECT(HR 3.158; 95%CI: 1.611–6.191, p=.001) influenced relapse. The duration of the C/M-ECT(C-ECT vs M-ECT) and the use of antipsychotics showed a trend that did not exceed the level of significance (HR 1.846; 95%CI: .928–3.671; p=.081 and HR 3.415, 95%CI: .818–14.262; p=.092, respectively). Other clinical and treatment variables, such as gender, age, diagnosis, presence of psychotic symptoms, age of onset and duration of the disorder, past use of ECT or use of other drugs (antidepressants, benzodiazepines or mood stabilisers) did not appear to influence recurrence.
Univariate Cox regression analysis: time to relapse.
| Variables | HR | Confidence interval 95% | p value |
|---|---|---|---|
| Male gender | 1.127 | .585–2.170 | .720 |
| Age, years | 1.011 | .989–1.033 | .334 |
| Diagnosis (not MDD) | 1.223 | .625–2.393 | .556 |
| Psychotic symptoms | 1.411 | .548–3.631 | .475 |
| Age of onset of disorder, years | 1.011 | .993–1.028 | .225 |
| Duration of disease, years | .996 | .973–1.019 | .731 |
| Previous episodes, number | 1.117 | 1.047–1.192 | .001 |
| Previous acute ECT, number | 1.139 | .970–1.337 | .113 |
| Reason for withdrawal of C/M-ECT (other than remission>6 months) | 2.477 | 1158–5.298 | .019 |
| Continuation ECT (<6m) | 1.846 | .928–3.671 | .081 |
| C/M-ECT sessions, number | 1.003 | .994–1.012 | .465 |
| Interval between sessions<1 month | 3.158 | 1.611–6.191 | .001 |
| Use of AD | .771 | .369–1.614 | .491 |
| Use of AP | 3.415 | .818–14.262 | .092 |
| Use of BZD | 1.128 | .569–2.238 | .730 |
| Use of mood stabilisers | .665 | .336–1.318 | .243 |
AD: antidepressants; AP: antipsychotics; BZD: benzodiazepines; MDD: major depressive disorder.
If we include a multivariate Cox regression model, the variables that showed a significant association in the univariate analysis (number of previous episodes, reason for discontinuation and interval between C/M-ECT sessions), a greater number of previous episodes and an interval between C/M-ECT sessions of less than one month influenced relapse (HR 1.080; 95%CI: 1.004–1.161; p=.038 and HR: 2.308, 95%CI: 1.095–4.865; p=.028, respectively).
DiscussionThe aim of the study was to assess the progress of the patients after discontinuation of C/M-ECT, as well as to detect possible risk factors for relapse. In our sample, 49.3% of the patients relapsed on discontinuation of treatment with C/M-ECT (36.11% relapsed during the first 6 months and 61.1% during the first year). As risk factors for relapse, we found that a greater number of previous episodes and the frequency of C/M-ECT before withdrawal (interval between sessions of less than one month) influenced relapse.
The percentage of patients who relapsed after discontinuation of C/M-ECT (49.3%) was similar to the 44% reported by Huuhka et al. (2012) in their study at one year of follow-up.16 This study found that all patients who relapsed did so in the first 8 months,16 whereas in our sample 61.1% did so during the first year. The percentage of relapse observed is also similar to that observed in the first 12 months after completion of an acute course of ECT, regardless of the therapeutic maintenance strategy employed.7,18 In this regard, the 12 months after discontinuation of any treatment would be a period of vulnerability or greater risk of relapse. For this reason, in this window period following discontinuation of C/M-ECT, it would be advisable to closely monitor and include psychoeducational programmes in the clinical approach aimed at detecting warning signs and symptoms of relapse.
In our study, the presence of previous episodes influenced relapse after discontinuing C/M-ECT. This finding is in line with the risk factors identified for relapse after acute ECT.19 Similarly to MDD, bipolar disorder and schizophrenia, a greater number of previous episodes tends to increase the risk of relapse and subsequent recurrence.20–22 Therefore, we consider that, as with discontinuation of other therapeutic modalities, the number of episodes should be considered when deciding to discontinue C/M-ECT.
Most guidelines state that the interval between sessions of C/M-ECT should be increased (e.g. weekly, fortnightly or monthly) until the minimum frequency of treatment administration compatible with sustained remission is identified.9,17 In the consensus on M-ECT by Gill and Kellner (2019), the authors recommend attempting to space sessions if the patient is stable over a prolonged period of time.11 In our sample the interval between sessions of less than one month influenced relapse after discontinuation of C/M-ECT, a fact that might suggest that, in these patients, the clinical improvement obtained after acute ECT was not sufficiently established at the time of discontinuation. This result would indicate that before considering discontinuation or withdrawal of C/M-ECT it would be advisable to ensure that the patient has achieved sufficiently solid clinical stability, which would be determined by reaching a minimum frequency of one month or more.
In our sample, other clinical or treatment characteristics, identified as risk factors for relapse after acute ECT, such as gender,23 the presence or absence of psychotic symptoms24 or treatment with benzodiazepines or antipsychotics,25 do not appear to influence relapse. Nonetheless, our results would be in line with other studies, performed mainly in MDD, in which no risk factors for relapse have been identified among the clinical and socio-demographic variables analysed.26–28
The following limitations must be considered when interpreting our results. In the first place, it is a retrospective study, with a review of histories and administrative data and without semi-structured diagnostic interviews or systematic clinical scales. Likewise, the patients were followed up in their corresponding mental health centres, and therefore the frequency of follow-up visits was not the same for all patients. In order to be more objective, only admission to a psychiatric unit or the need to undergo a new acute course of ECT was considered a relapse. This fact could have meant that the analysis did not include relapses that were resolved on an outpatient basis, without the need for admission or a new acute course of ECT. Likewise, the fact of considering the date of relapse, in cases where it was not available, as the date of admission or of starting acute ECT, might have contributed to a longer time to relapse. C/M-ECT was performed bilaterally, which could make it difficult to generalise the results to other modalities of ECT. Finally, it is worth noting that we studied a sample of a relatively small size. However, the difficulty in conducting randomised controlled studies in patients treated with ECT enhances the value of retrospective studies in clinical practice.
In conclusion, almost half of the patients had a relapse after discontinuing C/M-ECT, most in the first year. This risk must be taken into account when considering the withdrawal of C/M-ECT and close and individualised follow-up of these patients should be ensured, especially those with previous episodes and with an interval between sessions of less than one month. Withdrawal of C/M-ECT is not recommended if the administration frequency is less than one month. More studies are needed to identify risk groups for recurrence. A specific programme for monitoring these patients needs to be defined.
Conflict of interestsNone.
The authors would like to thank Dr Joan Carles Oliva for his contribution to the statistical analysis, and all the subjects of the study, and the staff of the Psychiatric Department of the Corporació Sanitària Parc Taulí de Sabadell.
Please cite this article as: Martínez-Amorós E, Serra P, Goldberg X, Urraca L, Palao DJ, Urretavizcaya M, et al. Evolución clínica tras la discontinuación de la terapia electroconvulsiva de mantenimiento. Estudio de seguimiento retrospectivo. Rev Psiquiatr Salud Ment (Barc.). 2020;13:5–10.