Studies on adult bipolar patients have demonstrated a disability associated with the bipolar disorder, even in euthymic patients, but there is a lack of data in the elderly population.
Material and methodA cross-sectional, multicentre study on a consecutive sample of ambulatory bipolar patients (DSM-IV-TR criteria), aged 65 years or over. Retrospective and cross-sectional sociodemographic and clinical data were collected, as well as the Clinical Global Impression for Bipolar Modified scale (CGI-BP-M) and the level of disability using the World Health Organisation Disability Assessment Schedule (WHO/DAS). The disability was assessed globally and by areas. The presence of a moderate to maximum disability compared to a mild to no disability was considered a dependent variable.
ResultsA moderate to maximum global disability was present in 43.6% of the sample. By areas, occupational functioning was the area most frequently affected, and personal care the least affected. The only variables which were associated with disability were the presence of medical comorbidity (P=.01), increased age (P=.005) global clinical severity (P=.0001) and in the depressive pole (P=.03). There was no relationship between clinical subtype, duration of the disease, number of previous episodes, number of hospitalisations, or other clinical variables and the degree of disability.
ConclusionsThese data underline the need to establish specific therapeutic strategies in the approach to depressive symptoms and medical comorbidity, with the aim of minimising the disability in elderly bipolar patients. Given the lack of current data, new studies are needed with larger samples and control groups.
Los estudios en pacientes bipolares adultos han demostrado una discapacidad asociada al trastorno bipolar, incluso en pacientes eutímicos, pero apenas hay datos en población anciana.
Material y métodoEstudio transversal y multicéntrico, en una muestra de pacientes bipolares (criterios DSM-IV-TR) ambulatorios, consecutivos, con edad igual o superior a 65 años. Se recogieron datos retrospectivos y transversales sociodemográficos y clínicos, además de la gravedad clínica global (ICG-BP-M) y el grado de discapacidad mediante la Escala de Discapacidad de la OMS (WHO/DAS). Se valoró la discapacidad global y por áreas. Se consideró variable dependiente la presencia de discapacidad de moderada a máxima frente a discapacidad de nula a ligera.
ResultadosEl 43,6% de la muestra presentó una discapacidad global entre moderada y máxima. Por áreas, el funcionamiento ocupacional resultó el área más frecuentemente afectada y la de cuidado personal la menos afectada. Las únicas variables con las que se relacionó la discapacidad fueron la presencia de comorbilidad médica (p=0,01), una edad mayor (p=0,005) y la gravedad clínica global (p=0,0001) y en el polo depresivo (p=0,03). El subtipo clínico, la duración de la enfermedad, el número de episodios previos, el número de hospitalizaciones y otras variables clínicas no mostraron asociación con el grado de discapacidad.
ConclusionesEstos datos subrayan la necesidad de establecer estrategias terapéuticas específicas para abordar los síntomas depresivos y la comorbilidad médica, con el fin de minimizar la discapacidad de los pacientes bipolares ancianos. Dada la escasez de datos actual, sería necesario realizar nuevos estudios con muestras amplias y grupos control.
While the estimated prevalence of type I and type II bipolar disorder (BP) is between 1% and 3% in the general population,1,2 epidemiological studies of elderly people estimate prevalence figures between 0.1% and 0.4% for BP.3,4 However, prevalence can reach 8–10% in institutionalised elderly patients or those in psychiatric hospitalisation units.5
The proportion of elderly people in Western societies is increasing at an unstoppable rate due to the population aging process, conditioned by the increase in life expectancy. The aging factor and the intense developments in medical healthcare in general—and psychiatry in particular—make an increase in the number of elderly people with mental illnesses under medical treatment foreseeable.
However, there is a significant deficit in knowledge of psychiatric disorders, excluding dementia, in elderly people.5,6 This deficit is more pronounced in the study of BP compared to other mood disorders, such as major depression.
Few multi-centre studies have been published to date. The literature specifically lacks studies with larger samples and data with respect to prevalence rates, aetiopathogeny, clinical variables and functioning in elderly bipolar patients. In addition, follow-up studies are rare in this population group. The articles that are published have several limitations that make generalisation difficult, as they are based on small samples composed of, generally, patients admitted for manic phases.7–9 Consequently, existing data almost exclusively pertain to patients with type I BP.The data currently available for the adult population show that mental illnesses, and specifically BP, produce significant functional impairment.10–16 This impairment is greater in some studies17 to that found for unipolar depression, even though it is not as serious as that associated with patients with schizophrenia.18,19 Unfortunately, there is little data with respect to the degree of impairment in elderly bipolar patients, although greater intensity would be predicted in this group compared to that in the adult population. This is due to the cumulative effect of affective episodes and the frequent presence of medical comorbidity and cognitive impairment, all of which are variables correlated with worse functioning often occurring in the elderly population.19–22
The scarcity of data in elderly bipolar patients is probably related to the methodological difficulties in studying this type of population. These studies should not only include the elderly who seek continuous treatment, but also those who are institutionalised and those who do not maintain contact with mental health centres.
The objectives of the present study were: to ascertain the degree of impairment shown in bipolar patients older than 65 years who continue outpatient treatment, to identify the areas of functioning most affected and to determine the sociodemographic, clinical and evolutionary variables most associated with impairment.
MethodsThis was a transversal and multi-centre study, in which patients in outpatient care (65 years or older) were recruited if they complied with DSM-IV-TR diagnostic criteria for BP. These patients were recruited from 5 psychiatric consultations in the mental health centres and the general hospitals of the Community of Madrid, the Community of Valencia and the Community of Murcia. Patients were included if they were able to understand the study procedures and give their informed consent. Patients were excluded from the sample if they were participating in a clinical trial.
Patients were evaluated in only 1 interview, in which sociodemographic, clinical and treatment data were collected. Likewise, their overall clinical severity was assessed using the Clinical Global Impression scale modified for bipolar disorder (CGI-BP-M).23 The degree of impairment was measured by the WHO Disability Assessment Schedule (WHODAS).24
The WHODAS is a scale designed so that the clinical professional can assess functioning and impairment in patients with mental disorders in general—psychotic disorders in particular—within the following areas: personal care, occupational area, family relations and social context.
In quantifying impairment, 2 parameters were considered: the intensity of the impairment (slight, moderate or severe) and its duration (at no time, a short time or some time, quite some time, most of the time or all the time). By combining both parameters, the clinician scored impairment in each of the areas, as well as overall impairment. The score could range from 0 to 5. Zero was given when there was no impairment, 1 if the impairment was minimal (slightly impaired for some time), 2 if the impairment was moderate (slightly impaired for quite some time or moderately impaired for a short time), 3 if the impairment was serious (moderately impaired for quite some time or severely impaired for some time), 4 if the impairment was very serious (severely impaired most of the time or moderately impaired all of the time) and 5 for maximum impairment (severely impaired all of the time).
Personal care was evaluated in relation to hygiene, dressing oneself, diet, etc. Occupational functioning considered how the patient functioned in paid work, in studies or in domestic tasks. Regarding the family variable, interaction with the spouse, children and parents was assessed. Social functioning was evaluated with respect to the patient's relationship with members of the community and participation in leisure and social activities.
The relationship between the different sociodemographic and clinical variables, and the degree of impairment and functioning in different areas were analysed. In the statistical analysis, degree of impairment between moderate and maximum was considered a dependent variable, such that patients with slight or no impairment were classified apart from those with a moderate, serious, very serious or maximum impairment.
The dependent variable was split so that the profile of patients with minimal or no impairment could be compared to those with at least a moderate impairment. The relationship between the independent qualitative variables and the dependent variable was analysed using chi-square tests, and Fisher's exact test when possible. The relationship between the qualitative and the quantitative variables was analysed using Student's t-test for difference in means.
The ethics committee of the La Paz University Hospital approved this study. In addition, the patients signed an informed consent form.
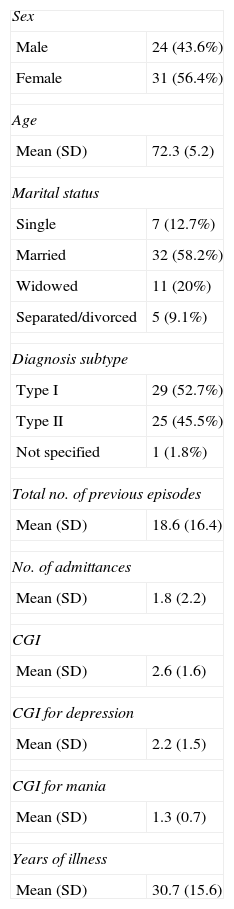
ResultsA sample of 55 patients in outpatient care was recruited from bipolar disorder consultations in the following healthcare facilities: La Princesa University Hospital, Madrid (n=15), San Blas Centre for Mental Health, Madrid (n=6), Fuencarral Centre for Mental Health, Madrid (n=11), La Fe Hospital, Valencia (n=17) and Murcia Hospital (n=6). The mean age was 72.3±5.2 years. In the sample, 56.4% of the participants were female, 58.2% were married and 20% were widowed. Regarding the diagnostic subtypes, 52.7% were diagnosed with BP-I, 45.5% with BP-II and 1.8% with non-specified BP (Table 1).
Sample description.
| Sex | |
| Male | 24 (43.6%) |
| Female | 31 (56.4%) |
| Age | |
| Mean (SD) | 72.3 (5.2) |
| Marital status | |
| Single | 7 (12.7%) |
| Married | 32 (58.2%) |
| Widowed | 11 (20%) |
| Separated/divorced | 5 (9.1%) |
| Diagnosis subtype | |
| Type I | 29 (52.7%) |
| Type II | 25 (45.5%) |
| Not specified | 1 (1.8%) |
| Total no. of previous episodes | |
| Mean (SD) | 18.6 (16.4) |
| No. of admittances | |
| Mean (SD) | 1.8 (2.2) |
| CGI | |
| Mean (SD) | 2.6 (1.6) |
| CGI for depression | |
| Mean (SD) | 2.2 (1.5) |
| CGI for mania | |
| Mean (SD) | 1.3 (0.7) |
| Years of illness | |
| Mean (SD) | 30.7 (15.6) |
According to the assessment of emotional state, 33 patients (60%) were in clinical remission, 15 (27.3%) were diagnosed with mild-moderate depression during the evaluation, 4 (7.3%) with severe depression without psychotic symptoms, 1 (1.8%) with severe depression with psychotic symptoms and 2 (3.6%) with hypomania.
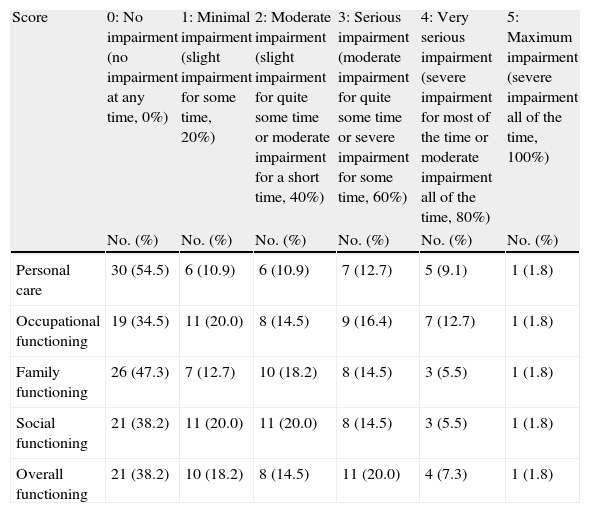
Most patients (56.4%) presented minimal or no impairment, 14.5% presented moderate impairment, 20% serious impairment, 7.3% very serious impairment and 1 case (1.8%) showed maximum impairment (Table 2).
Observed impairment in elderly patients, by areas of functioning.
| Score | 0: No impairment (no impairment at any time, 0%) | 1: Minimal impairment (slight impairment for some time, 20%) | 2: Moderate impairment (slight impairment for quite some time or moderate impairment for a short time, 40%) | 3: Serious impairment (moderate impairment for quite some time or severe impairment for some time, 60%) | 4: Very serious impairment (severe impairment for most of the time or moderate impairment all of the time, 80%) | 5: Maximum impairment (severe impairment all of the time, 100%) |
| No. (%) | No. (%) | No. (%) | No. (%) | No. (%) | No. (%) | |
| Personal care | 30 (54.5) | 6 (10.9) | 6 (10.9) | 7 (12.7) | 5 (9.1) | 1 (1.8) |
| Occupational functioning | 19 (34.5) | 11 (20.0) | 8 (14.5) | 9 (16.4) | 7 (12.7) | 1 (1.8) |
| Family functioning | 26 (47.3) | 7 (12.7) | 10 (18.2) | 8 (14.5) | 3 (5.5) | 1 (1.8) |
| Social functioning | 21 (38.2) | 11 (20.0) | 11 (20.0) | 8 (14.5) | 3 (5.5) | 1 (1.8) |
| Overall functioning | 21 (38.2) | 10 (18.2) | 8 (14.5) | 11 (20.0) | 4 (7.3) | 1 (1.8) |
Most patients presented minimal or no impairment (56.4%) on the lower levels of impairment, suffering mostly from impairment in occupational and social functioning.
Patients who presented obvious, serious, very serious or maximum impairment were impaired similarly in each area of functioning.
Among the areas of functioning, the best possible results—although with a few differences—were obtained in the personal care area, where 65.4% of patients showed minimal or no impairment, while 10.9% suffered from serious or maximum impairment.
In occupational functioning, 54.5% of the cases were recorded to have minimal or no impairment (Table 2).
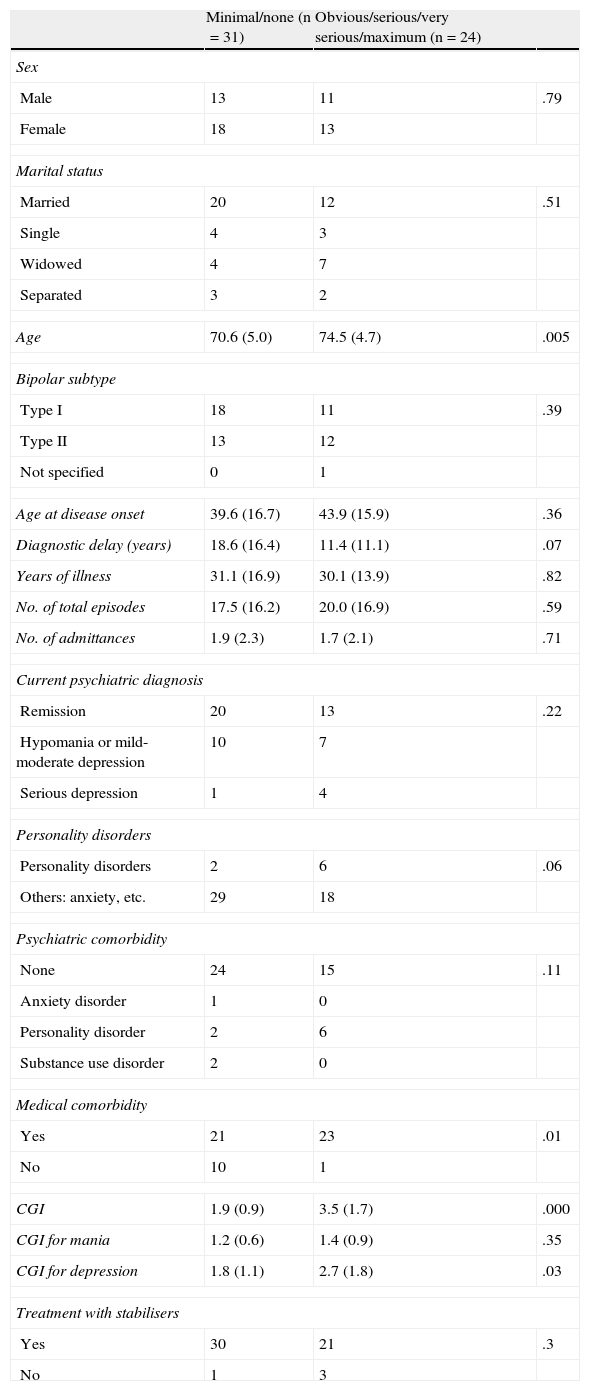
No significant association was found between the sociodemographic and clinical variables studied and the following variables: overall functioning, marital status, work situation, level of studies, previous psychotic symptoms, duration of the illness, number of previous episodes, number of previous admittances, emotional state during the assessment, psychiatric comorbidity or consumption of alcohol, tobacco or other drugs. Years of delay in diagnosis and diagnosis of a comorbid personality disorder presented a correlation that did not reach statistical significance.
The variables significantly correlated with moderate to maximum impairment were the following: older age, presence of physical comorbidity and higher score, either on the Clinical Global Impression scale or the CGI for depression (Table 3).
Sociodemographic and clinical variables correlated with some kind of impairment (obvious or maximum overall impairment).
| Minimal/none (n=31) | Obvious/serious/very serious/maximum (n=24) | ||
| Sex | |||
| Male | 13 | 11 | .79 |
| Female | 18 | 13 | |
| Marital status | |||
| Married | 20 | 12 | .51 |
| Single | 4 | 3 | |
| Widowed | 4 | 7 | |
| Separated | 3 | 2 | |
| Age | 70.6 (5.0) | 74.5 (4.7) | .005 |
| Bipolar subtype | |||
| Type I | 18 | 11 | .39 |
| Type II | 13 | 12 | |
| Not specified | 0 | 1 | |
| Age at disease onset | 39.6 (16.7) | 43.9 (15.9) | .36 |
| Diagnostic delay (years) | 18.6 (16.4) | 11.4 (11.1) | .07 |
| Years of illness | 31.1 (16.9) | 30.1 (13.9) | .82 |
| No. of total episodes | 17.5 (16.2) | 20.0 (16.9) | .59 |
| No. of admittances | 1.9 (2.3) | 1.7 (2.1) | .71 |
| Current psychiatric diagnosis | |||
| Remission | 20 | 13 | .22 |
| Hypomania or mild-moderate depression | 10 | 7 | |
| Serious depression | 1 | 4 | |
| Personality disorders | |||
| Personality disorders | 2 | 6 | .06 |
| Others: anxiety, etc. | 29 | 18 | |
| Psychiatric comorbidity | |||
| None | 24 | 15 | .11 |
| Anxiety disorder | 1 | 0 | |
| Personality disorder | 2 | 6 | |
| Substance use disorder | 2 | 0 | |
| Medical comorbidity | |||
| Yes | 21 | 23 | .01 |
| No | 10 | 1 | |
| CGI | 1.9 (0.9) | 3.5 (1.7) | .000 |
| CGI for mania | 1.2 (0.6) | 1.4 (0.9) | .35 |
| CGI for depression | 1.8 (1.1) | 2.7 (1.8) | .03 |
| Treatment with stabilisers | |||
| Yes | 30 | 21 | .3 |
| No | 1 | 3 | |
Our results confirmed that there is an elevated percentage of bipolar patients in the elderly population that suffer from significant impairment. Although 56.4% of the sample demonstrated minimal or no impairment, a high percentage of patients (43.6%) scored between moderate and maximum overall impairment, according to the WHODAS scale. The scarcity of data for the elderly made it difficult to compare our results with those in other samples.
There was a study that compared middle-aged and elderly bipolar patients who lived in the community with another group of schizophrenia patients and a control group, using various functioning indicators and various scales measuring quality of life or health condition. In this study, Depp et al.25 found that social functioning in the bipolar patient group was significantly worse than that of the control group and worse than that of even the schizophrenic patient group. It was also remarkable that remission of the affective symptomatology was associated with incomplete functional improvement.
The same group of researchers assessed day-to-day functioning in a recent article,26 using a sample of middle-aged and elderly bipolar patients. Analysis was done with subjective and objective measures, showing significant functioning impairment in the sample, greater than that in the control subjects. In addition, this functioning impairment was correlated with cognitive impairment.
In review studies of adult patients in general, 30–60% of the cases did not achieve occupational and social recovery11,16 after an affective episode, and 2/3 did not achieve complete functional recovery, even when in remission.15,27
The areas of functioning most affected in adult bipolar patients are usually the family, social and work areas.16 Regarding social functioning, our data were similar with respect to impairment percentages (41.8% had a moderate, serious, very serious or maximum degree of impairment). However, these figures may have been more serious than those obtained in adult patients by authors such as Goldberg and Harrow,28 who found that between 30 and 40% of the adult bipolar patients studied presented some degree of social impairment, despite being in clinical remission. In the same vein, several authors have found a significant deficit in social functioning for adult bipolar patients, even in a clinical remission situation.17,29
Family functioning is also impaired in bipolar patient samples. For example, the percentage of separated or divorced patients is greater than that in the general population.30 In 1 study, patients in primary healthcare that were identified as bipolar reported greater difficulties in family functioning.31 In our elderly patient sample, a high percentage (40%) showed moderate to maximum impairment in family functioning.
In adult bipolar patients, labour and occupational functioning were also significantly impaired.32,33 Less than 50% of the patients with bipolar disorder were actively working or working full time.34 In addition, these patients typically suffered reductions in income and labour status.17 In the data from a sample recruited in our surroundings,35,36 only 42.4% of the adult patients worked full time at the time of assessment. Among retired elderly patients—where it is not possible to assess their labour functioning but instead their functioning in being occupied—45.4% of the cases presented between moderate and maximum impairment and only 34.5% did not suffer any impairment. The area of personal care turned out to be the least affected, as almost 2/3 of the sample presented minimal or no impairment, and only 1/3 of the patients showed between moderate and maximum impairment. However, in assessing these apparently positive results, it should be considered that the sample consists of elderly patients that (despite occasionally needing some kind of help) are capable enough to live in a normalised environment. It is also very possible that they did not represent all elderly bipolar patients, but rather only those who live at home and can access specialised outpatient care.
Similar to what has occurred in many studies of functionality in bipolar patients,21,22 most clinical and sociodemographic variables in our study (such as sex, marital status, age at disease onset, years of illness or type of current pharmacological treatment) showed no significant relationship with the degree of functional impairment. Furthermore, no differences were observed based on diagnostic subtype: patients with type I BP had a degree of impairment similar to that of patients with type II BP disorder, as has been tested very recently in non-elderly patient samples.37
In our sample, patients without impairment had a mean age of 70 years, while those that suffered between serious and maximum impairment had a mean age of 75 years. Rosa et al.22 also found that older age was associated with greater functional impairment in a sample of adult bipolar patients.
Comorbidity with a significant medical pathology was associated with greater impairment in this study. This result, as expected, was observed38 in elderly patients with unipolar depression.
Both the Clinical Global Impression scale (CGI) and the depression subscale (CGI-D) were associated with impairment. This result was expected, as the clinician uses the Clinical Global Impression scale to assess the severity of the illness, including psychopathological aspects but also functional aspects. Regarding the association between a higher CGI-D subscale score and greater impairment, our findings were similar to those in other studies,12,39 in which 1 of the most consistent variables in predicting functional impairment was the presence of depressive symptomatology, but not the presence of hypomanic symptomatology.
Study strengths: This study was 1 of the few that assessed impairment specifically in a sample of elderly bipolar patients treated in outpatient care.
Study limitations: The limited sample size reflects how difficult it is to recruit broad groups from the elderly population, specifically patients undergoing follow-up in outpatient clinics (this difficulty could possibly explain the scarcity of publications on this topic). Small sample size can also limit the generalisation of results and reinforces the need to organise more multi-centre studies. The absence of a control group consisting of non-bipolar elderly participants prevented us from differentiating the specific impairments, consequences of the bipolar illness and impairments derived from problems associated with age. Furthermore, cognitive impairment was not specifically assessed in patients. In any case, none of the patients included complied with diagnostic criteria for dementia.
When this study was designed, there were no specific instruments validated to measure impairment in the Spanish bipolar population. A general impairment scale was consequently used. Currently, the Functioning Assessment Short Test (FAST)40 is available specifically for bipolar disorder and it has been validated for the Spanish population.
In conclusion, there is little published data on functioning and impairment in elderly bipolar patients, and our data confirmed significant functional impairment in almost half of the elderly bipolar patients in outpatient treatment. The only variables that were correlated with this impairment were the following: presence of medical comorbidity, older age, overall clinical severity and specifically depression. Clinical subtype, duration of the illness, number of previous episodes, number of hospitalisations and other clinical variables showed no association with degree of impairment.
These data highlight the need to establish specific therapeutic strategies to address depressive symptoms and medical comorbidity in an effort to minimise impairment in elderly bipolar patients.
Ethical disclosuresProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of data. The authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consent. The authors have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence is in possession of this document.
Conflict of interestThe authors have no conflict of interest to declare.
Please cite this article as: Ezquiaga E, et al. Discapacidad en pacientes bipolares ancianos en tratamiento ambulatorio. Variables asociadas. Rev Psiquiatr Salud Ment (Barc.). 2012;5:183–90.