Hyperventilation in electroconvulsive therapy sessions has been associated with seizure threshold, seizure characteristics, and cognitive effects. There is no consensus on the optimal procedure of applying hyperventilation manoeuvres during electroconvulsive therapy.
Material and methodsProspective evaluation of the effects of systematic use of hyperventilation manoeuvres with facial mask and capnography (protocolised hyperventilation [pHV]), on ventilation parameters and on seizures. The study included a sample of 130 sessions (65 performed according to hyperventilation standard practice and 65 successive sessions, with pHV) of 35 patients over a period of 10 weeks.
ResultsThe pHV manoeuvres reduced exhaled CO2 and increased O2 saturation significantly (p<0.001). The average CO2 reduction achieved was 6.52±4.75mmHg (95% CI −7.7 to −5.3). The CO2 values after pHV correlated significantly with seizure duration and O2 values, with other electroencephalographic quality indices. In pHV sessions, compared with sessions performed according to hyperventilation standard practice, the average lengthening of the motor and electroencephalographic seizure was 3.86±14.62 and 4.73±13.95s, respectively. No differences were identified in other ictal quality parameters.
ConclusionsThe proposed pHV manoeuvres significantly modify ventilation parameters. The hypocapnia and hyperoxia obtained by applying these manoeuvres lengthen the duration of seizures without worsening the quality of the electroencephalographic trace. The use of pHV is generalisable and might improve electroconvulsive therapy procedure without adding costs.
La hiperventilación en las sesiones de terapia electroconvulsiva se ha relacionado con el umbral convulsivo, las características de la convulsión y los efectos cognitivos. No existe consenso sobre el procedimiento óptimo de aplicación de las maniobras de hiperventilación durante la terapia electroconvulsiva.
Material y métodosEvaluación prospectiva de los efectos del uso sistematizado de maniobras de hiperventilación con mascarilla facial y capnografía (hiperventilación reglada [HVr]) en los parámetros ventilatorios y de la convulsión. Muestra de 130 sesiones (65 realizadas con hiperventilación según la práctica habitual y 65 sucesivas con HVr) de 35 pacientes en un periodo de 10 semanas.
ResultadosLas maniobras de HVr disminuyeron el CO2 espirado e incrementaron la saturación de O2 significativamente (p<0,001). La disminución media de CO2 alcanzada fue de 6,52±4,75mmHg (IC 95% −7,7 a −5,3). Los valores de CO2 tras la HVr correlacionaron significativamente con la duración de la convulsión, y los de O2, con otros índices electroencefalográficos de calidad. En las sesiones con HVr, en comparación con las sesiones realizadas con hiperventilación según la práctica habitual, el alargamiento medio de la convulsión motora y electroencefalográfica fue de 3,86±14,62 y de 4,73±13,95s, respectivamente, sin diferencias en los demás parámetros ictales.
ConclusionesLas maniobras de HVr propuestas modifican de forma relevante los parámetros ventilatorios. La hipocapnia y la hiperoxia obtenidas al aplicar estas maniobras alargan la duración de las convulsiones sin empeorar la calidad del trazado electroencefalográfico. El uso de protocolos de HVr es generalizable y puede mejorar el procedimiento de la terapia electroconvulsiva sin añadir costes.
The conditions for providing electroconvulsive therapy (ECT) influence the outcome of treatment and its side effects. Along these lines, we have studied the parameters related to electrical stimulation such as the charge, the pulse amplitude, the location of the electrodes and the influence of different anaesthetics. Available evidence of the ideal characteristics for ventilatory support during ECT is scarce. In the literature on the ECT procedure and current clinical practice guidelines,1–5 pre-oxygenation with elevated oxygen levels (O2) is recommended for monitoring and to provide ventilatory assistance with slight hyperventilation to promote seizure and avoid the risk of hypoxia during the procedure. There has been no consensus as to specific protocols for the application of hyperventilation, including duration, type of manoeuvres, and optimum carbon dioxide (CO2) values required. In usual clinical practice, hyperventilation is usually at the discretion of the anaesthesiologist who runs the ECT session. Hyperventilation has been proposed as a method for optimising seizure,2,6,7 since this is associated with a need for smaller charges8–10 and longer crises obtained.8,10–13 In addition, hyperventilation has been associated with an improvement in the cognitive effects associated with ECT, since it produces shortened reorientation time13 and a decrease in the incidence of postictal delirium.8
Capnography consists of the non-invasive measurement of partial CO2 pressure and, through end-tidal CO2 (EtCO2), or maximum CO2 concentration at the end of each exhalation, provides instantaneous ventilation, perfusion and metabolism of CO2. EtCO2 measurements correlate closely with arterial CO2 values in patients with no lung disease14 and are an early sign of potential respiratory adverse effects, such as airway obstruction, respiratory failure, hypoventilation, or apnea.15–19 Monitoring EtCO2 with capnography during ECT has been associated with maintenance of lower CO2 values during the procedure and more adequate control of haemodynamic parameters.20
The objective of this study is to evaluate the effects of manual hyperventilation manoeuvres with facial masks monitored by capnography, applied in a systematised and reproducible way, which we shall call reflex hyperventilation (rHV). The main objective is to analyse the changes in the ventilatory parameters produced in the sessions where the RHV manoeuvres are used, on the hypothesis that these will decrease EtCO2 values. In order to study the clinical repercussion of rHV, as a secondary objective, we have defined the exploration of the effects of these manoeuvres on the characteristics of the seizure obtained, as compared to the application of hyperventilation following the usual practice.
Materials and methodsProspective assessment of a sample of ECT sessions given over a period of 10 weeks (January–March 2014) in the ECT unit of the Psychiatry Service at the University Hospital of Bellvitge. The indication of ECT was run in all patients by a referring psychiatrist, following the guidelines of good clinical practice.
Patients over 18 years with stable conditions of ECT administration (with no change in charge, anaesthetic dose, concomitant psychoactive drugs or number of days between sessions) were included in a minimum of 2 sessions prior to inclusion in the study. Patients who might be at risk were excluded from hyperventilation (e.g. patients with COPD (chronic obstructive pulmonary disease), those undergoing bronchodilator treatment and pregnant women); sessions where valid baseline EtCO2 measurements were not obtained; sessions where vasoactive drugs were used; and sessions requiring re-stimulation or changes in the conditions of ECT administration.
A total of 274 ECT sessions were run in 37 patients. Two patients were excluded for pneumopathy and 120 sessions for not fulfilling the inclusion criteria.
The 2 forms of hyperventilation were applied on each patient in 2 consecutive sessions. In all cases the order of application was hyperventilation, following the usual practice, in the first place, followed by RHV in the following session with the same parameters as for ECT. Thirty patients were included on 2 occasions and 5 patients on one single occasion, the latter in order to complete ECT treatment before the end of the study period. A total of 130 ECT sessions were analysed, 65 sessions run with hyperventilation manoeuvres, following the usual practice, and 65 with rHV, using facial masks and capnography.
The study was approved by the Clinical Research Ethics Committee, University Hospital of Bellvitge.
ProcedureECT was administered following current clinical guidelines,1,5 with electrocardiogram, heart rate, blood pressure and oxygen saturation (SpO2) recorded throughout the procedure. All patients were preoxygenated with high O flows (10L/min) by face mask connected to a manual resuscitation system. Subsequently, anaesthesia was given with sodium thiopental (1.5–2.5μg/kg) and succinylcholine (0.5μg/kg), and manual hyperventilation with wide pulses and variable duration (1–3μg/kg)min). In usual practice, the duration-both preoxygenation and hyperventilation per se-was determined by the anaesthesiologist (hyperventilation following usual clinical practice). The electrical stimulation was then given using the Thymatron® System IV device, with brief pulse (0.5–1ms), placement of bifrontotemporal electrodes and charge between 1.5 and 2.5 times the patient's convulsive threshold. After the crisis, the patient was assisted until recovery of spontaneous ventilation.
Application of the rHV manoeuvres was as follows:
- -
After preoxygenation and before anaesthetic induction (at start or t1), the patient's initial EtCO2 was recorded, placing the facial mask over the nose and mouth, ensuring a good seal and encouraging the patient to breathe voluntarily for 1min. Respiration quality was controlled using the capnogram, adjusting the volume of each respiration to the current volume adjusted for the patient's weight (6–8mL/kg). The EtCO2 values were taken as valid in that no discrepancy of more than 4 points was observed between the repeated measurements of EtCO2 and with at least 3 consecutive monomorphic waves in the capnogram.
- -
After anaesthetic induction, hyperventilation was given using a facemask connected to a manual resuscitation system with O2 flow of 10L/min and a CO2 sampling line from a Datex-Engstrom AS/3™ monitor. Systematised and constant hyperventilation was given for 60s at the expense of an increase in respiratory rate to 40–50pulses/min with small volumes, and EtCO2 (post-rHV or t2) was measured once again.
Demographic, clinical and treatment variables were recorded (age, sex, diagnosis following DSM-IV-TR,21 pharmacological treatment and parameters for the application of ECT).
For the evaluation of the main objective, at each treatment session run with rHV, the following variables of interest were recorded at 2 different points of the procedure (initial or t1 and post-rHV or t2): haemodynamic variables (systolic, diastolic and mean arterial pressure, heart rate) and ventilatory (SpO2 and EtCO2). EtCO2 values were monitored by capnography with a CO2 line connected to the facemask and Datex-Engstrom AS/3™ monitor.
In all sessions, the following variables were recorded to assess the quality of seizures: duration of motor seizure, duration of electroencephalographic seizure (EEG) and quality indices, determined automatically by the Thymatron® System IV device. Interhemispheric coherence measures were recorded (maximum sustained coherence, time to maximum sustained coherence); amplitude measurements (mean energy rate of seizure, maximum sustained power, time to maximum sustained power, amplitude of initial, mid and postictal segment); and the rate of postictal suppression.
Statistical analysisStudent's T-test was used for paired data or Wilcoxon's sum of ranks, when required, due to the lack of normal variables, to evaluate changes in ventilatory parameters prior to and after the application of rHV (main objective), and to explore changes in the quality of seizures by comparing the sessions run with hyperventilation, following the usual practice for those run with rHV. The relationships between the different ventilatory variables of interest and the crisis obtained through correlations (Spearman's Rho) were studied.
The level of statistical significance was set at p<0.05 (bilateral). Bonferroni correction was used for multiple comparisons in the main objective analysis.
The analyses were run with SPSS® v. 18.0 for Windows (SPSS, Chicago, USA). GPower 3.1.9.2 (Franz Faul, Kiel Univ., Germany) was used to calculate the power of the sample in the main objective analysis, run with the Student's T-test for paired data, assessing 65 sessions of ECT which gave statistical power of 99% to detect the mean difference (6.52) and the standard deviations observed in the study.
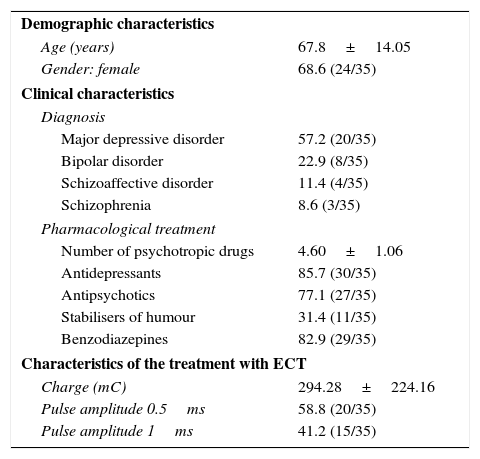
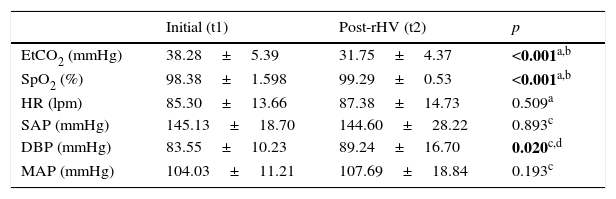
ResultsThe clinical, demographic and treatment characteristics of the sample are shown in Table 1 and after (t2) rHV manoeuvres in the 65 ECT sessions analysed for the main objective. There was a decrease in CO2 and a statistically significant increase in SpO2 and DBP after rHV. The mean decrease in CO2 reached was 6.52±4.75±mmHg (95% CI −7.7 to −5.3) (Table 2).
Clinical and demographic characteristics of the sample (No.=35).
| Demographic characteristics | |
| Age (years) | 67.8±14.05 |
| Gender: female | 68.6 (24/35) |
| Clinical characteristics | |
| Diagnosis | |
| Major depressive disorder | 57.2 (20/35) |
| Bipolar disorder | 22.9 (8/35) |
| Schizoaffective disorder | 11.4 (4/35) |
| Schizophrenia | 8.6 (3/35) |
| Pharmacological treatment | |
| Number of psychotropic drugs | 4.60±1.06 |
| Antidepressants | 85.7 (30/35) |
| Antipsychotics | 77.1 (27/35) |
| Stabilisers of humour | 31.4 (11/35) |
| Benzodiazepines | 82.9 (29/35) |
| Characteristics of the treatment with ECT | |
| Charge (mC) | 294.28±224.16 |
| Pulse amplitude 0.5ms | 58.8 (20/35) |
| Pulse amplitude 1ms | 41.2 (15/35) |
SD: standard deviation; ECT: electroconvulsive therapy.
Data is shown as mean±SD except for categorical variables, which are expressed as a percentage (n/No.).
Comparison of ventilatory and haemodynamic parameters at pre- and post-application points of reflex hyperventilation (n=65).
| Initial (t1) | Post-rHV (t2) | p | |
|---|---|---|---|
| EtCO2 (mmHg) | 38.28±5.39 | 31.75±4.37 | <0.001a,b |
| SpO2 (%) | 98.38±1.598 | 99.29±0.53 | <0.001a,b |
| HR (lpm) | 85.30±13.66 | 87.38±14.73 | 0.509a |
| SAP (mmHg) | 145.13±18.70 | 144.60±28.22 | 0.893c |
| DBP (mmHg) | 83.55±10.23 | 89.24±16.70 | 0.020c,d |
| MAP (mmHg) | 104.03±11.21 | 107.69±18.84 | 0.193c |
EtCO2: final expiratory carbon dioxide; HR: heart rate; rHV: reflex hyperventilation; DBP: diastolic blood pressure; MAP: mean arterial pressure; SBP: systolic blood pressure; SpO2: oxygen saturation; t1: stage 1 (pre-HVr); t2: stage 2 (post-rHV).
Data are shown with mean±standard deviation.
In bold type, statistically significant data.
The lower values of EtCO2 after rHV correlated with a longer duration of motor seizures(r=−0.282; p=0.024) and EEG (r=−0.276; p=0.032).
It was noted that maintaining high SpO2 values correlated with higher postictal suppression rate values (−r=0.357; p=0.019), the average energy rate of seizure (−r=0.342; p=0.012) and a greater amplitude of the mean ictal segment (r=−0.364; p=0.007).
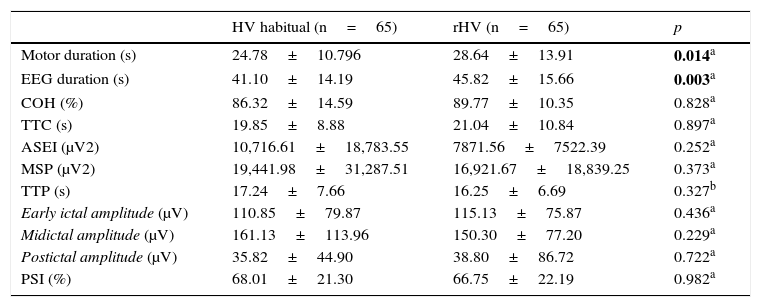
Table 3 shows the characteristics of the EEG recording of the rHV sessions, as compared to the records for the sessions with the same patients run following the usual clinical practice. A mean motor seizure length of 3.86±14.62s and EEG of 4.73±13.95s was found in the sessions run with rHV manoeuvres, without finding any statistically significant differences in the other ictal quality parameters. Also, lower values of EtCO2 reached after rHV correlated with greater differences in motor seizure time (r=−0.368; p=0.003) and EEG (r=−0.342; p=0.006) as compared with the sessions with hyperventilation following the usual practice.
Comparison of seizure parameters between sessions, following the usual procedure, and sessions with the same patients, with reflex hyperventilation manoeuvres.
| HV habitual (n=65) | rHV (n=65) | p | |
|---|---|---|---|
| Motor duration (s) | 24.78±10.796 | 28.64±13.91 | 0.014a |
| EEG duration (s) | 41.10±14.19 | 45.82±15.66 | 0.003a |
| COH (%) | 86.32±14.59 | 89.77±10.35 | 0.828a |
| TTC (s) | 19.85±8.88 | 21.04±10.84 | 0.897a |
| ASEI (μV2) | 10,716.61±18,783.55 | 7871.56±7522.39 | 0.252a |
| MSP (μV2) | 19,441.98±31,287.51 | 16,921.67±18,839.25 | 0.373a |
| TTP (s) | 17.24±7.66 | 16.25±6.69 | 0.327b |
| Early ictal amplitude (μV) | 110.85±79.87 | 115.13±75.87 | 0.436a |
| Midictal amplitude (μV) | 161.13±113.96 | 150.30±77.20 | 0.229a |
| Postictal amplitude (μV) | 35.82±44.90 | 38.80±86.72 | 0.722a |
| PSI (%) | 68.01±21.30 | 66.75±22.19 | 0.982a |
ASEI: average seizure energy index; COH: maximum sustained coherence; EEG: electroencephalogram; early ictal amplitude; HV: hyperventilation; midictal amplitude; MSP: maximum sustained power; postictal segment amplitude; PSI: postictal suppression index; TTC: time to reach maximum coherence; TTP: time to reach maximum power.
Data is shown with mean±standard deviation.
In bold type: statistically significant data.
The RHV manoeuvres with facial masks run in the present study were effective in the reduction of EtCO2 prior to the application of ECT, thus verifying the hypothesis that concurs with the main objective. The rHV decreased the EtCO2 by a mean of 6.52mmHg as compared with the baseline values and the SpO2 increased significantly. These changes in ventilatory parameters lengthened the duration of the seizure without changing the rest of the EEG tracing quality indices.
The significant repercussion of rHV manoeuvres, decreasing CO2, was accompanied by an increase in DBP that could be explained by the effect of hypocapnia on vascular resistance. However, this increase in DBP did not lead to any other haemodynamic changes and was resolved in all sessions in less than 5min.
The hypocapnia produced by rHV was significantly associated with a longer duration of the seizure, without any correlation with the rest of the seizure quality measures. However, O2 saturation correlated with some parameters related to the quality of the seizure without this being associated with the duration of the seizure. In a recent study, the quality of the seizure was significantly associated with the O2/CO2 ratio, measured transcutaneously, without this association being detected when O2 and CO2 levels were taken as independent variables.
This would indicate that O2 and CO2 could have a synergistic influence on the quality of the seizure. In this study, ventilatory assistance with a face mask was given following standard practice. This is not explained in detail. Mean CO2 values were 41mmHg. The quality of the seizure was evaluated by an index that included different ictal parameters.9
In this study, the duration of the motor and EEG crisis in the sessions with rHV were longer than those achieved in the same patient in the sessions following the usual practice. These results concur with those of previous studies on the impact of hypocapnia and hyperoxia produced by hyperventilation in the seizure, in the form of longer duration.8,10–13 In contrast, no significant differences were found in the comparison of the other EEG characteristics of ictal quality. The latter could be because the EtCO2 values achieved were not low enough to influence other characteristics of the seizure. In previous studies, which showed higher values for mean energy of the seizure and sustained maximum power when hyperventilation was used, the EtCO2 value decreased to at least equal to or lower than 30mmHg, using a laryngeal mask.8
However, in another study where EtCO2 was decreased to a modal value of 32mmHg, which is similar to the value achieved in the present study (31.75±4.37mmHg), no differences were observed in the rates of seizure intensity and postictal suppression, evaluated manually, as compared with the group with no hyperventilation. Even so, hyperventilation was associated with clinical changes, prolonging the duration of the seizure and decreasing the reorientation time in the ECT sessions. In this study, the hyperventilation method consisted of the active application of 20 insufflations at maximum capacity and frequency of one respiration per second before the electrical stimulus, compared to a maximum of 3 positive pressure ventilations in the group with no hyperventilation.13
A possible way to increase hypocapnia with the use of a face mask would be to prolong hyperventilation time to 2–3min before the application of the electrical stimulus.9,10,22–24 In the present study, hyperventilation, following anaesthetic induction, was applied for 1min, as this made it possible not to extend the procedure excessively. A greater increase in the time between anaesthetic induction and the application of the stimulus may affect the anaesthetic depth25 and even require an increase in the dose of the anaesthetic, with an eventual repercussion on the convulsive threshold.26 In previous studies on voluntary hyperventilation, run in epilepsy consultations during EEGs to provoke a crisis, in 85.5% of the patients these occurred in the first 90s of hyperventilation.27
In this study, rHV occurred at the expense of increasing the respiratory rate with small volumes to minimise stomach insufflation and possible associated adverse effects, such as nausea, regurgitation and subsequent bronchoaspirations.
Among the limitations of the study, it should be noted that the design was observational and not randomised. The absence of determination of the EtCO2 values in the sessions with hyperventilation, following the usual clinical practice, prevented objectivity as to the degree of hyperventilation achieved and its repercussion on the EEG recordings. Therefore, the variability of hyperventilation in these sessions, run following the usual procedure, at the discretion of the anaesthesiologist, could be minimising or maximising the differences found in the rHV sessions. Determination of EtCO2 values is not general clinical practice in our working environment.
All rHV was run with a face mask without using any other airway management methods such as the laryngeal mask or orotracheal intubation, which could require the use of higher doses of anaesthetic drugs.22 The use of face masks presents difficulties in coapting the mask correctly in some patients, due to anatomical aspects of the face physiognomy, such as the presence of a bushy beard, absence of teeth due to removing dentures, loss of muscle mass secondary to large losses of weight, etc. The impact of this is generally minimised by adequate training in the application of the technique and in particular for the present study, with the exclusion of sessions that did not present stable baseline EtCO2 values. The manual ventilatory assistance with face mask is the most commonly used in the usual procedure at most centres. Orotracheal intubation or the laryngeal mask are not routinely used or univocally recommended for the time being in the clinical practice guidelines for ECT.
EtCO2, as a measure for monitoring ventilation may be susceptible to artefacts if the face mask is used for airway management. EtCO2 was monitored by capnography, since it is a bloodless method that has been used in monitoring CO2 in previous studies in the field of ECT,23,28,29 instead of using other more accurate methods for measuring CO2 but more invasive and without immediate reading possible, such as arterial blood gas.
Finally, we should underline the limitations to the use of seizure quality rates calculated automatically by the device itself (Thymatron® System IV) from the EEG records. Situations that generate artefacts in the recording (patient movements, accidental disconnection of any of the cables, or transmission of the electrocardiogram signal) may give rise to erroneous values or prevent calculation of these quality indexes. This fact raises the need to reach a consensus over the evaluation of clinical quality indicators of EEG registers, beyond those generated by the devices themselves.
In future studies it would be valuable to assess the effects of hyperventilation on the treatment response and adverse effects of ECT, as well as the safety and tolerability of the use of hyperventilation. In some previous studies, the effect of hyperventilation on the duration of the seizure was only significant in the first session of ECT,23 so that more in-depth study of the extent of the effects produced by hyperventilation throughout the course of treatment is required, taking into account the electric charge.
In conclusion, the rHV manoeuvres proposed in this study influence the ventilatory parameters, with relevant clinical repercussions, by lengthening the duration of the seizures obtained without worsening the quality of the EEG tracing. Furthermore, the study considers the importance, in usual clinical practice, of using manual hyperventilation protocols with systematised face masks which are easy to apply and without any added replicable and generalisable costs. The regular use of CO2 monitoring methods within these protocols, in addition to increasing patient safety in case of adverse respiratory events, enables us to objectify the changes obtained with hyperventilation manoeuvres and helps to optimise ventilation during ECT sessions. Further studies are needed to examine the characteristics of optimal application for hyperventilation more closely and to study its clinical effects. This could improve the efficacy and efficiency of ECT.
Declaration of transparencyThe main author states that this manuscript is an honest, accurate and transparent account of the study presented; that no major aspect of the study has been omitted; and that the differences with the study initially planned have been explained (and if relevant, recorded).
Ethical responsibilityProtection of people and animalsThe authors state that there have been no experiments done on humans or animals for this research.
Confidentiality of dataThe authors declare that theyt have followed the protocols for their work centre on publication of patient information.
Right to privacy and informed consentThe authors have no conflicts of interest to declare.
Conflict of interestThe authors state that there is no conflict of interest.
Please cite this article as: de Arriba-Arnau A, Dalmau A, Salvat-Pujol N, Soria V, Bocos J, Menchón JM, et al. Inducción de hipocapnia e hiperoxia con maniobras de hiperventilación reglada en la terapia electroconvulsiva. Rev Psiquiatr Salud Ment (Barc). 2017;10:21–27.