The last two decades have seen a strong movement towards evidence-based medicine, with an emphasis on supporting clinical decision making by sound scientific evidence. A major tool of the evidence-based-medicine movement has been the grading of levels of evidence [1]. Another tool supporting the process of clinical decision making is the opinion of experts for which several methods of consensus have been developed. An expert consensus method in turn depends, in large part, on the evidence the consensus is based on [1]. A further step in the same direction leads us to clinical practice guidelines (CPG) which integrate evidence-based-medicine supported recommendations or statements with the work of groups of experts for various purposes.
In our specialty, hepatology, most liver specialists regard clinical guidelines developed by well recognized professional and academic organizations such as the American association for the study of the liver (AASLD), the European association for the study of the liver (EASL), the Latinamerican association of liver diseases (ALEH), the various Japanese biliary and hepato-biliary associations and societies, the Canadian association for the study of the liver (CASL) and the Asian Pacific association for the study of the liver (APASL) and others, as an authoritative body of knowledge as well as reference for decision making. The topic coverage by all of them has been extensive, 21 and 30 CPGs to date by just the AASLD and EASL with experience of 20 and 10 years respectively. The coverage by all the organizations has been vast including most areas where there has been a need for a well recognized guideline. Nevertheless, not infrequently specialists from many countries have found that some of those guidelines do not apply fully to their patients or their environments arguing demographic and epidemiological differences between different populations. Others argue the questionable applicability of some measures or interventions in countries or places with different settings and resources [2]. Thus the need to develop their own CPG to apply in their local or regional setting.
In that sense the Latin American (LA) region has been pro-active and there are examples of different initiatives culminating in the publication of CPGs from different associations and organizations e.g. at least 17 CPGs (Latin American) from 10 different countries and 5 CPG from ALEH itself [3]. Nevertheless there is still some discussion about the justification for developing more CPG for the region and, as expected, there are different views of how to develop them (who, where, when, and how). In favour of developing new LA CPG there are strong arguments related to the genetic, demographic and some particularities specific or endemic to the Latin American region and its populations. For instance, the human populations within the American continent (Canada, United States of America (USA), and LA countries) are rich in genetic variability due to the historical admixture between the New World (Amerindian) and Old World (European and African) ancestries. This variability is heterogenic based on the distribution of the risk or protective alleles and their interactions with the environment, and they may account for differences in the natural history of chronic liver diseases that need to be identified. These gene-environmental interactions are the main topic of genomic medicine studies that search for the individuals or populations who are at risk and for the prevailing predisposing factors. Finding such differences is crucial for elaborating regional CPGs with an impact on the prevention and management of chronic liver diseases. There are several examples of why we need to distinguish in which way LA populations are different from those in the USA, Europe or Asia. One example is the case of viral hepatitis B (HBV) for which there are at least eight HBV genotypes circulating worldwide. However, they do not cause the same rate of morbidity and mortality due to chronic hepatitis, cirrhosis and hepatocellular carcinoma everywhere. HBV genotypes F and H are endemic among the native amerindians of South America and Mexico, respectively. These genotypes show greater adaptability with the host's genetic and immunological profile that may give rise to frequent occult B infection that requires further study [4,5]. On the other hand, genotypes A and D isolated from LA people with European or African ancestry may manifest differently [6]. In the same line of ideas, phylogeographical and evolutionary analyses conducted in Brazil and Argentina have enlightened our knowledge of the origin and spread of certain HBV subgenotypes throughout the local regions and their potential risk for the host of chronic infection, cirrhosis and liver cancer [7,8]. In a similar case, hepatitis C virus (HCV) genotypes and subtypes are also regionally distributed, which in turn is linked to the routes of transmission among certain risk groups. As for spontaneous clearance, response to antiviral treatment and treatment side effects, these may be modulated by the prevalence of risk-allele profiles of the IL28B/IFNL4 (rs12979860 T>C, rs8099917 G>T) or ITPA (rs1127354 C>A) polymorphisms among populations [9,10]. On the other hand, the use of the direct-acting antivirals (DAA) which is not equally feasible in all LA countries [11] may also be hindered by the natural occurrence of mutations of drug resistance in the HCV genome [12]. Thus revealing the genotypes/subgenotypes not only is important to trace their spread throughout the continent; it is relevant for the understanding of how these regional host–virus interactions may influence the clinical outcome, either due to viral dynamics or human gene polymorphisms that may lead to or avoid virus-related cirrhosis or hepatocellular carcinoma. In the case of alcoholism, taste receptor genes, brain reward system genes and alcohol-metabolizing genes in humans are highly polymorphic and have been associated with the risk of alcoholic cirrhosis [13]. Therefore, the management of alcoholic liver disease requires recognizing their prevalence and how they interact with lifestyle and social–behavioral factors related to the specific pattern of alcohol drinking among the distinct LA populations [14].
Non-alcoholic fatty liver disease (NAFLD) driven by the obesity epidemic is escalating worldwide as well as in LA [15]. It is comprised of a spectrum of distinct phenotypes (steatosis, non-alcoholic steatohepatitis, fibrosis, cirrhosis, and liver cancer), some of which are polymorphic, causing significant liver-related morbidity and mortality. To date, no unique pharmacological regimen has effectively reverted on-going NAFLD and genomic medicine could open some alternatives. For this problem there is no universal diet and since no two populations are similar, a regionalized nutritional strategy based on the genetic background and tailored by population including regional foodstuffs and food culture has been proposed [16,17].
An exhaustive review of the fast-growing evidence that appears in the literature on the genetic epidemiology of the LA populations and its impact on liver disease falls out of the scope of this Viewpoint. However, CPGs based on the systematic evaluation of research performed in such populations would come closer to resolving local health problems. This argument seems more reasonable than just reproducing, adapting or simply translating foreign CPGs. Furthermore, CPGs are mainly focused on the principle of using evidence-based medicine for treatment whereas currently, genomic medicine and translational research provide knowledge on how to prevent diseases and morbidity based on the factors that predispose each population.
There are also different opinions as to who should steer the initiative(s), who should organize the CPG development process, where should the developing and steering groups meet, who should be the sponsor, where should the funding be sought? One person alone cannot answer many of these questions but certainly the answer could be the result of group discussions at ALEH meetings with representatives from the different participating national societies. As a proposal, the first question to be discussed could be the need to have Latin American clinical guidelines, which answer we could envisage being affirmative. This article has been written as a result of many discussions and deep reflexions some of which included in the editorial section of Annals of Hepatology and partly as a result of the scholarly work of the Medical decision making academic group of the Department of medical clinics at the Health Sciences Center (CUCS) of the University of Guadalajara, Mexico.
2Consensus methodsAt present evidence-based guidelines derived from rigorously conducted controlled studies outperform expert opinion [1]; however, in the real world there are instances where there is insufficient scientific-based evidence for a particular problem that needs to be addressed. For those reasons, various group consensus methods incorporate opinions of a group of experts rather than an individual expert in a formalized manner. Consensus methods are a form of reaching agreement by incorporating opinions of a group of experts in a formalized way [1] leading to a statement or in a broader sense a “guidance”. They are usually endorsed by a major academic, scientific or both, organization [18]. There are several methods to reach consensus on a topic under study. Some of the best known are: Delphi study, nominal group, RAM method and Consensus development conferences.
2.1Delphi studyA Delphi study is a method developed in the 1950s by scientists at the RAND corporation that has subsequently been used in healthcare and Medicine to develop consensus on group opinion and establish guidelines [1]. It consists of a structured questionnaire distributed to a group of experts who express their opinion anonymously through at least two rounds until a prespecified level of consensus is reached. This method has the advantage of not requiring a face to face contact.
2.2Nominal groupThe nominal group also called the expert panel method is derived from social-psychological studies of decision conferences also used for developing consensus practice guidelines [1]. It is a method of consensus that allows a group of experts to develop and suggest ideas or solutions within a group in an initial phase. It is a face-to-face structured group meeting that is led by an experienced moderator [1]. This method is often used in combination with the Delphi method described above.
2.3RAND-UCLA appropriateness method (RAM)This procedure has been used in the United States for assessing appropriateness of a number of procedures such as coronary angiography, upper gastrointestinal tract endoscopy and other conditions [1]. This method usually involves two interdependent groups: core panel and an expert panel. While RAM was initially used for assessing appropriateness of a procedure, it has been applied to the development of practice guidelines and classification criteria [1].
2.4Consensus development conferencesConsensus development conferences are organized meetings of experts in a given field, and depending on the topic of the conference may require a mixture of experts from various fields to create a multidisciplinary approach to the topic at hand. The most well-developed application has been used by the National institutes of health (NIH) of the USA [1].
3Clinical practice guidelinesClinical practice guidelines (CPG) are “systematically developed statements to assist practitioner and patient decisions about appropriate health care for specific clinical circumstances.” (Institute of Medicine, 1990)[19]. The clinical practice guideline contains systematically developed statements including recommendations aimed to optimize patient care and assist physicians and other health care practitioners and patients to make decisions about appropriate health care for specific clinical problems [2,19].
Recently a new version of CPG PracticeGuidances was published by the AASLD [18] where experts participate providing a consensus statement on a topic that lacks sufficient data to perform systematic reviews [20].
3.1Purposes of CPGAccording to International Society for Quality in Health Care CPG are intended to improve effectiveness and quality of care, to decrease variations in clinical practice and to decrease costly and preventable clinical mistakes and adverse events [21]. Sometimes when accepted by some national superior organism they may provide some legal protection to conforming clinicians or at least reduce their exposure to medical liability.
CPG can include best-practice statements regarding screening, diagnosis, management or monitoring [21] and in many cases they are supplemented with simple to elaborated algorithms that aid in the understanding and clarity of the statements.
There are important characteristics regarding quality, efficiency, transparency and applicability that should be considered in the development of a CPG [20].
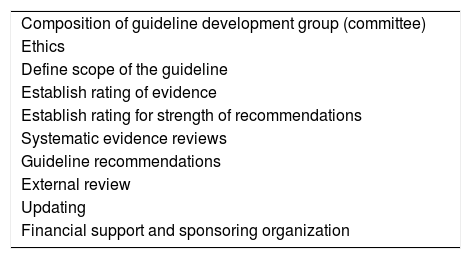
3.2DevelopmentGuidelines are usually developed by a designated group of experts selected and organized by a well established and recognized professional or academic institution or association [21]. In some cases a health authority or government organization plays a central role and in a few cases a CPG is the product of small teams of dedicated volunteers working with limited funding and variable understanding or experience with CPG development methods [21]. There are several well recognized manuals including guideline development standards set by leading international organizations [2,19] describing the process of constructing and developing a CPG [2,19,22]. An initiative by McMaster University conducted a review of the methodological content of more than 30 international CPG development manuals producing a thorough checklist [23]. Guidelines are developed using clinically relevant questions, which are then answered by systematic reviews of the literature and followed by data-supported recommendations (Table 1).
Core elements of a CPG.
| Composition of guideline development group (committee) |
| Ethics |
| Define scope of the guideline |
| Establish rating of evidence |
| Establish rating for strength of recommendations |
| Systematic evidence reviews |
| Guideline recommendations |
| External review |
| Updating |
| Financial support and sponsoring organization |
The guideline development group (GDG) or committee should be a diverse, multidisciplinary and balanced group of specialists and experts in particular topics comprising clinicians, specialists in basic sciences, statistics, methodology and a representative of the population of patients [20,22]. The GDG is responsible for reviewing the evidence, translating it into practice recommendations, writing the guideline, and assuring that the recommendations are not biased by being based on factors other than the best available scientific evidence [20,22].
3.4EthicsThe ethical context for a CPG is a fundamental part in any process of guideline development and as such are the ethical principles involved with it [20].
Those principles are applied in the concepts of independence, transparency, conflicts of interest (COI), adherence to a ethics code and the CPG themselves (i.e. development process) [19,24]. COI are defined as any circumstance(s) that produce a risk that some actions or professional judgments regarding a specific interest will be improperly influenced by a secondary interest [24] and are thoroughly described by many CPG manuals [19,24].
3.5Defining the scopeThe scope will inform the problem, the type of population affected, the interventions or approaches, the expected outcomes, establish the focus for the recommendations as well as the priorities and the key questions that will govern the search for evidence [2,19].
3.6PICO questionsThe first and most important step to begin a systematic literature review is to prepare the questions the review is expected to answer. They will determine the scope, eligibility criteria, type of studies to look for, type of data and outcomes among other things [25]. The review questions should specify the types of population (participants), types of interventions (and comparisons), and the types of outcomes that are of interest elements; that conforms the acronym PICO [2,25]. A concise and general background is provided to bring context to the questions and evidence profiles are prepared for each PICO question for which a systematic review was done. Each question follows with an associated recommendation. Technical remarks accompany each recommendation, which serve to facilitate its implementation. A summary of the evidence profile and rationale is then presented, ending with a section addressing areas of future research opportunities relevant to that question [18].
3.7Determining the quality of scientific evidenceJudgments about the quality of scientific evidence and grade of recommendations in healthcare are intricate [18]. However a more systematic approach to make those judgments was developed evolving into an almost universally adopted system for grading the quality of the evidence and the strength of recommendations, the GRADE system [26]. GRADE categorizes the quality of evidence as high, moderate, low or very low [2]. This will allow explicit determination of the strength of recommendations.
3.8Determining the strength of recommendationsA systematic approach to making judgments about the recommendations has been widely adopted, the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) system mentioned above [18,26]. There are two types of strengths of recommendation: strong recommendation and weak or a conditional recommendation. As for clinicians, this means that patients should receive the recommended course of action, with consistent benefits and limited of few side effects [18].
4CommentaryAt present, evidence-based medicine requires better methods of medical decision making among which CPGs are one of the most frequently used tools to achieve best clinical practices. Most accepted CPG are developed by academic, professional and sometimes governmental organizations and published by recognized journals including standards for development and quality. It has been shown that Latin American populations have specific gene-environmental interactions making them different from North American, European and African populations thus the need to study and analyze in which cases CPG need to be developed to address liver problems in the region.
Conflict of interestThe authors declare that there is no conflict of interest regarding the publication of this article.