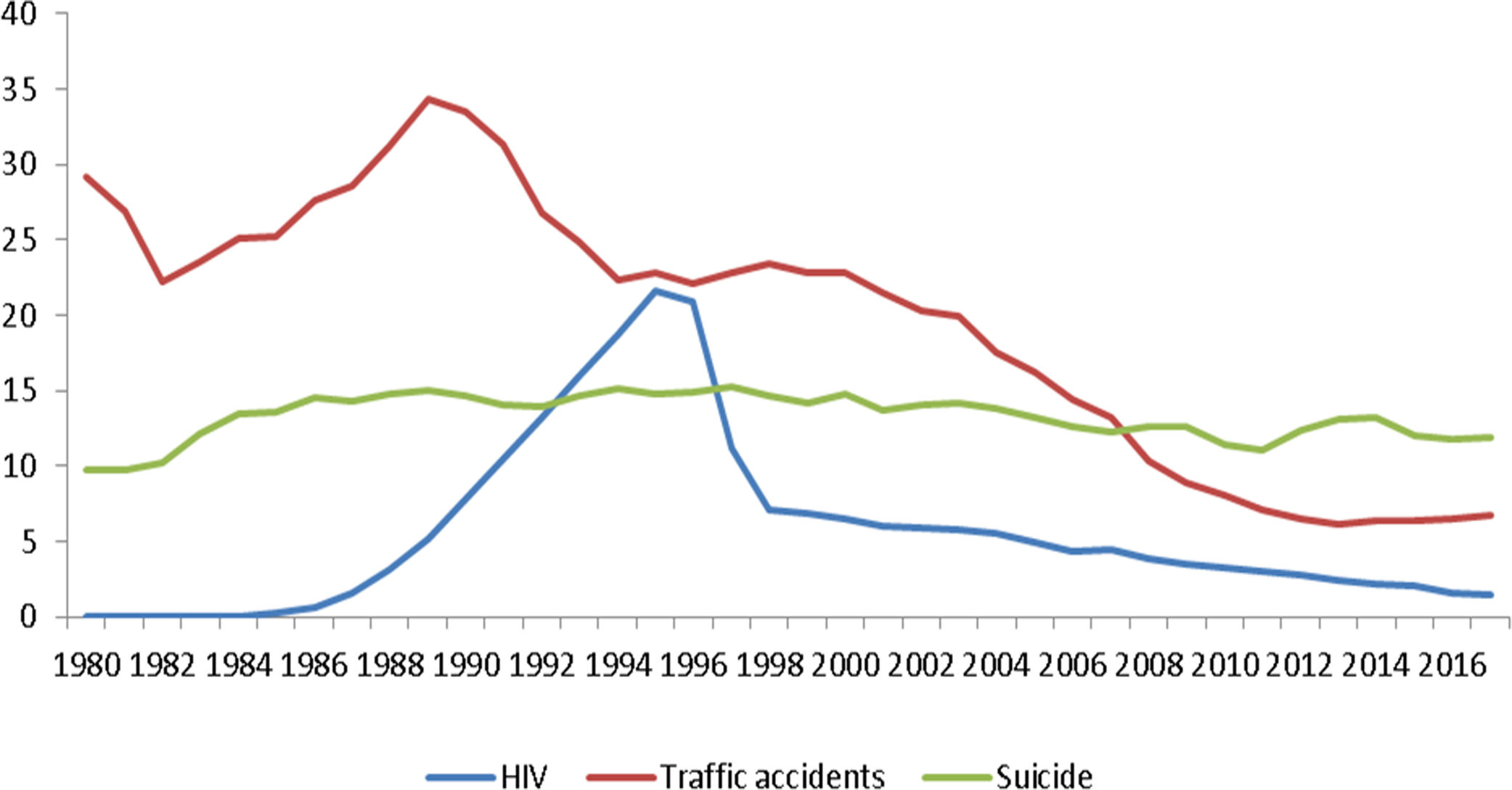
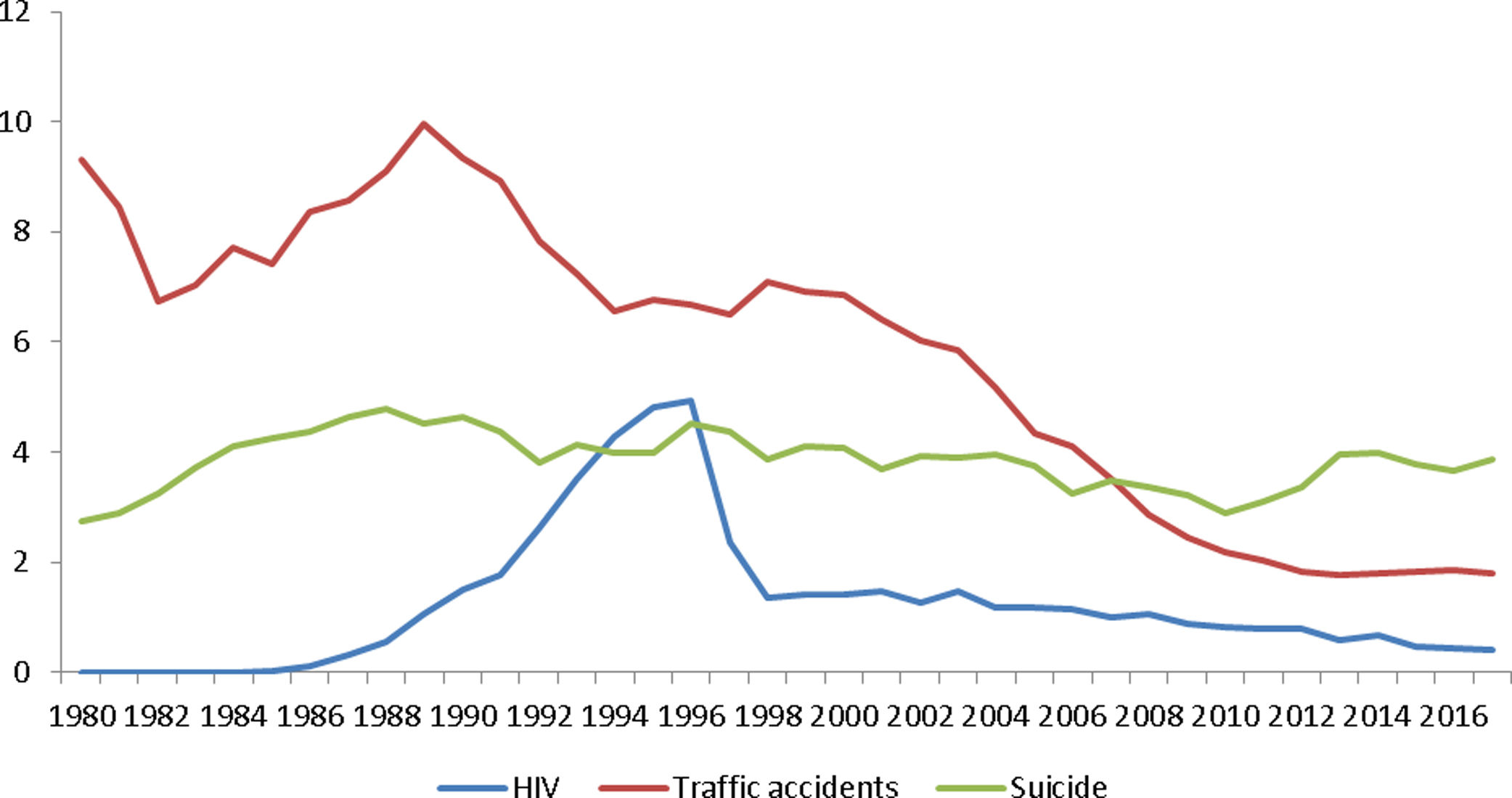
The suicide is a worldwide public health problem included among WHO's priorities. An average of 800,000 persons committed suicide every year in the world1 and 3600 in Spain; moreover, suicide is the second cause of death in those aged 15 to 29 years old.1,2 In Spain, the evolution of the main causes of death, in younger people, over the last decades; shows a clear decrease trend in traffic accidents and HIV, while death by suicide did not suffer a significant decrease for the whole period3 (Figs. 1 and 2).
The satisfactory evolution of deaths due to HIV and traffic accidents is linked mostly to a strong political commitment and appropriate policies (both causes), to the improvement of the clinical management (HIV), and to the active national and international research investment. Although these, mostly multi sectoral, public health measures do not have been successfully applied to improve national suicide rates. This fact is even more appalling if we take into consideration that suicide is also preventable and there is a huge margin for improvement. This is evident if we take into account that the disparities in suicide mortality among the Spanish regions in the year 2017 are of a much more important magnitude than the temporal variations collected over the last decades for the whole country (between 1999 and 2017 the adjusted rates of suicide ranged from 14.1 to 11.8 for males and 4.1 to 3.8 for females but the variations among the Spanish regions in 2017 had a range from 6.3 to 16.8 for males and 2.6 to 7.0 for females). Moreover, these large and recurrent disparities among the Spanish regions prevail after the improvement in the registry method implemented since 2013. Furthermore, these data are accordant with other international studies that consistently assessed that the geographical disparities in suicide mortality are of a more important magnitude than the temporal variations over the last decades.4
The scarcity of public health activities devoted to suicide control during last years added to the emerging COVID-19 pandemic, will place us in a difficult post pandemic situation, since it is reasonable to assume that the suicide rates are bound to raise.5,6 In fact, there was an increase in the suicide rates among the older people during the severe acute respiratory syndrome (SARS) epidemic in 2003 in China;7 thus similar consequences could be expected within the post-COVID-19 juncture.
One lesson we must learn from the current COVID-19 pandemic, is that we have to be prepared to face the future epidemiologic threats, including their mental health consequences.8,9 The current COVID-19 pandemic will worsen mental illness burden and increase its incidence. Quarantine policies and its consequences: stress,5 mourning, loneliness,5,8 and all the economic problems that entails,9 will produce a rise in harmful alcohol and drug use, mental illness and suicide rates as it has already been warned by WHO.5,6
In order to anticipate this scenario and mitigate it, to the best of our ability, we must start now to design and implement the appropriate measures. These should include in Spain, among others, the recommendations from experts10,11: the implementation of a consensus national plan (including the best preventive practices), with adequate resources and mandatory for all autonomous communities; the early detection of persons at risk; to approach suicide as a complex problem that requires a multi sectoral integrated approach for its prevention and treatment (including the primary care, the mental health services, social services and non-health organizations); to increase the collaboration between mental services and primary care to improve the capacity building of health professional, the diagnosis and the treatment with an adequate continuity of care; a satisfactory management and dissemination of information; to increase the research on the physiopathology and neurobiology of depression and suicide; to promote the epidemiological research of suicide and to develop new tools for an adequate information system about suicide and its risk factors, including suicide attempts.
FundingThe authors received no specific funding for this work.
Conflict of interestDr. Perez has been a consultant to or has received honoraria or grants from AstraZeneca, Bristol-Myers-Squibb, Janssen Cilag, Lundbeck, Otsuka, Servier, Medtronic and Exeltis, outside the submitted work.
Dr. Miquel Roca reported receiving grants from the European Union, the Spanish Ministry of Economy and Competitiveness and research funding or for participating in boards from Adamed, Exeltis, Janssen and Lundbeck, outside the submitted work.
Dr. Saiz-Ruiz has been a speaker for and on the advisory boards of Adamed, Lundbeck, Servier, Medtronic, Casen-Recordati, Neurofarmagen, Otsuka, Indivior, Lilly, Schwabe, Janssen and Pfizer, outside the submitted work.
The rest of the authors declare that they have no conflict of interest.