Hepatocellular carcinoma (HCC) is one of the leading causes of cancer-related death worldwide. Interestingly, the great majority of individuals affected by the tumor have underlying liver disease, therefore narrowing the population to be screened. Still, however, there is a clear lack of blood biomarkers, and surveillance in those at risk is performed by frequent imaging of the liver. A variety of multinational collaborations are currently invested in finding biomarkers for HCC based on liver-produced proteins. A new approach with assessment of peripheral proteins might be necessary for the successful early detection of this malignancy.
Elsa (not her real name) is 36 years old. In December 2017 she was diagnosed with cirrhosis secondary to hepatitis B infection (HBV), after being referred to a tertiary hospital in Quito, Ecuador due to a gastrointestinal bleed from esophageal varices. She has since remained stable and on treatment for HBV. Due to her HBV-related cirrhosis she was advised to undergo hepatocellular carcinoma (HCC) surveillance with ultrasound, the gold standard, every 6 months. Elsa lives in Tepapare, Pastaza province, in the Ecuadorian Amazon. To comply with her HCC surveillance she undertakes a 6–8h canoe trip through the Amazon River, followed by a 5-h bus ride to Quito. Although until present time she has followed her surveillance instructions properly, her primary hepatologist in Quito is unsure that she can undertake such a commute for a long period of time. Elsa's example is not isolated, but a rather common scenario of individuals with cirrhosis residing in rural settings in many regions of the world.
HCC is the most frequent malignancy of the liver and the second most common cause of cancer-related death worldwide. HCC has a specific particularity: it does rarely-to-never occur in a healthy liver. The great majority of HCCs occur in a setting of underlying cirrhosis. Indeed, individuals with liver cirrhosis, depending on the initial cause of liver disease, have an approximate 50% risk of HCC over a 10 year period [1].
One would assume that with such a specific population to target, the scientific community would have developed screening technologies for early identification of HCC in those at risk. Sadly, this is not the case: in the current standard of care individuals with advanced liver disease are advised to return to the clinic every 6 months to undergo ultrasonographic examination of the liver with the goal of “visually” identifying a tumor small enough to be amenable to curative treatment. Despite the non-invasive nature of ultrasound, the frequency of the testing, time-consuming appointments and preparation (individuals have to stop eating or drinking hours before the test) lead to poor adherence as individuals grow tired and miss appointments. This explains why Edenvik et al. reported that only 30% of HCC diagnoses occur through surveillance in Sweden, and Singal et al. reported 24% proper surveillance for HCC in the United States, which improved to 47% only after specific efforts in reaching patients were attempted [2,3]. These issues are more prevalent in Latin America where access to hospitals for imaging is limited, work permits for medical exams are scarce and cultural factors lead to individuals shying from frequent health visits. A recent analysis from the South American Liver Research Network (SALRN) of more than 1300 HCC cases revealed that over half of them were diagnosed outside of surveillance [4].
There is a clear and obvious need for new biomarkers in order to easily detect early HCC. These biomarkers should be sensed in blood and ideally in intervals longer than 6 months. The scientific community and industry, as well as the hepatology community as a whole, are fully aware of this and efforts have been placed to achieve early HCC detection via blood tests. Nonetheless, biomarkers that have so far been identified do not reliably predict the development of HCC in those at risk.
A commonly used biomarker for HCC is alpha-fetoprotein (AFP). However, the sensitivity and specificity of this protein is quite low and the most important professional societies for liver disease do not advocate its use in isolation as levels show significant variation in individuals with and without HCC [5]. The GALAD model (which combines age, gender and 3 blood biomarkers) has shown promise, but it is unclear how it performs in different populations. Other biomarkers that have been studied or proposed with variable degrees of success are glypican-3, alpha-glucosidase, AFP-L3 and des-gamma-carboxy prothrombin (DCP) [6–8]. However, none of these are ready for prime time and we still rely on ultrasound for surveillance and early detection.
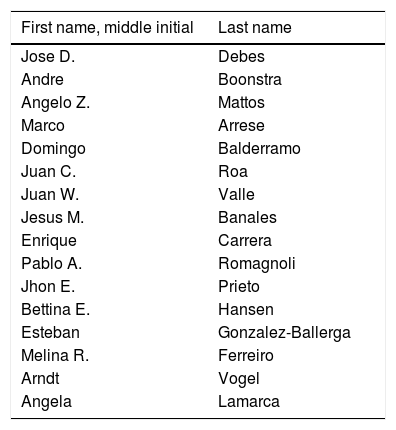
The rationale for the proposed biomarkers for HCC screening (mentioned above) is based on the understanding that a tumor will produce a protein that can be detected in blood. However, HCC presents an array of complexities, such as a highly variable genetic component and variable protein productions depending on the cause of underlying liver disease. One other particularity of HCC is that it develops from an inflammatory environment in the majority of cases (the environment that leads to cirrhosis). Therefore, the immune system in these individuals is inter-related to the formation of the tumor likely from very early stages, even when the tumor is not detectable by imaging. Interestingly, a recent study from our group in a small cohort of HCV patients found that immune markers detected in blood could predict HCC development up to 2 years in advance [9]. It is with this in mind, that a group of clinicians and researchers from Europe, North America and South America joined forces to form ESCALON (European-South American Consortium to Assess Liver-Originated Neoplasia). One of the main goals of this multinational initiative is to validate immune-related markers that could predict HCC early on, with a blood test. The concept is simple, albeit important: “to use the immune reaction of the body to predict early tumor development”. We expect that this approach will eventually allow providers to detect HCC earlier than a “6-month period” likely extending surveillance time to once a year or more and also minimizing discomfort by subjecting a patient to a simple blood draw. Besides ESCALON, other multinational initiatives are studying novel biomarkers for HCC. The common goal amongst of all of them is the same: that the Elsas of this world don’t have to endure heroic hurdles to undergo cancer surveillance.
FundingThis project has received funding from the European Union's Horizon 2020 research and innovation program under grant agreement No. 825510, the Robert Wood Johnson Foundation, AFMDP and NIH-NCI R21 CA215883-01A1 to JDD.