Although combining medications for the treatment of schizophrenia is the rule rather than the exception, the literature and treatment guidelines consistently direct clinicians away from this practice, emphasizing that antipsychotic polypharmacy/combination treatments are associated with higher medication costs, more side effects, and no clearly documented improvement in efficacy and in fact, worse outcomes.1–17 However, the tide may be beginning to turn in favor of antipsychotic polypharmacy for selected patients. Who are these patients and what are the emerging guidelines for using antipsychotic polypharmacy?
Which are the patients who do not respond to antipsychotic monotherapy?Although it is clear that patients with schizophrenia should initially try a series of monotherapies including clozapine as first-line treatments, what about patients who do not respond to monotherapy? A dozen suggestions are outlined in Table 1 for what to do, based upon clinical experience as well as clinical trials.15–21 Much of the existing evidence base for and against antipsychotic polypharmacy is elegantly reviewed in two recently published comprehensive volumes.16,17 This body of data tells us is that while evidence-based practice indeed supports antipsychotic monotherapy as the best trade-off between risks and benefits for first line treatment of schizophrenia, a close look at the specific patient populations from published studies supporting monotherapy shows that these are patients with schizophrenia who are generally not too disabled to give informed consent for treatment; not so violent nor aggressive to be unable to cooperate; not active current substance abusers; and without a long history of failing to respond to numerous monotherapies at adequate doses and durations of treatment. Real world psychiatrists, however, have to treat schizophrenic patients who do not respond to numerous monotherapies, who have uncontrolled impulsivity, violence, aggression and active substance abuse, who are increasingly housed long-term on forensic units or prisons following commission of violent crimes, and/or who may have borderline, affective, and even antisocial psychopathic features. Do such patients fare poorer with polypharmacy/augmentation because they receive this treatment, or do they receive this treatment because they fare even more poorly on monotherapy?22 When patients do not fare well even on clozapine, do they respond to polypharmacy?4 When patients are switched off polypharmacy and onto monotherapy, a third of them relapse and have to go back to polypharmacy.23 For these difficult patients with schizophrenia, some of the selected studies combined with real world clinical experience–also called practice-based evidence–now point to the efficacy of very high doses of antipsychotics as monotherapies or to combinations of two antipsychotics or to combinations of an antipsychotic with another agent, often a mood stabilizer.15–21 How does one apply these controversial treatment options?
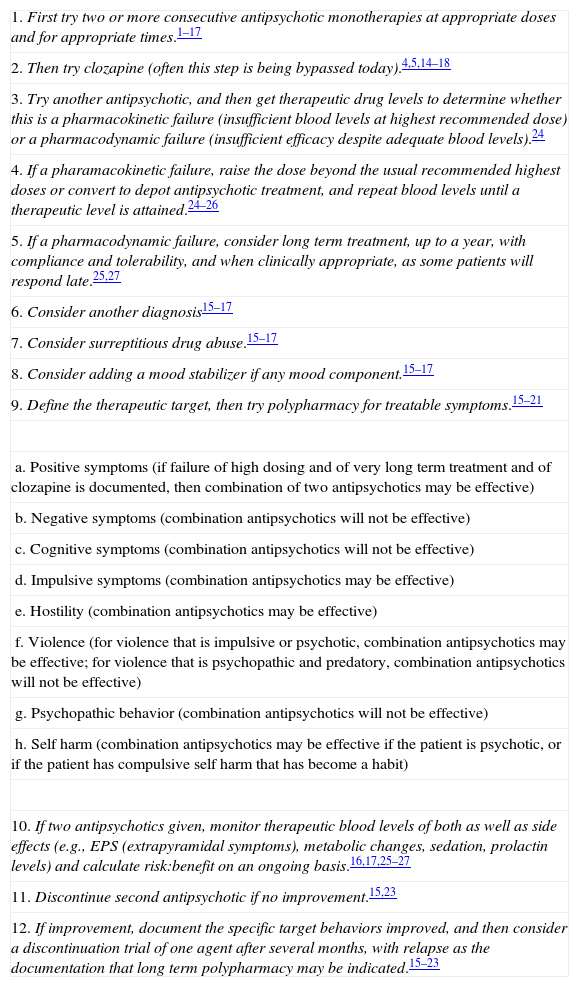
The journey from antipsychotic monotherapy to antipsychotic polypharmacy: a dozen suggestions.
| 1. First try two or more consecutive antipsychotic monotherapies at appropriate doses and for appropriate times.1–17 |
| 2. Then try clozapine (often this step is being bypassed today).4,5,14–18 |
| 3. Try another antipsychotic, and then get therapeutic drug levels to determine whether this is a pharmacokinetic failure (insufficient blood levels at highest recommended dose) or a pharmacodynamic failure (insufficient efficacy despite adequate blood levels).24 |
| 4. If a pharamacokinetic failure, raise the dose beyond the usual recommended highest doses or convert to depot antipsychotic treatment, and repeat blood levels until a therapeutic level is attained.24–26 |
| 5. If a pharmacodynamic failure, consider long term treatment, up to a year, with compliance and tolerability, and when clinically appropriate, as some patients will respond late.25,27 |
| 6. Consider another diagnosis15–17 |
| 7. Consider surreptitious drug abuse.15–17 |
| 8. Consider adding a mood stabilizer if any mood component.15–17 |
| 9. Define the therapeutic target, then try polypharmacy for treatable symptoms.15–21 |
| a. Positive symptoms (if failure of high dosing and of very long term treatment and of clozapine is documented, then combination of two antipsychotics may be effective) |
| b. Negative symptoms (combination antipsychotics will not be effective) |
| c. Cognitive symptoms (combination antipsychotics will not be effective) |
| d. Impulsive symptoms (combination antipsychotics may be effective) |
| e. Hostility (combination antipsychotics may be effective) |
| f. Violence (for violence that is impulsive or psychotic, combination antipsychotics may be effective; for violence that is psychopathic and predatory, combination antipsychotics will not be effective) |
| g. Psychopathic behavior (combination antipsychotics will not be effective) |
| h. Self harm (combination antipsychotics may be effective if the patient is psychotic, or if the patient has compulsive self harm that has become a habit) |
| 10. If two antipsychotics given, monitor therapeutic blood levels of both as well as side effects (e.g., EPS (extrapyramidal symptoms), metabolic changes, sedation, prolactin levels) and calculate risk:benefit on an ongoing basis.16,17,25–27 |
| 11. Discontinue second antipsychotic if no improvement.15,23 |
| 12. If improvement, document the specific target behaviors improved, and then consider a discontinuation trial of one agent after several months, with relapse as the documentation that long term polypharmacy may be indicated.15–23 |
The paradigm for treating schizophrenia is shifting from discouraging all uses of polypharmacy/combinations, to determining instead who should get polypharmacy/combinations (Table 1).15–21 Treatment guidelines are now required for this. It would be ideal to have more studies of polypharmacy/combinations in well-defined patient subtypes in order to help develop these guidelines, but it is not likely that there will ever be any randomized, multicenter placebo controlled trials for the most difficult patients because of ethical and pragmatic barriers to their study. Perhaps developing an expert consensus from case-based medicine and practice-based evidence is the best approach for now.15–21 I am impressed with the therapeutic benefits of antipsychotic high dose, polypharmacy/combinations in selected cases of treatment resistance and violence, and have even included in a recent case book a few such cases from a forensic psychiatry facility where I consult (Patton State Hospital in San Bernardino, California) and who had good outcomes from high dose polypharmacy/combination treatment.18–21
A dozen suggestions for using antipsychotic polypharmacy (see Table 1)First, try monotherapiesFollow existing guidelines for first line treatments of schizophrenia, meaning use two or more antipsychotics, usually two different and sequential atypical antipsychotics, and then maybe a conventional antipsychotic.1–17
Don’t forget clozapineToo often this treatment option is bypassed, and there is a need to revitalize the use of clozapine in some of the treatment settings before proceeding to more heroic measures.4,5,14–18
Get therapeutic blood levelsThe only way to determine whether the patient's lack of treatment response is a pharmacokinetic failure (i.e., blood levels low), or a pharmacodynamic failure (i.e., inadequate treatment response despite adequate blood levels) is to get therapeutic drug levels of the antipsychotic,24 something which is done rarely in most psychiatric settings. Trying to figure out what is going on without therapeutic drug monitoring is like trying to drive at night without your headlights on.
Block at least 60% of D2 receptorsSince no antipsychotic (except perhaps clozapine) has been shown to be effective if fewer than 60% of dopamine D2 receptors are blocked,25,26 it is critical to attain a therapeutic drug level consistent with blocking of at least this number of D2 receptors. In the absence of clinically available PET (positron emission tomography) scans for individual patients, the next best thing is to rule out a pharmacokinetic failure in a monotherapy patient who is not responding to standard doses of antipsychotics by using therapeutic drug monitoring and in cases of low plasma drug levels despite adequate dosing, high or even very high doses are called for, and in this context are not really high, but merely adequate for that patient.24–26
Time is a drugSome patients respond much better to an antipsychotic after many months of treatment, and in cases of inadequate response where the situation is not urgent, consider giving very long treatment periods of a monotherapy, especially an atypical antipsychotic.25,27
Are you sure the diagnosis is schizophrenia?Repeated failure to respond to adequate monotherapy having ruled out pharmacokinetic failure means re-considering other medical and neurological illnesses, drug abuse or personality disorders, which do not respond to antipsychotics.15
Consider surreptitious drug abusePatients who are activating their symptoms due to undetected substance abuse can sabotage monotherapy trials.15–17
Consider adding a non-antipsychotic to an antipsychoticFor patients with affective symptoms, consider an antidepressant, mood stabilizer, lithium or even a short-term benzodiazepine, and document clear improvement without unacceptable side effects as a criterion for continuing this approach as well.16,17
Define the therapeutic target, then try polypharmacy with two antipsychoticsSome symptoms such as negative and cognitive symptoms of schizophrenia are not responsive to antipsychotics, whereas treatment resistant positive symptoms and impulsive and hostile symptoms can definitely be responsive both to high dosing and polypharmacy. Although psychotic and impulsive violence may be responsive to high degrees of D2 occupancy,21–27 psychopathic/predatory violence is not. If you don’t know where you are going, no road will take you there, so define potentially treatable therapeutic targets prior to instituting polypharmacy with two agents. One of these agents may need to be a depot antipsychotic to assure compliance and a foundation of consistent daylong D2 receptor occupancy by one of the agents, with the second agent being given to “top up” the first, aiming for blockade of more than 60% D2 receptors. Demonstrating clear clinical improvement without unacceptable side effects should be a criterion for continuing this approach.
Monitor drug levels of both antipsychoticsTo document compliance and the desired goal of high degrees of receptor occupancy, it is prudent to monitor the therapeutic blood levels of both agents.24
Discontinuation trialAlthough it is tempting to leave well enough alone if the heroic and possibly controversial polypharmacy intervention is selected, it may be prudent nevertheless to attempt a trial at conversion to monotherapy just to prove that long-term polypharmacy/combinations are necessary.15,23 In the Essock et al.23 study, for example, two-thirds of the patients successfully switched to monotherapy, thus documenting the need for return to long-term polypharmacy in the other one-third.
Reinstitute polypharmacy long term if relapse documentedOn the other hand, relapse when switching to one agent is justification for long term maintenance treatment with two antipsychotics.15–17,23
We should grasp this opportunity to debate the issue of antipsychotic polypharmacy, and define treatment guidelines to improve the treatment of schizophrenia by defining who are the candidates for polypharmacy/augmentation, rather than continuing to try to deny this approach to everyone.
Please cite this article as: Stahl SM. Nuevas guías para el uso de la polifarmacia antipsicótica. Rev Psiquiatr Salud Ment (Barc.). 2013;6:97–100.