The wide spectrum of COVID-19 symptoms, ranging from mild manifestations to severe pulmonary damage and mortality, prompted this study to investigate the relationship between clinical symptoms and complement system (CS) activation in COVID-19 patients.
Materials and methodThis retrospective study focused on 100 PCR-positive COVID-19 individuals admitted to Imam Khomeini and Bu Ali hospitals in Sari City from April to June 2021. The levels of C3 and C4 proteins in their blood were measured using nephelometry, and CH50 tests were done with single radial immunodiffusion to determine the activity of CS.
ResultsThe study found that high blood pressure, smoking, and diabetes were the most common underlying conditions among the patients, with prevalence rates of 29%, 24%, and 23%, respectively. Positive correlations were found between C4 and CH50 levels and the presence of cough and rhinorrhea in the subjects. Stratifying patients into 2 groups based on cough or rhinorrhea revealed a significant difference in CH50.
ConclusionThe findings suggest that COVID-19 patients with hypertension or diabetes mellitus may benefit from targeting CS for disease management.
El amplio espectro de síntomas de COVID-19, que van desde manifestaciones leves hasta daño pulmonar severo y mortalidad, impulsó este estudio a investigar la relación entre los síntomas clínicos y la activación del sistema del complemento (CS) en pacientes con COVID-19.
Materiales y métodoeste estudio retrospectivo se centró en 100 personas con COVID-19 con PCR positiva admitidas en los hospitales Imam Khomeini y Bu Ali en la ciudad de Sari de abril a junio de 2021. Los niveles de proteínas C3 y C4 en la sangre se midieron mediante nefelometría y Se realizaron pruebas de CH50 con inmunodifusión radial única (SRID) para determinar la actividad de CS.
ResultadosEl estudio encontró que la presión arterial alta, el tabaquismo y la diabetes eran las afecciones subyacentes más comunes entre los pacientes, con tasas de prevalencia del 29%, 24% y 23%, respectivamente. Se encontraron correlaciones positivas entre los niveles de C4 y CH50 y la presencia de tos y rinorrea en los sujetos. La estratificación de los pacientes en dos grupos según la tos o la rinorrea reveló una diferencia significativa en CH50.
ConclusiónLos hallazgos sugieren que los pacientes con COVID-19 con hipertensión o diabetes mellitus pueden beneficiarse al abordar la CS para el manejo de la enfermedad.
On December 29, 2019, medical professionals at a hospital in Wuhan, China, observed an unusual pattern of pneumonia cases. The SARS-CoV-2 virus, responsible for the COVID-19 pandemic, has spread to all corners of the globe, resulting in numerous fatalities.1 Symptoms of this disease vary from mild (such as fever, headache, muscle aches, and infrequently, digestive disorders) to severe lung damage and fatality. The virus is primarily transmitted through the respiratory tract.2,3 COVID-19 can lead to severe consequences for society and especially for individuals who are at higher risk, such as heart patients, diabetics, those with immune system deficiencies, and elderly people. Additionally, a country's healthcare system can experience staggering costs due to diagnostic interventions, treatments, long-term hospitalizations, and the loss of human resources. Mental problems may also become more prevalent. Therefore, it is imperative to take appropriate health measures to prevent the spread of this disease.4,5
In case of an emergency, it is crucial to quickly identify all suspicious cases and isolate them to cut-off the source of infection. In this situation, developing and improving identification methods can quickly identify infected or asymptomatic carriers and prevent further spread of the disease. Identifying the nucleic acid of the virus in nasopharyngeal samples and lower respiratory tract secretions6,7 or checking the presence of specific antibodies of the SARS-CoV-2 virus in the serum are current diagnostic methods for diagnosing the acute phase of the disease, carriers, and recovered people.7–9 The innate and acquired immune systems play crucial roles in protecting our body against coronavirus or intensiting further damage to different tissues. Therefore, gaining a better understanding of how these systems function in response to the coronavirus can be a valuable way to control the disease and develop new treatments.10
The complement system (CS) is an important part of innate immunity that responds quickly to invading microorganisms.11 It consists of more than 20 serum proteins that interact with other regulatory molecules on the cell surface to destroy microbes and viruses.12 The CS is activated in various pathways, but the process of activation and termination remains the same in all of them. The proteins in this system act on each other in a sequence of reactions, where the product of each reaction affects the next one (C2–C4).13 In the end, some complement components have accumulated on the membrane surface of a microorganism (C5–C9), they create holes in the membrane, which causes it to become permeable. This process is known as the membrane attack complex. As a result, fluids can enter the microorganism and destroy it.14 Since studies suggest that the activation of the CS may contribute to the inflammation intensity and tissue damage of COVID-19, the severity of symptoms may be also related to the degree of activation of the CS. Therefore, in this study, we investigated the relationship between clinical symptoms and the activation of CS in patients who tested positive for COVID-19 through polymerase chain reaction (PCR). The levels of C3 and C4 in serum, along with the CH50 test, were employed to assess CS activation.
MethodsStudy designThe study centered on 100 PCR-positive COVID-19 patients who were admitted to Imam Khomeini and Bu Ali hospitals in Sari City from April to June 2021. A trained nurse collected 5 ml of blood from each patient in a tube without anticoagulant and forwarded it to the laboratory for analysis. The samples underwent centrifugation at 3000 rpm for 10 min to isolate the serum, which was subsequently stored at −70 °C in the immunology laboratory freezer until the completion of sample collection and testing. The study received approval from the Ethics Committee of Islamic Azad University, Chalous (IR.IAU.CHALUS.REC.1401.015) and all participants provided informed consent before participating in the study and completing the questionnaire.
Measurement of serum levels of C3 and C4 components of complementThe levels of C3 and C4 were measured to assess CS activity due to their high consumption during the activation process.15 The levels of C3 and C4 proteins in serum were measured using the nephelometry method, using the Binding Company's protein measurement kit from the UK. The patients' serum, positive, and negative control samples were diluted 1:11 with physiological serum, as instructed by the kit. Next, 40 μl of the diluted samples were added to the Minineph device, which contains a magnet. The amount of these protein levels were determined using nephelometry method for COVID-19 patients.16
Measurement of complement activity with CH50 testTo measure the activity of the CS and to screen 9 main components of this system (C1–C9), the CH50 test was performed using the Single Radial Immunodiffusion method and IraGen kit in patients and control group.16
Statistical analysisThe data were analyzed using SPSS software version 24.0. To assess the significant difference in mean values of complement components between patient groups categorized based on the presence or absence of clinical symptoms, the t-test was employed. Furthermore, the Spearman correlation test was utilized to investigate the correlational relationship between clinical symptoms and serum levels of complement components. Classification and relative risk were performed using Chi Square test when necessary. The data is presented as mean±SD. A significance level of less than .05 was considered.
ResultsThe correlation between COVID-19 and 2 key factors: Age and sexIn this study, 100 individuals aged between 17 and 79 who tested positive-PCR for COVID-19 were evaluated. Of these individuals, 57 were women and 43 were men. The results indicated that there was no significant difference in COVID-19 incidence based on age (p=.811) or gender (p=.841).
Underlying diseases and the risk of contracting COVID-19The current study revealed the prevalence of different comorbidities among COVID-19 patients. The findings indicated that hypertension, smoking, and diabetes mellitus were the 3 most commonly observed underlying conditions, present in 29%, 24%, and 23% of the patients, respectively. The study also found that the prevalence of cardiovascular disease and systemic autoimmune diseases was lower among the subjects.
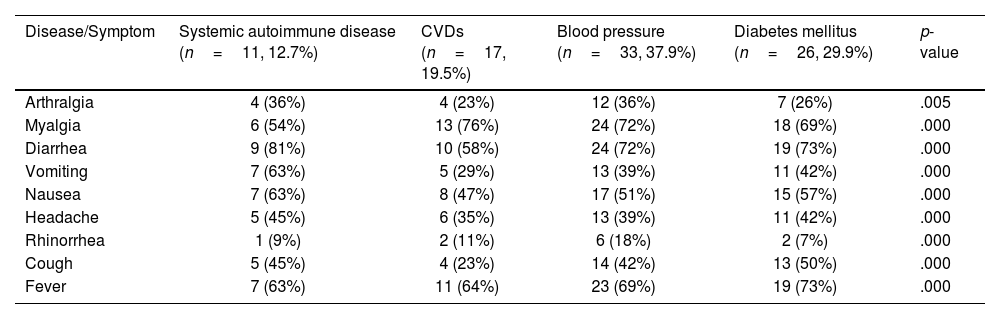
The most frequently observed symptoms in COVID-19 patientsThe clinical symptoms observed among the patients revealed that fever, with an incidence rate of 17%, was the most commonly reported symptom. Both diarrhea and myalgia were reported in 15% of the subjects. Cough was observed in 12% of the samples, while symptoms of rhinorrhea or runny nose were present in 5% of the samples. Headache was reported by 10% of the subjects, while 11% experienced nausea and 9% reported vomiting. Additionally, 6% of the patients reported arthralgia. Table 1 shows the frequencies of different symptoms among COVID-19 patients with various clinical backgrounds. Here, the difference in the rate of the symptoms were compared among patients. Chi square analysis revealed that arthralgia (p=.005) and all other symptoms occurred with significant different (p=.000) in frequencies among patients with various comorbidities.
Frequency of symptoms among COVID-19 patients with different background diseases.
| Disease/Symptom | Systemic autoimmune disease (n=11, 12.7%) | CVDs (n=17, 19.5%) | Blood pressure (n=33, 37.9%) | Diabetes mellitus (n=26, 29.9%) | p-value |
|---|---|---|---|---|---|
| Arthralgia | 4 (36%) | 4 (23%) | 12 (36%) | 7 (26%) | .005 |
| Myalgia | 6 (54%) | 13 (76%) | 24 (72%) | 18 (69%) | .000 |
| Diarrhea | 9 (81%) | 10 (58%) | 24 (72%) | 19 (73%) | .000 |
| Vomiting | 7 (63%) | 5 (29%) | 13 (39%) | 11 (42%) | .000 |
| Nausea | 7 (63%) | 8 (47%) | 17 (51%) | 15 (57%) | .000 |
| Headache | 5 (45%) | 6 (35%) | 13 (39%) | 11 (42%) | .000 |
| Rhinorrhea | 1 (9%) | 2 (11%) | 6 (18%) | 2 (7%) | .000 |
| Cough | 5 (45%) | 4 (23%) | 14 (42%) | 13 (50%) | .000 |
| Fever | 7 (63%) | 11 (64%) | 23 (69%) | 19 (73%) | .000 |
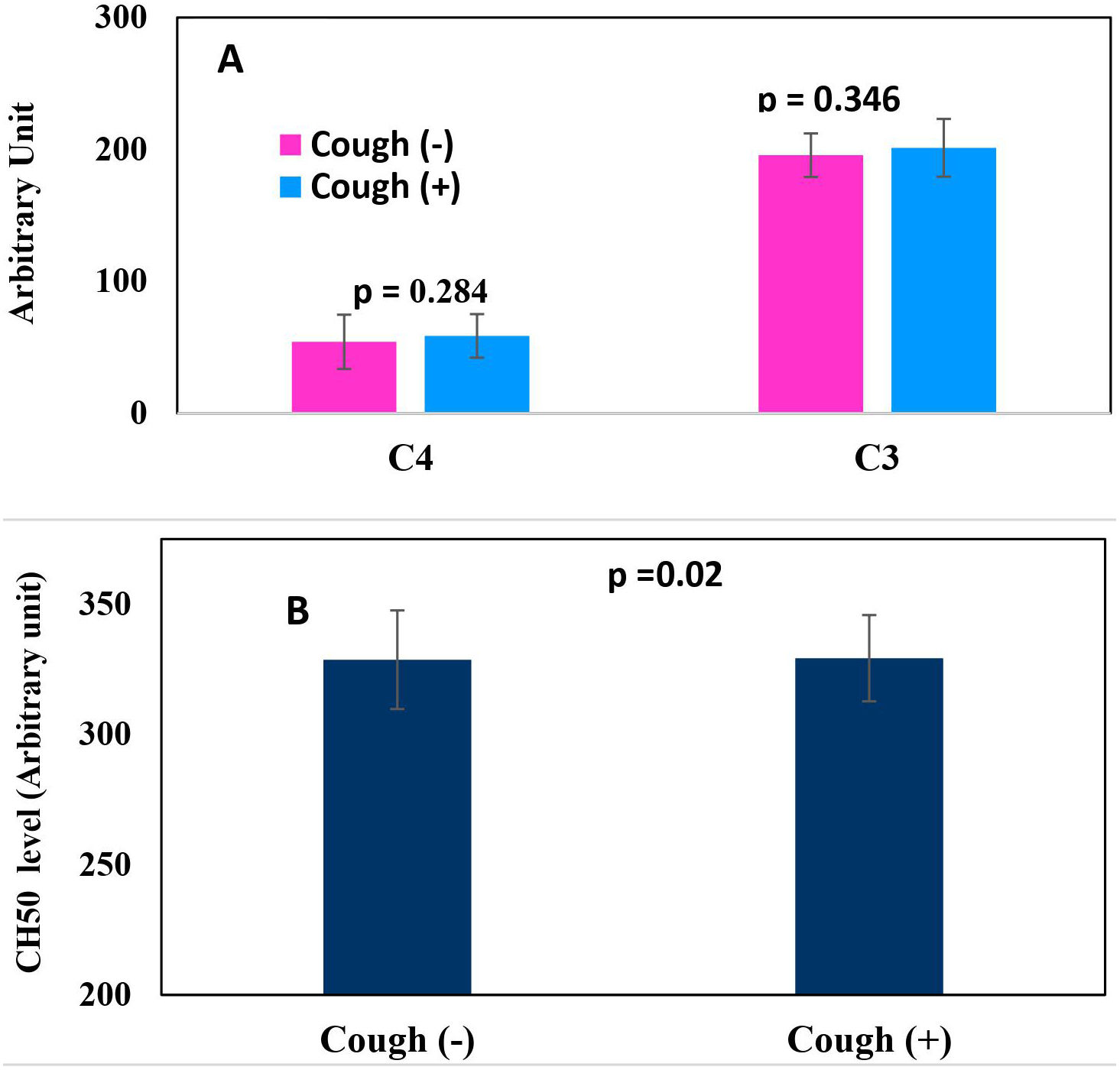
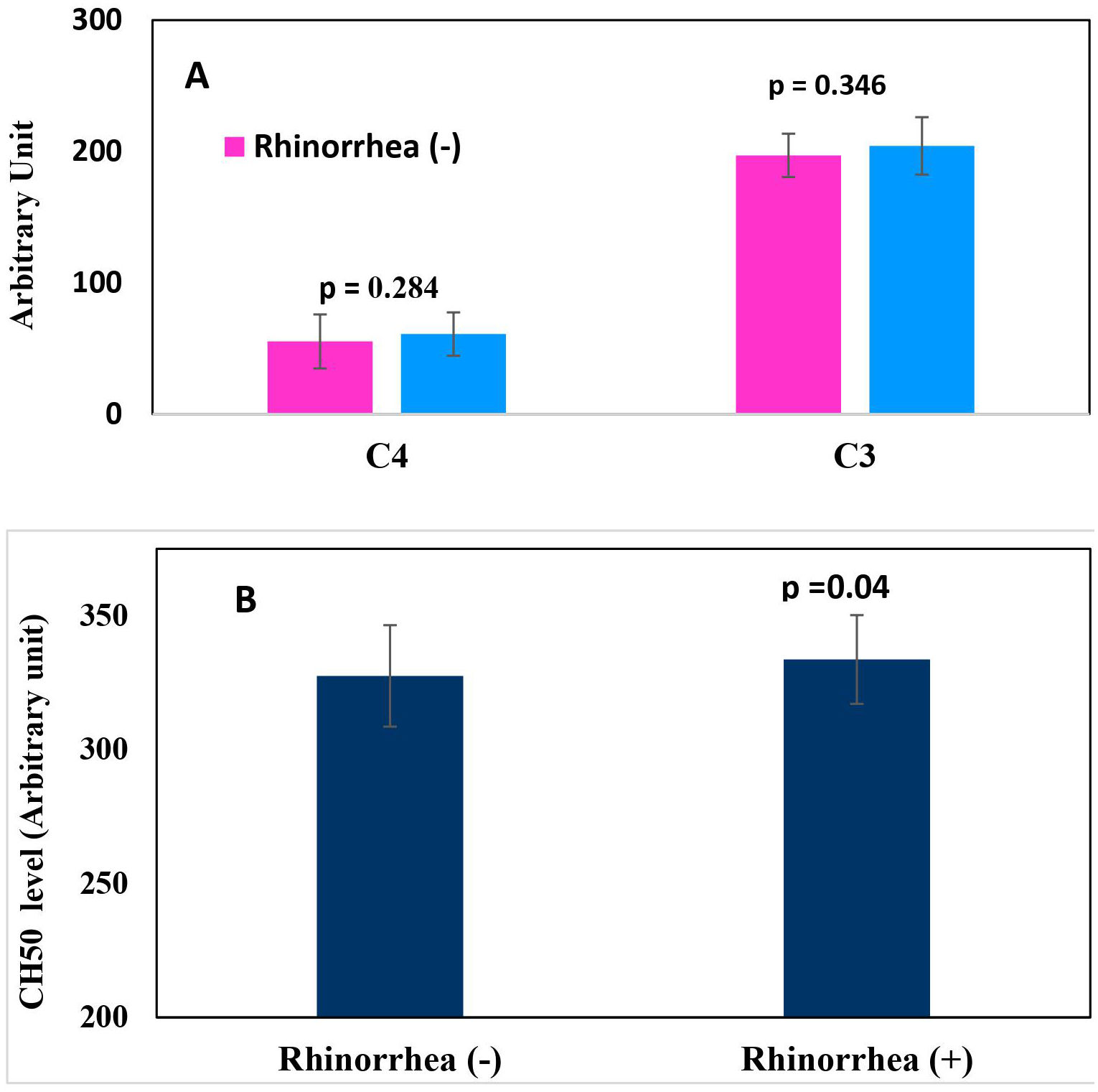
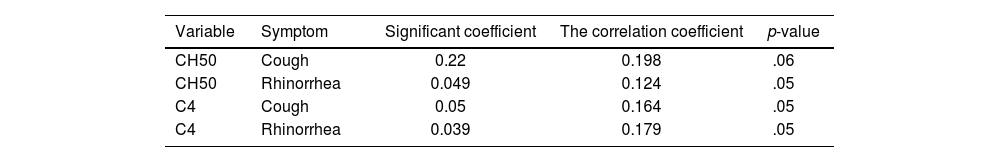
The study analyzed serum levels of CS components by measuring C3, C4, and CH50 in COVID-19 patients. The results showed that there was no significant difference in the levels of C3 or C4 between patients with or without cough (p>.05). Nonetheless, there were notably elevated CH50 levels in COVID-19 patients with cough (p<.05) (Fig. 1A and B). Furthermore, there was no significant difference in the levels of C3 or C4 between patients with or without rhinorrhea. However, there were significantly heightened CH50 levels in COVID-19 patients with rhinorrhea symptoms (p<.05) (Fig. 2A and B). The analysis of the correlation between serum levels of complement components and clinical symptoms in COVID-19 subjects was conducted using the Spearman statistical test. As indicated in Table 2, cough and rhinorrhea exhibited significant correlations with C4 and CH50 (p<.05), while C3 showed no correlation with clinical symptoms in the patients (p>.05).
The study aims to investigate the role of CS among individuals with COVID-19 in Mazandaran Province, Iran. To assess the impact of CS on the occurrence of COVID-19 symptoms, we measured serum levels of C3 and C4, and conducted CH50 tests. The study also examined a correlation between complement activation and some clinical manifestations. In addition, in this study, researchers also investigated the correlation between COVID-19 and various underlying diseases. The damage caused by the entry of the SARS-COV-2 into the lung causes the initiation of various immune responses such as the release of cytokines and chemokines, the absorption of immune cells into the tissue, the activation of the blood coagulation pathway and thrombosis in the lung, which results in the occurrence of acute respiratory distress syndrome (ARDS).17
Our findings indicated that patients with symptoms of cough and rhinorrhea had higher levels of C3 and C4 than those without symptoms. However, this difference was not statistically significant. Additionally, patients with symptoms exhibited a higher level of CH50 compared to asymptomatic patients. This suggests a higher activity of the CS in patients experiencing symptoms. In line with our findings, Guan et al. reported complement activation in COVID-19 and demonstrated that the rise of C3 worsens disease in ARDS associated with SARS-CoV.18 Gralinski et al. found that C3-deficient mice had less respiratory dysfunction with SARS-CoV despite equal viral loads in the lungs compared to control.19 A recent study showed that measuring levels of C3a and/or C4a (fragments of C3 and/or C4) in the blood may be a useful tool to predict the risk of lung injury in COVID-19 and other immune-related diseases. These free blood fragments (C3a and/or C4a) indicate the decomposition of C3 and C4 and the activity of CS.20
A variety of COVID-19 symptoms have been observed, with cough being more prominent than rhinorrhea.21 Our data revealed a significant correlation between cough and rhinorrhea manifestations and the values of either C4 or CH50 in the subjects. The increased levels of C4 or CH50 in our patients raise the question of whether cough or rhinorrhea predispose individuals to SARS-COV-2 infection or if these manifestations occur as outcomes of the disease. There are conflicting data regarding the impact of cough or rhinorrhea-causing comorbidities on the course of COVID-19.7 One study has reported asthma as a potential risk factor for COVID-19 infection.22 Beken et al. showed that asthma and atopic did not increase hospitalization in COVID-19.23 Thus, it appears that cough and rhinorrhea are not the pathological context of COVID-19, but rather occur as a result of SARS-COVID-19 infection. However, further studies are needed to determine whether cough or rhinorrhea-causing comorbidities are related to the severity of COVID-19.
Our study found that blood pressure and diabetes were more common in COVID-19 patients. These findings parallel some other studies,18,21,24,25 which also showed a similar pattern of comorbidities. A longitudinal cohort study by Engström et al. revealed that hypertension is associated with increased plasma levels of C3 and C4.26 Magen et al. showed a significant positive correlation between systolic blood pressure and C3 levels in patients with resistant arterial hypertension compared to those with controlled arterial hypertension.27 Similarly, Chen et al. reported a higher incidence of intensive care unit stays in the hypertension group compared to the non-hypertension group (p<.05). Their logistic regression analysis also showed that hypertension was an independent risk factor for death.28 Elevated levels of C3 and C4 are also reported in diabetes patients.29,30 Like hypertension, diabetes mellitus is also associated with a significant risk of complications, extended hospital stays, and mortality in COVID-19-infected patients.31 Due to the contextual role of the CS in promoting COVID-19 pathology and the increased levels of C3 and C4 in patients with blood pressure and diabetes, may explain why patients with blood pressure or diabetes are more susceptible and have more severe COVID-19 symptoms.28,32 Understanding the intricate interplay between the CS, pre-existing conditions, and COVID-19 pathogenesis is crucial for developing targeted therapeutic interventions and improving patient outcomes in these high-risk groups.
ConclusionsOur study has shown that there is a direct relationship between the activation of the CS and the prevalence of cough and rhinorrhea in COVID-19 patients. Additionally, our results showed that people with hypertension and diabetes are at a higher risk of contracting COVID-19. The results indicate a possible connection between the CS activation, comorbidities such as hypertension and diabetes, and the exacerbation of COVID-19 severity. This emphasizes the necessity for further investigation into the mechanistic role of the CS in the development of COVID-19 in these high-risk patient populations.
FundingThis research received no external funding.