In order to reduce distress associated with working with COVID-19 patients, several psychological intervention programmes for healthcare workers have been developed in Spain. We aimed to describe the main characteristics and components of these programmes for healthcare workers treating COVID-19 patients in Spanish hospitals.
Material and methodsAn online survey was designed to evaluate the main characteristics of psychological intervention programmes for healthcare workers during the first wave of COVID-19 pandemic.
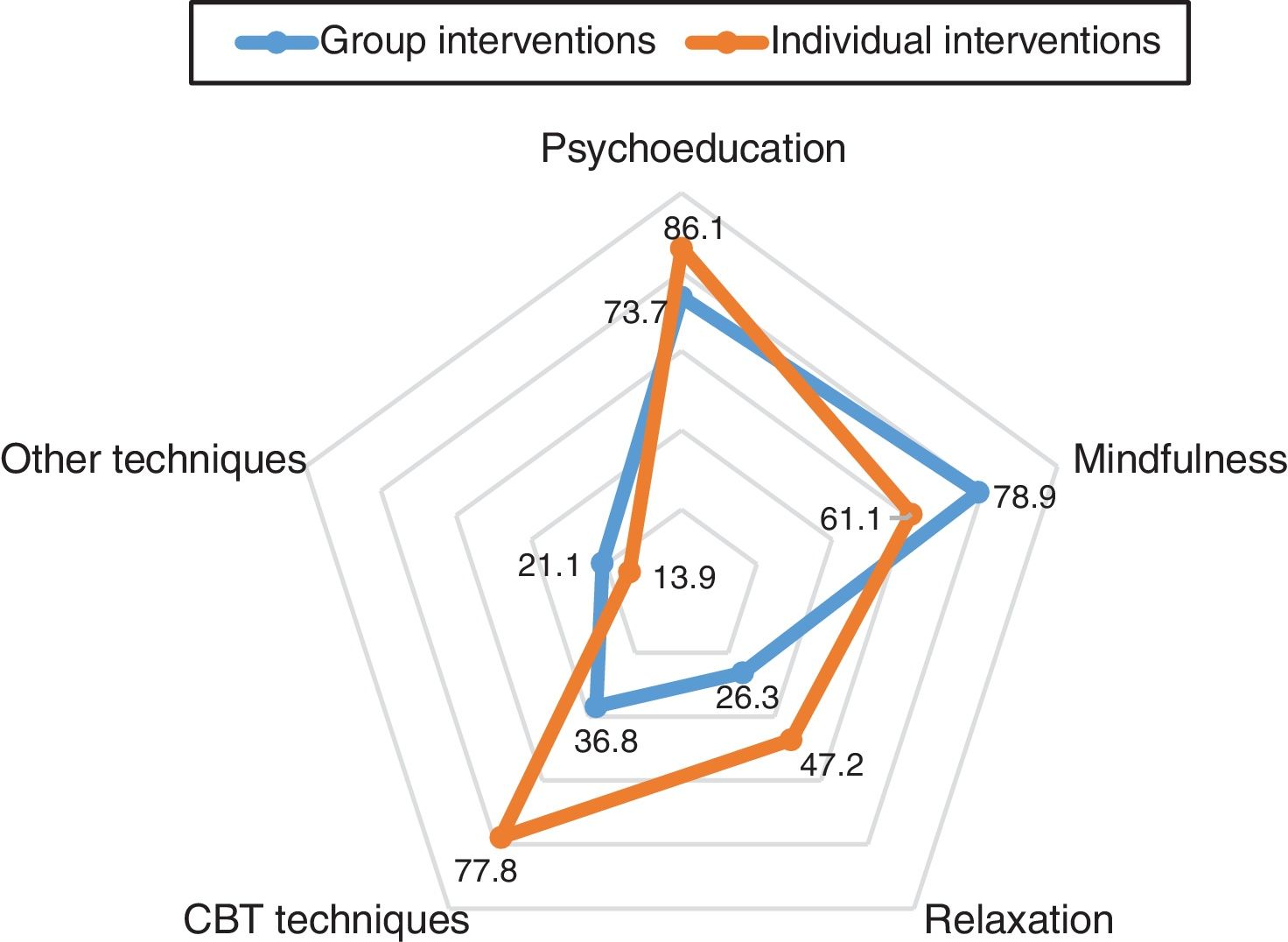
ResultsValid responses were received from 36 hospitals. Most of these programmes offered both in-person and online therapy. The most common aim of these interventions was emotional regulation, which was treated by psychoeducational and cognitive-behavioural techniques in individual interventions. Group interventions mainly used psychoeducation and mindfulness. Only half of the teams that offered in-person interventions received training in the proper use of personal protective equipment.
ConclusionsSeveral hospitals in Spain have developed mental health interventions for healthcare workers during the COVID-19 pandemic, deploying a wide range of therapeutic modalities and techniques. The rapid implementation of these programmes during the pandemic suggests that safety may not have received sufficient attention. The planning and development of interventions for healthcare workers during pandemics merits greater attention by national and regional authorities and institutions.
Para reducir el malestar psicológico asociado a tratar pacientes con COVID-19, se han desarrollado numerosos programas de intervención en España. Este estudio pretende describir las principales características y componentes de los programas para trabajadores sanitarios que atienden COVID-19 en hospitales españoles.
Material y métodosSe elaboró y distribuyó una encuesta online para evaluar las principales características de los programas de intervención psicológica para trabajadores sanitarios durante la primera ola de la pandemia de COVID-19.
ResultadosSe recibieron respuestas válidas de 36 hospitales. La mayoría de los programas ofrecían intervención presencial y online/telefónica. El principal objetivo de estos programas fue mejorar la regulación emocional. Las intervenciones individuales emplearon principalmente psicoeducación y técnicas cognitivo-conductuales, mientras que las grupales emplearon psicoeducación y mindfulness. Solo la mitad de los equipos que ofrecían intervenciones presenciales habían recibido la formación adecuada para usar equipos de protección individual.
ConclusionesNumerosos hospitales en España han desarrollado intervenciones de salud mental para trabajadores sanitarios durante la pandemia por COVID-19, empleando una gran variedad de modalidades terapéuticas. La rápida implementación de estos programas durante la pandemia sugiere que la necesidad de seguridad ha podido subestimarse. La planificación y desarrollo de intervenciones psicológicas durante las pandemias merece mayor atención por parte de las autoridades competentes.
The outbreak and the rapid spread of the coronavirus disease 2019 (COVID-19) has become pandemic and is threatening the health of people around the world.1 One of the countries facing the most severe crisis is Spain, with more than 377,906 confirmed cases of COVID-19 and 28,813 deaths as of August 21, 2020.2 The rapid increase in cases of COVID-19 in Spain is threatening the capacity of the well-established Spanish National Health System (Spanish acronym, SNS).3 As a result, the workload for healthcare professionals has increased substantially, with prolonged hours of work and higher stress due to the potential risks involved in this work, which is common cause of burnout and mental health disorders during outbreaks of infectious diseases.4 These same problems were also detected in during the COVID-19 outbreak.5,6 Furthermore, a recent meta-analysis found that, during the COVID-19 pandemic, healthcare workers show significant levels of depression, anxiety and insomnia symptoms.7 However, it is noteworthy that these prevalence studies are based on self-report screening questionnaires rather than diagnostic interviews, which may result in an overestimation of the real prevalence.
Previous research conducted in health care workers involved in treating patients with an infectious disease during an outbreak has shown an increase in short and long-term mental health problems in these populations. Several studies have shown that, during the outbreak of the Severe Acute Respiratory Syndrome (SARS) in 2003, health care workers were at increased risk of developing psychological distress,8,9 which persisted over time.10 During the 2015 outbreak of the Middle East Respiratory Syndrome (MERS) in Korea, most healthcare workers who treated quarantine hemodialysis patients had an increased risk of developing post-traumatic stress disorder (PTSD)-like symptoms compared to professionals not involved in performing those tasks.11
To manage the psychological problems in China during the COVID-19 outbreak, several psychological intervention programmes were developed in Chinese hospitals to support frontline health care workers.12–14 However, the efficacy of these interventions was partially reduced due to certain impediments. For example, medical doctors and nurses were frequently reluctant to participate in psychological interventions, as their focus was on ensuring better working conditions, including adequate rest periods and better protective equipment and safety.13 Other authors have pointed to difficulties in developing these interventions, mainly: (1) problems with planning and implementation of the interventions, (2) problems in cooperation and decoupled interventions from mental health services and community health services, and (3) an excessive number of volunteers (e.g., counsellors, nurses or teachers) in the intervention teams, with a scarce number of mental health professionals.15
Sadly, over 54,000 health professionals have been infected with the coronavirus in Spain,2 among the highest infection rates among healthcare professionals worldwide.16 Given that the risk of contagion is one of the main stressors during a pandemic, frontline healthcare workers in Spain are particularly vulnerable to developing mental health issues.17–19 To reduce the distress associated with working with COVID-19 patients, many hospitals in the SNS have developed mental health interventions to assist these professionals. However, no comprehensive study has been performed to date to determine the characteristics of these psychological interventions, including their active components, their duration and availability, or the conditions in which they were implemented. Furthermore, although common guidelines have been proposed for the physical health care of patients with COVID-19, no consensus or common guidelines have been developed for mental health interventions in the context of COVID-19.
In this context, the aim of the present study was to assess and describe the main characteristics and components of psychological intervention programmes offered to healthcare workers treating COVID-19 patients in Spanish hospitals during the peak of the outbreak.
Materials and methodsStudy procedureAn ad hoc online survey was designed in Google Forms (Google LLC). The survey assessed the most relevant variables in mental health interventions for healthcare workers, including data related to the following: site, training of team members, main objectives, characteristics of the interventions, setting, working hours, implementation of the programme, and personal protective equipment (PPE), among others (see Appendix A). The survey was distributed to mental health professional societies and key SNS hospitals using mailing lists provided by those organizations, and also distributed on social media. The survey was available online from March 23, 2020 to April 5, 2020. Participation was voluntary and no compensation was given.
The present study has been authorized by the Valdecilla Biomedical Research Institute (IDIVAL) Internal Scientific Committee (Santander, Spain). No ethics committee approval was needed because the study did not involve any personal data from human subjects.
Eligibility criteriaOnly data from public or semi-public (public–private) hospitals were considered as these institutions were responsible for treating most COVID-19 patients. Responses from other healthcare services or private hospitals were not considered. Only responses from members of mental health services at public or semi-public hospitals were included. In some cases, more than one individual from the same hospital responded to the survey. In these cases, any discrepancy was resolved by contacting the intervention team directly.
Statistical analysisDescriptive statistics are presented. Non-parametric tests (phi and Kruskal–Wallis H test) were performed to compare variables. All statistical analyses were performed using the Statistical Package for Social Sciences (SPSS, v.19.0).
ResultsWe received a total of 50 responses. We discarded duplicate responses (same hospital, n=10 responses) and those from other mental health services that did not fulfil the eligibility criteria (n=4, one response each from the following: primary care centre; health consortium; a programme not associated with the SNS; and one response without any information). Finally, mental health intervention programmes from 36 hospitals were considered valid for further analysis. Respondents were mainly members of the intervention teams (n=29; 80.6%) or coordinators of those teams (n=6; 16.7%).
Most hospitals were based in the regions of Madrid (n=8; 22.2%), Barcelona (n=7; 19.4%), or Valencia (n=4; 11.1%). The other hospitals (n=17; 47.2%) were widely distributed around the country. The full list of participating hospitals is available in Appendix B. The median number of beds at the participating hospitals was 466 (interquartile range [IQR]=508). Thirty-four programmes were created in hospitals to care for their own staff, while the other two programmes were created by regional health systems to serve multiple hospitals.
All the intervention programmes were created ad hoc to manage mental health issues in healthcare workers during the COVID-19 pandemic. The most common objectives of the programmes were as follows: (1) “to improve emotion regulation” (n=35; 97.2%), (2) “to reduce physiological arousal” (n=31; 86.1%), (3) “to improve the professionals’ communication skills with their patients” (n=19; 52.8%), and (4) “to improve communication among the members of medical teams” (n=16; 44.4%). The median (IQR) time required to prepare the programmes, defined as the time elapsed between the start of clinical interventions and the first preparation meeting, was 5 (5) days. Note that two programmes began clinical interventions before the first team meeting and four began on the same day of the first team meeting. These programmes were created after a proposal made by mental health professionals (n=23; 63.9%), the director of mental health services (n=9; 25.0%), hospital management (n=3; 8.3%), and others (n=1; 2.8%).
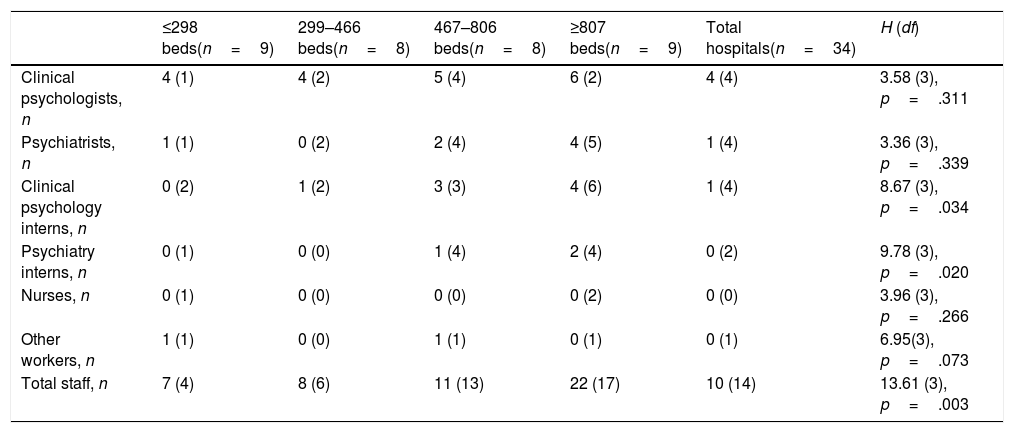
Psychological intervention teams had a median (IQR) of 10 (14) members. The teams were composed of clinical psychologists (50.1%), clinical psychology interns (18.1%), psychiatrists (15.6%), psychiatry interns (7.2%), and other staff (9.0%). Table 1 shows the professional profile categorized by hospital size. The presence of newly hired personnel (one site) or volunteers (five sites) was infrequent. More than half of the teams included professionals with specific training in emergencies and disaster situations (n=21; 58.3%). Most of the team leaders were clinical psychologists (n=19; 52.8%).
Staff members, working hours, and preparation time for the interventions, by hospital size (quartiles).
| ≤298 beds(n=9) | 299–466 beds(n=8) | 467–806 beds(n=8) | ≥807 beds(n=9) | Total hospitals(n=34) | H (df) | |
|---|---|---|---|---|---|---|
| Clinical psychologists, n | 4 (1) | 4 (2) | 5 (4) | 6 (2) | 4 (4) | 3.58 (3), p=.311 |
| Psychiatrists, n | 1 (1) | 0 (2) | 2 (4) | 4 (5) | 1 (4) | 3.36 (3), p=.339 |
| Clinical psychology interns, n | 0 (2) | 1 (2) | 3 (3) | 4 (6) | 1 (4) | 8.67 (3), p=.034 |
| Psychiatry interns, n | 0 (1) | 0 (0) | 1 (4) | 2 (4) | 0 (2) | 9.78 (3), p=.020 |
| Nurses, n | 0 (1) | 0 (0) | 0 (0) | 0 (2) | 0 (0) | 3.96 (3), p=.266 |
| Other workers, n | 1 (1) | 0 (0) | 1 (1) | 0 (1) | 0 (1) | 6.95(3), p=.073 |
| Total staff, n | 7 (4) | 8 (6) | 11 (13) | 22 (17) | 10 (14) | 13.61 (3), p=.003 |
Data are given as medians (IQR). Hospital size is categorized in quartiles. Kruskal–Wallis statistic (H) compares the differences among the four groups of hospitals; df, degrees of freedom.
Most intervention programmes (n=21; 58.3%) included in-person interventions while the remaining programmes (n=15; 41.7%) were performed exclusively online or by telephone. Only 11 programmes (30.6%) were manualized while 16 (44.4%) were supervised. Nineteen programmes (52.8%) included group interventions. Fig. 1 shows the main components of the individual and group interventions. Multimedia materials (video, audio, or mobile phone application) were available at 15 sites (41.7%). Thirteen programmes (36.1%) included pharmacological interventions.
All teams with in-person interventions used some type of protective gear (masks, gloves, gowns). However, performing in-person interventions was not associated with having received training for the correct use of PPE (phi=0.19; p=.257): about half of teams performing in-person interventions had received such training for the proper use of personal protection equipment (n=11).
The interventions were available a median (IQR) of 11 (5) hours each day. Nineteen out of 36 programmes (data missing for one site) offered care from Monday to Friday while 17 out of 36 were available seven days per week (Monday to Sunday). The majority of the intervention programmes were offered to most professional categories: physicians (n=35; data missing for one site; 100%), nurses (n=33; 94.3%); nursing assistants (n=30; 85.7%), and other staff members (n=29; 82.9%).
DiscussionThis is the first study to describe mental health interventions for healthcare workers in Spanish hospitals during the first wave of COVID-19 pandemic. Our results show that, prior to the national lockdown, several hospitals in Spain had developed some type of intervention to improve emotion regulation and/or to reduce anxiety/stress among hospital staff. These interventions were delivered both online and in-person, mostly using bottom-up schemas.
Studies conducted in China found that the most reported interventions were online or telephone-based.14,20 Similarly, in Spain, most of the hospitals surveyed offered these types of interventions. However, in contrast to China, a high proportion (58.3%) of the participating hospitals in Spain provided in-person psychological interventions, both individual and group. This is relevant given that recent research has shown that nurses and doctors are generally reluctant to participate in psychological interventions during the COVID-19 pandemic13 and almost half of them are not interested in engaging in any structured wellness resource,21 either because they felt well enough to work without them at this time or because they had other priorities19,22 (for example, improvements in workplace safety or resting periods). Moreover, other studies have shown that in-person psychological interventions are generally better accepted than online interventions23 and are likely to be preferred by healthcare workers during the COVID-19 pandemic.21 Consequently, it is important to offer in-person therapy options, which could potentially increase participation in those programmes. Nonetheless, Duan et al. argue that the presence of mental health professionals in areas of the hospital with COVID-19 patients should be discouraged to minimize the risk of contagion.15 Although teams performing in-person interventions in Spain used the proper protection materials, a high proportion of them had not received the appropriate training in the use of these materials. Clearly, proper training in the use of PPE is essential and should be offered to all mental health teams.24
In terms of the content of the interventions evaluated in our study, we found that psychoeducation and mindfulness were highly prevalent, both for group and individual interventions. By contrast, the main approach for individual interventions was cognitive-behavioural therapy.
Another aim of some of the interventions in Spanish hospitals was to improve communication within the medical team. Some organizations strongly recommend these type of intervention as they can reduce the anxiety associated with uncertainty and dysfunction in communication flows.25,26
The interventions in the present study were delivered mainly by mental health specialists, primarily clinical psychologists. This is important and a positive feature of these programmes, especially given that one of the main issues detected in China was the high number of volunteers delivering these interventions.15 Mental health professionals are preferable over volunteers as they guarantee higher professional skills, are better integrated within the health care system and ensure the continuity of care over the time. However, a wide range of different interventions was offered at these hospitals, and there was a notable lack of coordination among the institutions and no national guidelines were available. Better coordination among hospitals would likely improve the quality of the interventions, in part by ensuring that “best practices” are used.
During the COVID-19 outbreak in China, it has been found that depression and anxiety levels among healthcare workers were higher in women, nurses, professionals working in a secondary hospital, and frontline workers (direct contact with patients).7,27 Most of the psychological interventions developed in Spanish hospitals covered all frontline workers (including nurses and doctors), thereby providing this population, which is at high risk of developing mental health issues, with the necessary tools to prevent or cope with the stress.
Although there was a clear necessity during the pandemic to quickly develop and implement mental health programmes for healthcare workers, this has raised several issues. As our results show, some hospitals implemented these interventions with scant preparation, even commencing the interventions before conducting preparatory meetings. This implies that safety issues might have been overlooked (e.g., appropriate training in the use of PPE).
The present study has several limitations. First, the study is based on a convenience sample. We did not systematically collect data from all Spanish hospitals (about 492 public and semi-public hospitals). Thus, it is probable that some types of interventions were not considered. Moreover, the proportion of hospitals offering such psychological interventions for healthcare workers remains unknown. Furthermore, other programmes developed by different institutions (i.e. professional associations, non-governmental organizations) outside the SNS were not included. However, the main objective of the present study was to describe the characteristics of the interventions for healthcare workers, in order to inform decision making during the pandemic. It is likely that a more complex design would need more time and, consequently, cause an unwanted delay in access to information. Second, the study period is limited to the first wave of the pandemic in Spain, and some interventions may have been developed and implemented later to treat distress associated with a different phase of the pandemic. By contrast, the study has several important strengths. For example, all of the data was directly provided by members of the teams involved in the interventions, thus increasing the validity of these data. Also, the rapid assessment of these programmes allows us to precisely describe the psychological interventions deployed during the peak of the pandemic.
Future research should seek to more comprehensively evaluate the intervention programmes, including their acceptability, safety, efficacy, and effectiveness. According with a systematic review,28 no study has assessed the efficacy or effectiveness of stress reduction techniques for health care workers during pandemics. Only limited information about pilot interventions have been provided. For instance, Rodríguez-Vega et al. reported a mindfulness-based stress reduction intervention, supporting its utility, safety and feasibility.29 Furthermore, Blake et al. developed a digital learning package for healthcare workers in the United Kingdom, which included evidence-based guidance, support and signposting relating to psychological wellbeing.30 Besides usability, utility and user satisfaction with the content, little is known regarding the relative efficacy of different components and formats of the interventions. However, intervention programmes conducted in Spain included some recommendations for psychological interventions, like ensuring online or telephone interventions,14 promoting professionals engagement through in-person interventions21 or improving communication within medical teams.26 It is important that future studies systematically assess the efficacy of psychological interventions and its modalities, components, and common factors, in order to identify those with better results in the context of a health emergency.
A long-term, longitudinal approach is needed to assess the evolution of mental health of healthcare workers and the effects on mental health of potential risk factors for burnout.31 In addition, the development of electronic health technologies for psychological treatment and evidence-based self-help interventions during pandemics is warranted.32,33
ConclusionThe response of mental health teams to the first wave of COVID-19 pandemic in Spanish hospitals included diverse psychological interventions for healthcare workers. These interventions may have enhanced emotion regulation skills among health care workers and helped to prevent the incidence of mental disorders. However, the rapid development of these interventions has raised questions about potential safety issues and about the scant prior preparation for a health emergency of this magnitude. In this regard, specific mental health intervention programmes should be developed for healthcare workers and included in national and international contingency plans for pandemics and other emergency situations.
Conflict of interestsThe authors declare that they have no conflict of interest.
The study was supported by a grant from the Valdecilla Biomedical Research Institute – IDIVAL (PRIMVAL19/01) awarded to Dr. Priede; and grants from the Valdecilla Biomedical Research Institute – IDIVAL (PRIMVAL18/03 and INT/A19/02) awarded to Dr. González-Blanch. The sponsor did not participate in the design or conduct of this study; in the collection, management, analysis, or interpretation of data; in the writing of the manuscript; or in the preparation, review, approval, or decision to submit this manuscript for publication.