The aim of the current study was to assess the prevalence of symptoms of attention deficit/hyperactivity disorder (ADHD) in adolescents and young adults diagnosed with other primary psychiatric disorders, who had not responded to previous treatments.
Materials and methodsA total of 795 outpatients aged 15–24 years were included. The presence of ADHD was studied using DSM-IV criteria and the frequency of symptoms using the 18-item DuPaul ADHD Rating Scale.
ResultsADHD (DSM-IV criteria) was present in 48 patients (6%), none of them had previously received the diagnosis. A total of 260 patients (32.7%) met the criteria for moderate ADHD and between them, severity of primary psychiatric disorder was higher according to the CGI-S (p=0.007). Risk factors for moderate ADHD symptoms were the presence of substance use disorders (SUD) (odds ratio=1.543, p=0.01) and borderline personality disorders (odds ratio=2.173, p=0.0001).
ConclusionUnrecognized ADHD was present in 6% of patients; moreover 32.7% of the sample also presented moderate symptoms of the disorder. Screening for ADHD in young patients with refractory response to primary disorder treatment, mainly those with substance use disorders, conduct and personality disorders is highly advisable, due to the high frequency of ADHD comorbidity in these psychiatric disorders.
El objetivo de este estudio fue evaluar la prevalencia de síntomas de trastorno por déficit de atención con hiperactividad (TDAH) en adolescentes y adultos jóvenes diagnosticados de otros trastornos psiquiátricos primarios que no habían respondido a tratamientos previos.
Material y métodosSe incluyeron 795 pacientes ambulatorios de 15-24 años. Se estudió la presencia de un TDAH según los criterios DSM-IV y la frecuencia de los síntomas utilizando la escala de valoración del TDAH de DuPaul de 18 ítems.
ResultadosSe objetivó la presencia de un TDAH (criterios DSM-IV) en 48 pacientes (6%), ninguno de los cuales previamente había recibido este diagnóstico. Un total de 260 pacientes (32,7%) presentaron síntomas moderados de TDAH y en ellos la gravedad del trastorno psiquiátrico de base era mayor según la ICG-S (p=0,007). Los factores de riesgo para tener síntomas moderados de TDAH fueron la presencia de trastornos por uso de sustancias (TUS) (odds ratio=1,543; p=0,01) y de trastorno límite de la personalidad (odds ratio =2,173; p=0,0001).
ConclusionesEl TDAH no diagnosticado previamente estaba presente en el 6% de los pacientes, observándose asimismo una elevada frecuencia de síntomas moderados del trastorno (32,7%) en la muestra. Por estos motivos sería recomendable hacer un minucioso estudio del TDAH en los jóvenes refractarios al tratamiento del trastorno primario, principalmente en aquellos con trastornos por uso de sustancias, trastornos de conducta y de personalidad, debido a la elevada comorbilidad entre el TDAH y estos trastornos.
Attention deficit hyperactivity disorder (ADHD) occurs in approximately 5.3% of children and adolescents,1 and 50–70% of patients still have significant symptoms of the disorder during adolescence and early adulthood.2 The World Health Organization defines adolescence as the period of life ranging from 10 to 19 years, and youth as the period from 15 to 24 years.3 Difficulties experienced by adolescents as a result of ADHD may be intensified due to increasing demands and expectations occurring in this stage of life.4
Comorbidity with other psychiatric disorders such as substance use disorders, anxiety disorders, mood disorders, oppositional defiant disorder, borderline personality disorder or conduct disorder may be present in up to 70% of children and adolescents with ADHD.5–7 For example, comorbidity of substance use disorders and ADHD in addiction treatment centers ranges from 30 to 50%.8 Indeed, substance use disorders may be present later in life for up to 35% of adolescents with ADHD.9 The presence of comorbid psychiatric disorders is associated with significant additional morbidity which complicates ADHD diagnosis, treatment and prognosis9; therefore, it is important to identify and treat them.
Moreover, high frequency of ADHD has been observed in adolescents diagnosed with psychiatric disorders, although often it goes undetected or untreated10; furthermore, 6.5–25.4% of adults with a psychiatric diagnosis also meet criteria for ADHD.11 The 4 most prevalent psychiatric diagnoses associated with high ADHD rates are substance use disorders, bipolar disorder, agoraphobia and dysthymia. Thus, in the National Institute of Mental Health's STEP–BD systematic treatment program, a sample of 1000 adults with bipolar disorder had 9.5% lifetime prevalence of comorbid ADHD.12 In a sample of 161 adult psychiatric outpatient non-psychotic patients, ADHD prevalence was 16.8%.13 Patients with substance use disorders are also significantly more likely to have ADHD (25.4% compared to 4% in those without any other psychiatric disorder).14
Although overall ADHD prevalence is 2–7 times higher in adults with psychiatric illness,15 information on ADHD prevalence in adolescents and young adults diagnosed with other psychiatric illnesses is very low.16–19 Therefore, this study aims to determine ADHD prevalence symptoms in adolescents and young adults diagnosed with other primary psychiatric disorders, who do not respond sufficiently to treatment for these disorders. This is the first study to assess the presence of ADHD symptoms in a sample of young people with other psychiatric disorders who have responded poorly to treatment.
Materials and methodsStudy designA cross-sectional study was designed with the main objective of determining ADHD symptom prevalence and severity in adolescents/young adults (15–24) with other psychiatric diagnosis and inadequate response to their disorder's treatment. The study's secondary objectives were to: (a) assess ADHD symptom prevalence and severity in various groups of young people depending on their primary psychiatric diagnosis and (b) assess whether there were differences in drug abuse among patients with or without ADHD symptoms.
This study was conducted in mental health centers and public psychiatric units throughout Spain. In total, 180 centers participated: 64 adult mental health centers (35.55%), 59 children and youth mental health centers (32.77%), 22 substance-use care and monitoring centers (12.22%), 12 eating behavior disorder units (6.66%), and 23 adolescent addiction units (12.77%).
Physicians participating in each center (No.=180) were asked to work during a 2-month period on enrolling the first 5 consecutive outpatient-care patients with non-psychotic disorders, so that the centers would have a homogeneous recruitment rate distribution. All patients meeting selection criteria during the study period were assessed (No.=835), except those patients with psychotic disorders. The study was approved by the Vall d’Hebron University Hospital Ethics Committee in Barcelona. After explaining what constituted the study, written informed consents were obtained from all participants, and if under 18 years of age, from their parents or guardians.
ParticipantsBetween April 30 and June 30, 2012, the study included adolescents and young adults of both sexes, aged between 15 and 24 years, diagnosed with one or more non-psychotic disorders including affective disorders, substance use disorders, anxiety disorders, borderline personality disorder, bulimia nervosa, behavioral disorders (oppositional defiant disorder, conduct disorder), and antisocial personality disorder, who attended follow-up checks in outpatient clinics, provided they would have received standard treatment (as defined by the NICE guide) for psychiatric disorder for at least 2 months before the study. Another inclusion criterion was insufficient response to previous pharmacological/psychotherapeutic treatments which required a score equal to or greater than 4 (moderately ill) on the clinical global impression scale of severity (CGI-S) at the time of entering the study.
Patients were excluded if their IQ was lower than 85, as were those with psychotic disorders (excluding substance-induced psychosis), neurodevelopmental disorders, severe neurological disease (other than Tourette's), psychiatric disorder exacerbation, acute intoxication or psychotropic drug withdrawal syndrome, in addition to those who had a previous ADHD diagnosis and/or had received previous pharmacological treatment for it (current or past treatment with methylphenidate or atomoxetine), and patients with a CGI-S≤3.
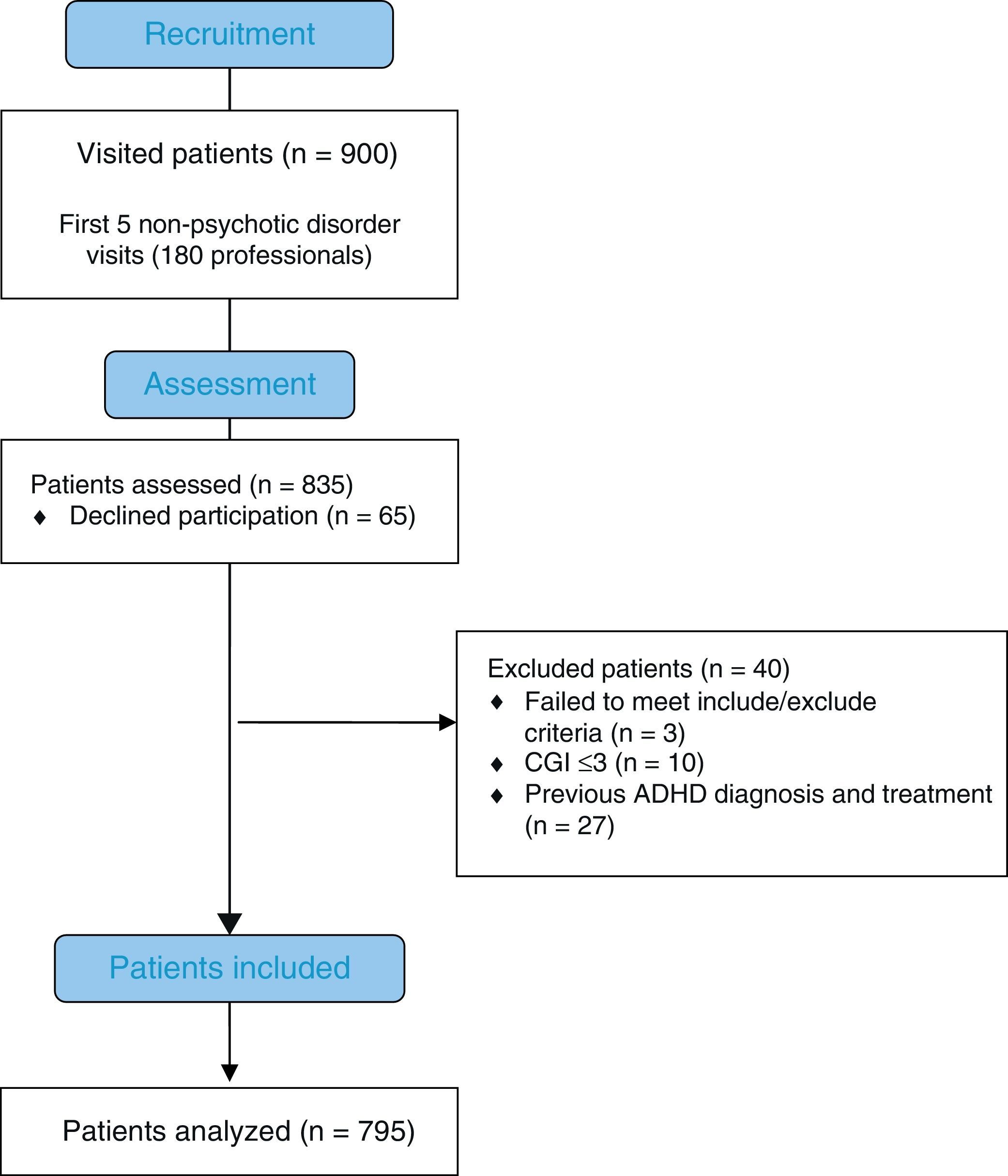
Fig. 1 shows the flow chart of the process for recruitment and selection of patients who participated in the study. From a total of 900 patients, 835 agreed to participate. However, 3 were excluded due to lack of inclusion/exclusion criteria (missing), and 27 patients with previous ADHD diagnosis and previous pharmacological treatment for said disorder (all patients who had a previous ADHD diagnosis had received pharmacological treatment), and 10 patients with CGI-S≤3 (adequate response to treatment).
Data collectionData were collected during a single visit at the time when physician and patient met via a standardized questionnaire specially designed for the study. Completed questionnaires were entered into a centralized database. The following variables were collected: age, sex, weight, educational level (no education, elementary school, high-school, college/university), employment status (unemployed, active, student), socioeconomic level, primary psychiatric diagnosis, and other associated psychiatric diagnoses defined by DSM-IV and data related to substance abuse (substance type, age at first use, amount consumed, administration route).
Presence of ADHD was accepted when DSM-IV diagnostic criteria for the disorder was met, based on the clinical interview. Other collected data: ADHD subtype (predominantly hyperactive-impulsive, predominantly inattentive or combined), CGI-ADHD-S score, frequency and intensity of ADHD symptoms using the DuPaul 18-item ADHD rating scale.20 This is a reliable and easy-to-administer instrument both for diagnosing ADHD in adolescents and adults, as well as for assessing response to treatment. Its 18 items are directly related to ADHD diagnostic criteria in the DSM-IV and the study used a validated Spanish version.21,22 Moderate ADHD symptoms were defined as the presence of 6 or more diagnostic criteria for hyperactivity and/or inattention of the DSM-IV and an overall score on the rating scale of ADHD DuPaul>24. In the Spanish version validation study, a score of 24 had 81.9% sensitivity and 74.7% specificity.22
Statistical analysisCategorical data were expressed as numbers and percentages, and continuous data as average and interquartile range (25th–75th percentile). Continuous variables were analyzed with the Student t test and Kruskal–Wallis test, and categorical variables with the chi-square test or Fisher's exact test when necessary. For statistical analysis, SAS software version 9.1.3 (Statistical Analysis Systems, SAS Institute, Cary, NC, USA) was used. Statistical significance was defined as p<0.05.
ResultsSociodemographic characteristics of study subjects were as follows: 57.5% in the sample were male, 42.5% female; mean age 21.1 years, and 2.6-year standard deviation (23.3% of patients aged 15–18 years, 51.3% between 18 and 21 years, and 25.4% between 21 and 24 years). At the time of the study, 34.4% of patients went to elementary school, 48% high-school; 33% were unemployed, 31% were attending school, and 31% actively working. Most study participants were from an average socioeconomic level (62.3%), 31.7% were patients from a low socioeconomic level, and 6% from a high socioeconomic level.
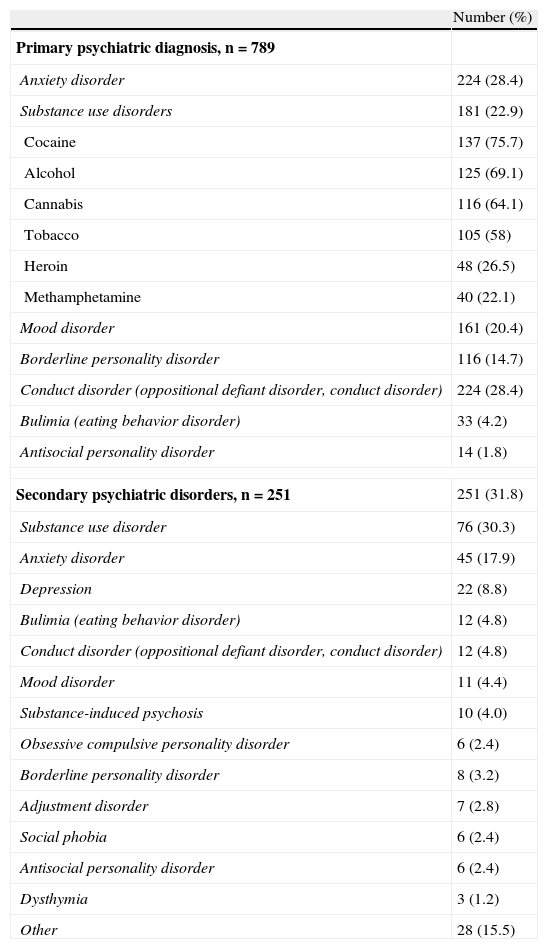
The most common primary diagnoses were anxiety disorders (18.7%), substance use disorders (cocaine, alcohol, tobacco, cannabis, methamphetamine, heroin) (25%), and mood disorders (10.4%) (Table 1). Among patients with substance use disorders, cocaine abuse/dependence was most common (75.7% of cases), followed by alcohol (69.1%), cannabis (64.1%), tobacco (58%), heroin (26.5%), and methamphetamine (22.1%).
Psychiatric diagnoses in the study population.
| Number (%) | |
| Primary psychiatric diagnosis, n=789 | |
| Anxiety disorder | 224 (28.4) |
| Substance use disorders | 181 (22.9) |
| Cocaine | 137 (75.7) |
| Alcohol | 125 (69.1) |
| Cannabis | 116 (64.1) |
| Tobacco | 105 (58) |
| Heroin | 48 (26.5) |
| Methamphetamine | 40 (22.1) |
| Mood disorder | 161 (20.4) |
| Borderline personality disorder | 116 (14.7) |
| Conduct disorder (oppositional defiant disorder, conduct disorder) | 224 (28.4) |
| Bulimia (eating behavior disorder) | 33 (4.2) |
| Antisocial personality disorder | 14 (1.8) |
| Secondary psychiatric disorders, n=251 | 251 (31.8) |
| Substance use disorder | 76 (30.3) |
| Anxiety disorder | 45 (17.9) |
| Depression | 22 (8.8) |
| Bulimia (eating behavior disorder) | 12 (4.8) |
| Conduct disorder (oppositional defiant disorder, conduct disorder) | 12 (4.8) |
| Mood disorder | 11 (4.4) |
| Substance-induced psychosis | 10 (4.0) |
| Obsessive compulsive personality disorder | 6 (2.4) |
| Borderline personality disorder | 8 (3.2) |
| Adjustment disorder | 7 (2.8) |
| Social phobia | 6 (2.4) |
| Antisocial personality disorder | 6 (2.4) |
| Dysthymia | 3 (1.2) |
| Other | 28 (15.5) |
Additionally, 31.6% of patients had more than one psychiatric diagnosis. Mean of the psychiatric diagnoses per patient was 1.3 (0.6), and mean time from primary diagnosis was 25.7 (32.3) months. Average score on the CGI–S was 4 (4–5 interquartile range). Sixty-nine patients had ADHD family history, and 58 had siblings with ADHD, at an average of 2 brothers (1–3 range). Of the 835 patients assessed, those maintaining CGI-S≥4 (No.=795) were considered as having an inadequate response to previous treatment; these patients had a 6-month mean (mean=6, standard deviation=3) of pharmacological/psychotherapeutic pretreatment.
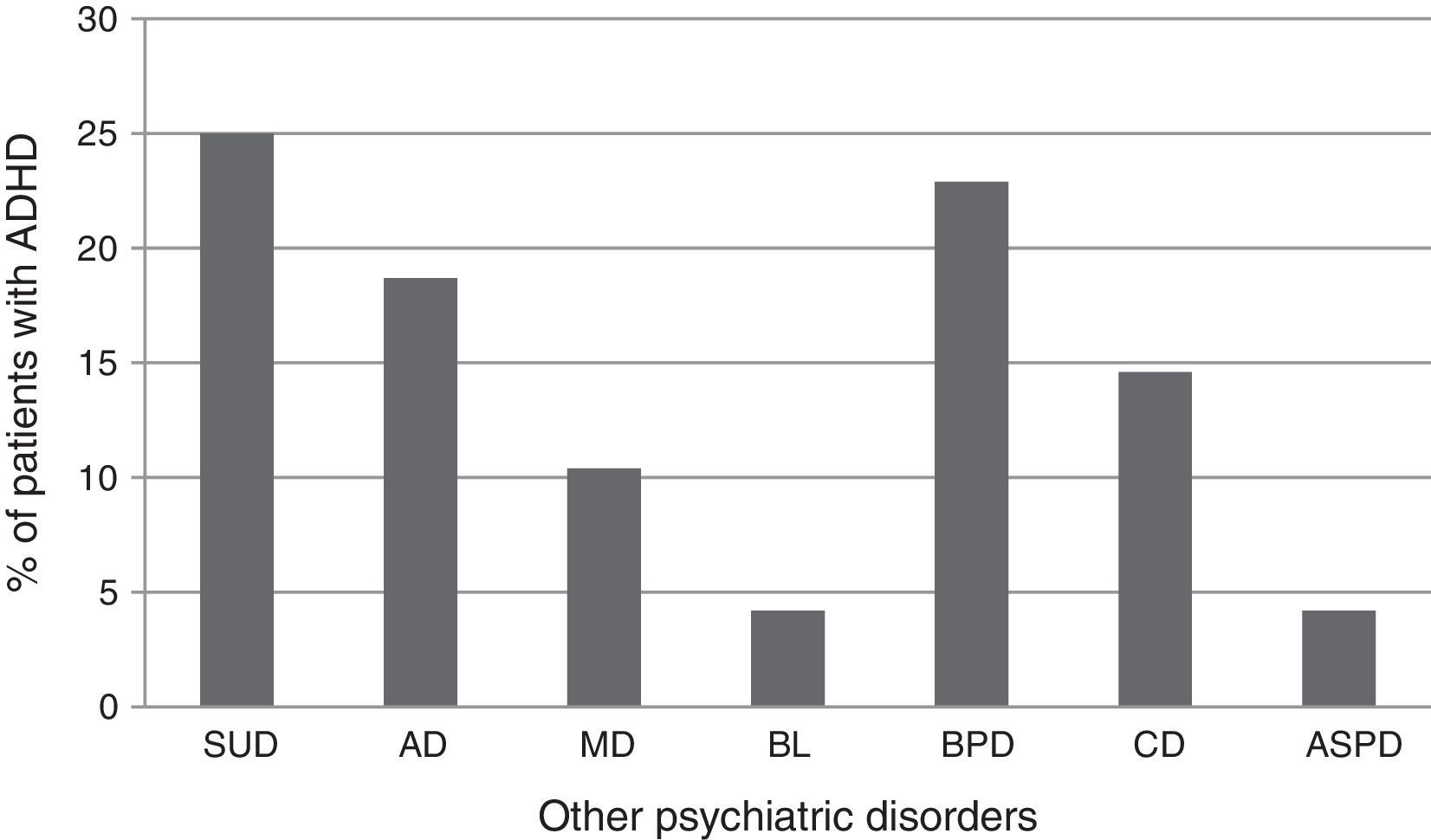
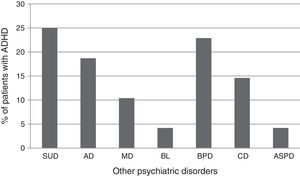
Of the 795 patients included in the study, 48 met DSM-IV clinician-assessed criteria for ADHD diagnosis, (6% overall prevalence rate): adult mental health centers (No.=11; 22.91%), children and youth mental health centers (No.=16; 33.33%), and substance-use care and monitoring centers (No.=10; 20.83%), eating disorder behavior units (No.=2; 4.16%), adolescent addiction units (No.=9; 18.75%). ADHD subtypes were: combined for 23 patients, predominantly inattentive for 15, predominantly hyperactive/impulsive for 10. Fig. 2 shows ADHD patient distribution in the various primary psychiatric disorder categories.
Percentage of patients meeting ADHD DSM-IV criteria on various primary psychiatric diagnoses. BL: bulimia; AD: anxiety disorders; ASPD: antisocial personality disorder; CD: conduct disorder; ADHD: attention deficit hyperactivity disorder; MD: mood disorders; BPD: borderline personality disorder; SUD: substance use disorder.
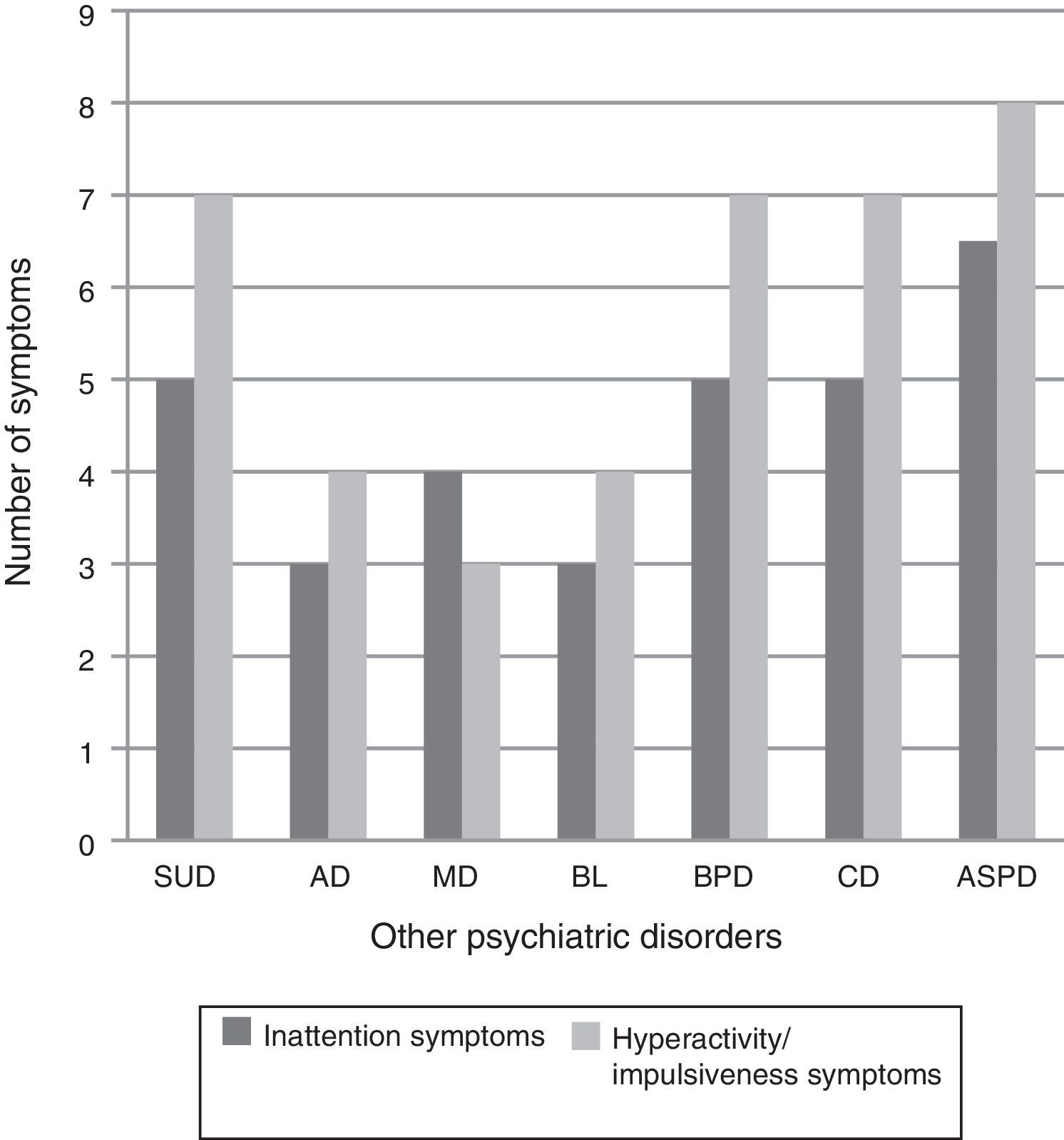
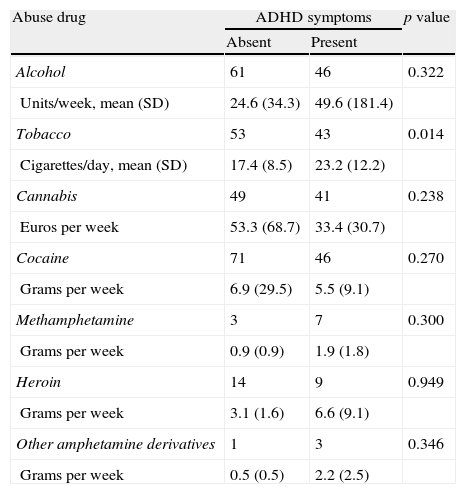
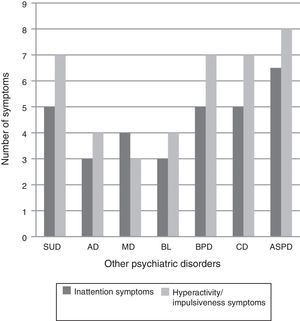
Average ADHD Rating Scale score was 23 (12–32 range). There were statistically significant differences (p<0.0001) on symptom frequency depending on primary psychiatric diagnosis. Subjects with substance abuse disorder, borderline personality disorder, conduct disorder and antisocial personality disorder had a greater number of symptoms of inattention and hyperactivity/impulsivity than subjects with anxiety disorder, mood disorder or bulimia (Fig. 3). However, in subjects with substance abuse disorders, differences were found in drug use, depending on the presence or absence of ADHD symptoms, which were not statistically significant, with the exception of tobacco use (Table 2). Subjects with ADHD symptoms smoked more cigarettes per day than those without (mean 23.1 [12.2] compared to 17.4 [8.5], p=0.014). A higher percentage of patients with psychiatric disorders and co-occurring ADHD symptoms had ADHD family history compared to those without ADHD symptoms. In all cases, the differences were statistically significant (father with ADHD: 9.3% with ADHD compared to 4.7%, p=0.014; mother with ADHD: 5.7% compared to 1.6%, p=0.001; siblings with ADHD: 13.2% compared to 5.1% (p=0.0001).
Frequency of ADHD symptoms by primary psychiatric diagnosis. BL: bulimia; AD: anxiety disorders; ASPD: antisocial personality disorder; CD: conduct disorder; ADHD: attention deficit hyperactivity disorder; MD: mood disorders; BPD: borderline personality disorder; SUD: substance use disorder.
Drug use in patients with substance use disorders according to the presence or absence of ADHD symptoms.
| Abuse drug | ADHD symptoms | p value | |
| Absent | Present | ||
| Alcohol | 61 | 46 | 0.322 |
| Units/week, mean (SD) | 24.6 (34.3) | 49.6 (181.4) | |
| Tobacco | 53 | 43 | 0.014 |
| Cigarettes/day, mean (SD) | 17.4 (8.5) | 23.2 (12.2) | |
| Cannabis | 49 | 41 | 0.238 |
| Euros per week | 53.3 (68.7) | 33.4 (30.7) | |
| Cocaine | 71 | 46 | 0.270 |
| Grams per week | 6.9 (29.5) | 5.5 (9.1) | |
| Methamphetamine | 3 | 7 | 0.300 |
| Grams per week | 0.9 (0.9) | 1.9 (1.8) | |
| Heroin | 14 | 9 | 0.949 |
| Grams per week | 3.1 (1.6) | 6.6 (9.1) | |
| Other amphetamine derivatives | 1 | 3 | 0.346 |
| Grams per week | 0.5 (0.5) | 2.2 (2.5) | |
A total of 260 patients (32.7%) met criteria for moderate ADHD symptoms. ADHD symptoms were primarily combined in 127 (47.7%) patients, predominantly attention deficit in 92 (35.4%), and predominantly hyperactive/impulsive in 44 (16.9%). Moderate ADHD symptoms were more frequent in males than females (67.1% compared to 32.9%, p=0.0002). With regard to the primary study endpoint, ADHD symptom frequency in each patient was high, with an average of 4 symptoms in the inattention subscale and 3 symptoms in the hyperactivity/impulsivity subscale. Thus, many study participants scored 2 or 3 (“often” or “very often”) for questions describing inattention and hyperactivity/impulsivity symptoms.
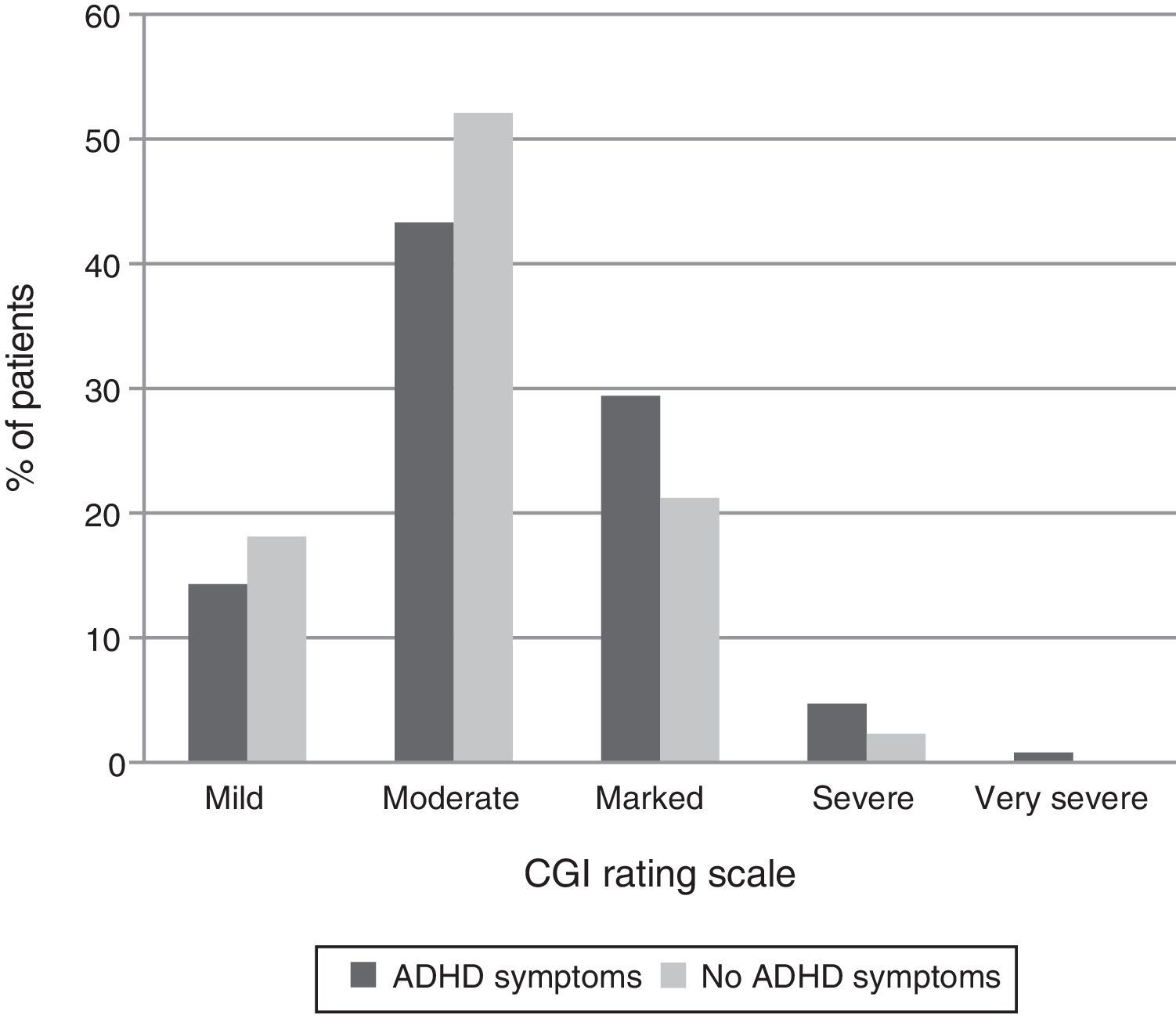
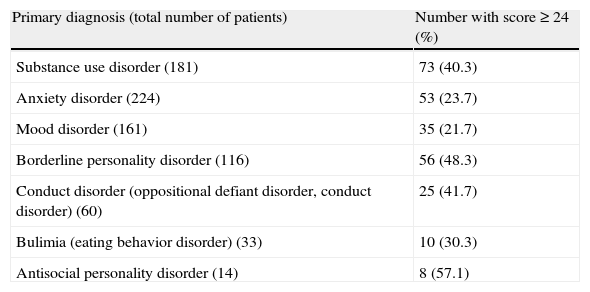
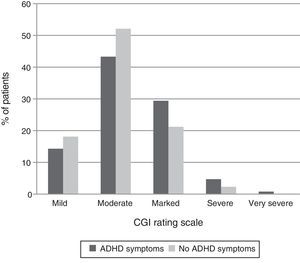
Presence of moderate ADHD symptoms was significantly linked to primary psychiatric disorder. As shown in Table 3, moderate ADHD symptoms appeared significantly more frequently in substance use disorders (40.3%), borderline personality disorder (48.3%), behavior disorders (41.7%), and antisocial personality disorder (57.1%), compared to the remaining diagnostic subgroups (p<0.0001). Additionally, patients with ADHD symptoms scored higher in the severity CGI-S scale than those without them (p=0.007) (Fig. 4). Indeed, 36.5% of patients with moderate ADHD symptoms ranked in the markedly ill and severely ill CGI-S categories compared to 25% of patients without moderate ADHD symptoms.
Distribution of patients with total score≥24 in the ADHD rating scale and 6 or more inattention or hyperactivity/impulsivity symptoms according to the primary psychiatric diagnosis.
| Primary diagnosis (total number of patients) | Number with score≥24 (%) |
| Substance use disorder (181) | 73 (40.3) |
| Anxiety disorder (224) | 53 (23.7) |
| Mood disorder (161) | 35 (21.7) |
| Borderline personality disorder (116) | 56 (48.3) |
| Conduct disorder (oppositional defiant disorder, conduct disorder) (60) | 25 (41.7) |
| Bulimia (eating behavior disorder) (33) | 10 (30.3) |
| Antisocial personality disorder (14) | 8 (57.1) |
Statistically significant ADHD symptom risk factors were: presence of substance use disorders (odds ratio [OR]=1.54; 95% confidence interval [CI] 1.09–2.17; p=0.01), and borderline personality disorder (OR=2.17; 95% CI 1.46–3.24; p=0.0001). In contrast, anxiety disorders (OR=0.54; 95% CI 0.39–0.77; p=0.0007), and mood disorders (OR=0.50; 95% CI 0.33–0.76; p=0.0009) were associated negatively with ADHD symptoms.
DiscussionResults obtained in this cross-sectional study of a large group of young people aged 15–24 years with primary psychiatric diagnosis who had previous inadequate response to pharmacological/psychological treatments (CGI≥4), and received care in routine clinical practice, show 6% of patients with ADHD symptoms.
We note that patients with a previous ADHD diagnosis and those with adequate response to treatment were excluded from the study. Twenty-seven patients had a previous ADHD diagnosis. This means that 3.23% of patients assessed had been previously diagnosed with ADHD; thus, the obtained ADHD symptom prevalence in patients diagnosed with other major disorders is conservative. Most patients (48%) had combined subtype ADHD. Substance use disorder was the most common psychiatric diagnosis (25%), followed by borderline personality (23%) and anxiety disorders (18.7%). Additionally, a significant study finding was that 32.7% of subjects diagnosed with other psychiatric disorders had a total ADHD rating scale score equal to or greater than the cutoff-point of 24.
The high frequency of ADHD symptoms in this study is an important finding, given that comorbid ADHD may affect adherence to pharmacological treatment for other psychiatric disorders and disrupt daily functioning, leading to a worse outcome due to refractory symptoms. Furthermore, psychiatric comorbidity greatly influences presentation, diagnosis and prognosis, complicates treatment and significantly increases ADHD morbidity.23
In this study, the most common subtype was ADHD combined subtype. In other studies, the combined subtype had more comorbid symptoms than inattentive or hyperactive/impulsive subtype.24 Another notable result was the high frequency of ADHD symptoms in young people with substance use disorder, conduct disorders, and personality disorders, compared to those with anxiety or mood disorders. It has been shown that children with ADHD and conduct disorders are at increased risk for antisocial personality disorder and substance abuse in adulthood.25 Moreover, adult patients with substance use disorders are more likely to have a previous or concurrent ADHD diagnosis.11 Many clinical and epidemiological studies have shown high comorbidity with substance use and other psychiatric disorders, although identifying psychiatric comorbidity in substance abusers is problematic, mainly because acute or chronic effects of substance abuse or withdrawal may be similar to other mental disorder symptoms.26 In a sample of 162 adolescent patients admitted to residential treatment programs for addictions, we found concurrent ADHD diagnosis in 31%; additionally, a third of the entire adolescent patient population reported previous abuse of psychostimulants.8 Substance use disorders may also be more severe when coupled with comorbid ADHD, and despite receiving further addiction treatment, these patients are less likely to maintain drug abstinence.27 In our study, the primary diagnoses for substance use disorder and borderline personality disorder were significant risk factors for coexistence of ADHD symptoms.
Regarding the influence of ADHD symptoms on drug use, no differences were observed among substance users with or without ADHD symptoms, except for tobacco use, since patients with coexisting ADHD symptoms smoked more. Finally, a significantly higher percentage of patients with coexisting ADHD symptoms had ADHD family history. Therefore, for young people with psychiatric disorders, it is important to investigate the presence of ADHD in first-degree relatives.
The results of this research must be interpreted taking certain constraints into account, such as the fact that various characteristics related to primary psychiatric diagnosis were not assessed, including medication regimen or treatment compliance. Note that patients were enrolled in public institutions; therefore, future studies should include private institutions to be able to observe possible differences. Moreover, although no structured interviews were used for ADHD diagnosis, the ADHD rating scale psychometric properties support the feasibility of this instrument for assessing and diagnosing that disorder.22 No teacher or parent scales were included for assessing ADHD symptoms. There are semi-structured interviews such as the K-SADS for children or CAADID for young adults (validated diagnostic tools in Spanish to assess ADHD28) that can be useful in assessing these patients.
ConclusionsUndiagnosed ADHD was present in 6% of patients, and high frequency of mild disorder symptoms (32.7%) was observed in the sample; therefore, it would be advisable, in order to optimize patient care, to perform a detailed study of ADHD in youths with substance use disorders, conduct disorders, and personality refractory to treatment, due to high comorbidity between ADHD and these disorders.
Ethical responsibilitiesProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentThe authors must have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence must be in possession of this document.
Conflict of interestThe study was funded by the Janssen-Cilag, S.A. Medical Department.
Dr. Ramos-Quiroga has conducted lectures and has been a consultant for Eli-Lilly, Janssen-Cilag, Novartis, Lundbeck, Shire and Rubió. He has received travel grants to attend Janssen-Cilag, Shire and Eli-Lilly conferences. In the past 3 years, the ADHD unit he leads has received grants for research and training from Eli-Lilly, Janssen-Cilag, Shire, Rovi and Rubió. Dr. Casas has received travel grants to participate in Eli Lilly and Company, Janssen-Cilag, Shire, and Laboratorios Rubió conferences. He has received research support from Janssen Cilag, Shire, Laboratorios Rubió, and Eli Lilly and Company. He has been a consultant and advisor to Janssen Cilag, Shire, Laboratorios Rubió, and Eli Lilly and Company.
Please cite this article as: Vidal R, Barrau V, Casas M, Caballero-Correa M, Martínez-Jiménez P, Ramos-Quiroga JA. Prevalencia de síntomas de trastorno por déficit de atención con hiperactividad en adolescentes y adultos jóvenes con otros trastornos psiquiátricos refractarios a tratamientos previos. Rev Psiquiatr Salud Ment (Barc). 2014;7:104–112.
These authors contributed equally to this work.