When a patient safety incident (PSI) occurs, not only the patient, but also the involved health professional can suffer. This study focused on this so-called “second victim” of a patient safety incident and aimed to examine: (1) experienced symptoms in the aftermath of a patient safety incident; (2) applied coping strategies; (3) the received versus needed support and (4) the aspects that influenced whether one becomes a second victim.
Materials and methodsThirty-one in-depth interviews were performed with physicians, nurses and midwives who have been involved in a patient safety incident.
ResultsThe symptoms were categorized under personal and professional impact. Both problem focused and emotion focused coping strategies were used in the aftermath of a PSI. Problem focused strategies such as performing a root cause analysis and the opportunity to learn from what happened were the most appreciated, but negative emotional responses such as repression and flight were common. Support from colleagues and supervisors who were involved in the same event, peer supporters or professional experts were the most needed. A few individuals described emotional support from the healthcare institution as unwanted. Rendered support was largely dependent on the organizational culture, a stigma remained among healthcare professionals to openly discuss patient safety incidents. Three aspects influenced the extent to which a healthcare professional became a second victim: personal, situational and organizational aspects.
ConclusionThese findings indicated that a multifactorial approach including individual and emotional support to second victims is crucial.
Cuando se produce un incidente adverso durante una intervención sanitaria, no solo puede sufrir el paciente, sino también el profesional sanitario implicado. Este estudio se centró en la conocida como «segunda víctima» de un incidente adverso durante una intervención y su objetivo fue evaluar: 1) los síntomas experimentados a raíz de un incidente adverso durante una intervención sanitaria; 2) las estrategias de afrontamiento que se aplicaron; 3) el apoyo recibido frente al apoyo necesario, y 4) los aspectos que influyeron en que uno se convirtiera en una segunda víctima.
Material y métodosSe llevaron a cabo 31 entrevistas exhaustivas con médicos, enfermeras y comadronas que habían estado involucrados en un incidente adverso durante una intervención.
ResultadosLos síntomas se clasificaron por repercusión personal y profesional. Se utilizaron estrategias de afrontamiento centradas en el problema y en la emoción después de un incidente adverso durante una intervención. Las estrategias centradas en el problema, como el análisis de la causa primordial y la oportunidad de aprender de lo sucedido, fueron las más apreciadas, pero las respuestas emocionales negativas, como represión y huida, eran frecuentes. Lo más necesitado era el apoyo de colegas y supervisores que participaron en la misma intervención, partidarios de los compañeros o expertos profesionales. Algunas personas describen el apoyo emocional de la institución sanitaria como no deseado. El apoyo prestado depende, en gran medida, de la cultura organizacional, aunque entre los profesionales sanitarios subsiste el estigma de hablar abiertamente de incidentes adversos durante una intervención. Tres aspectos influyeron en la medida en que un profesional sanitario se convirtió en una segunda víctima: aspectos personales, situacionales y organizacionales.
ConclusiónEstos resultados indicaron que es fundamental un enfoque multifactorial que incluya apoyo individual y emocional a la segunda víctima.
Reason said fallibility is part of the human condition.1 Because of the complexity of today's healthcare environment, it was recognized that even with preventive measures and the best healthcare professionals, they were all at risk of being involved in a patient safety incident (PSI) at some point.2 A PSI was “an event or circumstance that could have resulted, or did result, in unnecessary harm to a patient”.3 Despite all current efforts made to improve patient safety, harmful PSIs still occurred in one out of seven patients.4,5
Unfortunately, there was more than one victim after a PSI.6,7 The first victim was the patient and his/her family. The second victim after a PSI was the healthcare professional involved in the event. Scott et al.8 defined second victims as “healthcare professionals involved in an unanticipated adverse patient event or medical error who become victimized in the sense that they are traumatized by this event. Frequently, they feel personally responsible for the unexpected patient outcomes and feel as though they have failed their patient, doubting their clinical skills and knowledge base”. Several studies have reported signs and symptoms such as shame, guilt, anger, self-doubt and overall stress symptoms.9,10 Stress has been implicated as a major contributing factor to poor communication and poor leadership, a leading cause of sentinel events. It was estimated that nearly half of healthcare providers could experience the second victim phenomenon at least once during their professional career9,11 indicating this was a significant hazard in health care.
Clinician involvement in a PSI could affect both physical and psychological well-being and requires action to restore balance. Lazarus and Folkman12 described two types of coping responses as emotion focused and problem focused. Problem focused strategies aimed to remove or reduce the cause of the stressor. Emotion focused coping involved trying to reduce the negative emotional responses associated with stress such as embarrassment, fear, anxiety, depression, excitement and frustration. Healthcare professionals suffered when they did not have the chance to fully discuss incidents and express empathy through acknowledgement or apology to the patient and family. Open disclosure may help both the patient and the clinicians to deal with the consequences of an event.13
The most important factor to cope with a PSI is to receive support. Second victims can be further traumatized if their surroundings failed to provide offer the help that was needed.14 Understanding what other second victims had experienced could help the suffering healthcare professional to cope.15 The need for support was not limited to the person who committed an obvious error, but may be extended to other frontline healthcare staff.16 The post-incident trajectory for second victims could be to recover, to languish or to leave health care altogether.8 Scott et al.17 found that approximately 15% of second victims consider leaving their profession after a second victim experience.
Although there was a growing awareness that talking about PSIs was necessary to improve patient safety,7,18 it still remained taboo. To improve the quality of care and to sustain a culture of patient safety, there was a need to support healthcare clinicians who were suffering as second victims.19 Many healthcare professionals struggled to find support following a medical error and did not know where to find assistance or guidance. Healthcare institutions often failed to take responsibility for the provision of clinician support and provision of the necessary elements of a support system.7,20,21
In recent literature the impact on healthcare professionals after involvement in a PSI has been studied within single facilities.8,22–24 The objective of this study was to investigate the impact of PSIs on physicians, nurses and midwives from a multisite perspective. We focused on coping strategies, needed support and received support during one-on-one interviews. We also explored what aspects influenced when one becomes a second victim to a greater or smaller extent.
The following research questions were addressed in this study: (1) What symptoms are described by second victims in this study?, (2) How did second victims cope in the aftermath of the PSI?, (3) How were they supported and how was this appreciated? Which support did they need?, and (4) Which aspects influenced whether one becomes a second victim to a greater or smaller extent?
Materials and methodsStudy designIn-depth semi-structured interviews were conducted with physicians, midwives and nurses who were involved in a PSI during their working career. The interview guide was constructed based on the interview guide of Scott et al.8 and a review of the literature.9,19 It consisted of a general opening question concerning the respondents’ personal experience with a PSI (“Can you tell me what happened?”), followed by several probing questions regarding the used coping strategies, needed support, received support and how this was perceived by the clinician.
Setting and study sampleBecause of the sensitive nature of the subject of this research, a convenience sample was taken. A call for participation was launched via professional journals, lectures in hospitals and scientific associations. Candidates were asked to contact the researcher by e-mail or telephone. The researcher gave information about the study aim, the procedure and the measures that ensured privacy. Facilities were not specifically identified, neither were any patient or health professional data of individual facilities broken out in any reports or publications. Participants were included until saturation occurred.
Thirty-three interviews with nurses, midwives and physicians from different hospitals in Belgium were conducted. The inclusion criteria for the study included being a nurse, midwife or physician, having been involved in a PSI, voluntary participation, signing informed consent, currently working in a hospital and Dutch speaking. Exclusion criteria were having been involved in a legal case due to the PSI and indirect involvement in the PSI (team member). Due to these exclusion criteria, two interviews were excluded from the study. The study sample therefore consists of 31 interviews including 17 nurses, 3 midwives and 11 physicians from different hospitals in Belgium. The study sample contained 1 case that resulted in no harm for the patient, 9 cases resulted in temporary harm, 7 cases resulted in severe harm and 14 cases resulted in death of the patient.
Data collection procedure and analysisThe duration of an interview was between 45 and 90min and took place at a location of the participants’ choice. Participants were interviewed face-to-face by EVG. The interview was conducted in Dutch. It was audio-taped and field-notes were taken to maintain contextual details and non-verbal expressions. Data collection took place from June 2012 through January 2013. All interviews were transcribed verbatim. Interview recordings were saved by date and profession. Two researchers (EVG and DD) analysed the data independently. The data was processed with NVivo10, software for qualitative research.
Since it was impossible to neglect all the knowledge acquired from literature before starting the study, Bower25 referred to the use of sensitizing concepts for qualitative analysis. Sensitizing concepts were background ideas that inform the overall research problem and offer ways of seeing, organizing, and understanding the experience. They deepened perception and provided starting points for building analysis. The sensitizing concepts included in this study form the conceptual framework which linked various concepts and served as input for the formulation of theory.26 These concepts were derived from a thorough review of the literature and contain theoretical ideas that helped to set the context and direction of this study. Hence, the conceptual framework for this study included the following three sensitizing concepts which formed part of the analysis: (1) Emotional and professional impact, (2) emotion focused and problem focused coping strategies, and (3) three levels of support: informal, formal, and professional support.
Specific measurements were taken to avoid bias in this study. Bias by demand characteristics was avoided by clearly stating the aim of the study at the beginning of the interviews. Data collection bias and analysis bias was avoided by self-control and bracketing (with regards to being unprejudiced and actively seek for interview-faults) and peer debriefing within the research team.
Credibility of the study was achieved by the pursuit of data saturation, data triangulation (next to transcribed interviews, the field notes of the researcher were used to add relevant information) and peer evaluation (a team of experts in healthcare research, organizational psychology, coaching and qualitative research, had insight in the analytical process).
Ethics statementThe Ethics Committee of the University Hospitals KU Leuven granted approval for this study (ML8112). Written informed consent was obtained from all participants.
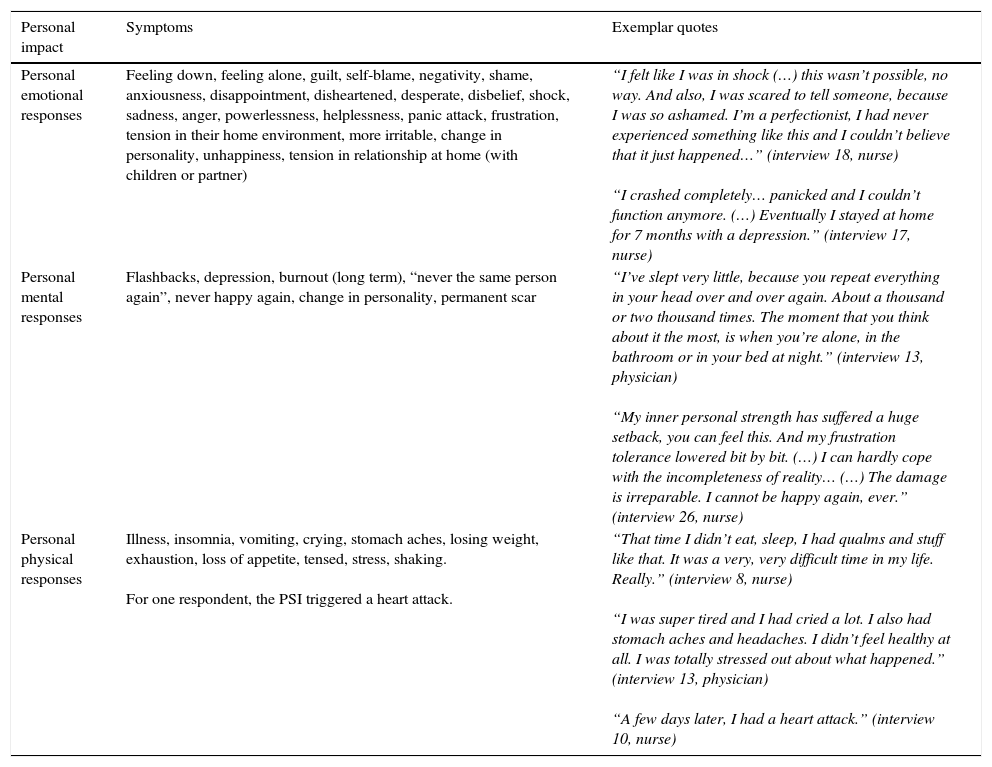
ResultsSymptoms after being involved in a patient safety incidentClinicians reported a personal impact as well as a professional impact. The personal symptoms are depicted in Table 1 and the professional impact in Table 2. Symptoms after being involved in a PSI were categorized into emotional, mental and physical responses.
Reported symptoms that have an effect on the personal life of the involved clinician.
| Personal impact | Symptoms | Exemplar quotes |
|---|---|---|
| Personal emotional responses | Feeling down, feeling alone, guilt, self-blame, negativity, shame, anxiousness, disappointment, disheartened, desperate, disbelief, shock, sadness, anger, powerlessness, helplessness, panic attack, frustration, tension in their home environment, more irritable, change in personality, unhappiness, tension in relationship at home (with children or partner) | “I felt like I was in shock (…) this wasn’t possible, no way. And also, I was scared to tell someone, because I was so ashamed. I’m a perfectionist, I had never experienced something like this and I couldn’t believe that it just happened…” (interview 18, nurse) “I crashed completely… panicked and I couldn’t function anymore. (…) Eventually I stayed at home for 7 months with a depression.” (interview 17, nurse) |
| Personal mental responses | Flashbacks, depression, burnout (long term), “never the same person again”, never happy again, change in personality, permanent scar | “I’ve slept very little, because you repeat everything in your head over and over again. About a thousand or two thousand times. The moment that you think about it the most, is when you’re alone, in the bathroom or in your bed at night.” (interview 13, physician) “My inner personal strength has suffered a huge setback, you can feel this. And my frustration tolerance lowered bit by bit. (…) I can hardly cope with the incompleteness of reality… (…) The damage is irreparable. I cannot be happy again, ever.” (interview 26, nurse) |
| Personal physical responses | Illness, insomnia, vomiting, crying, stomach aches, losing weight, exhaustion, loss of appetite, tensed, stress, shaking. For one respondent, the PSI triggered a heart attack. | “That time I didn’t eat, sleep, I had qualms and stuff like that. It was a very, very difficult time in my life. Really.” (interview 8, nurse) “I was super tired and I had cried a lot. I also had stomach aches and headaches. I didn’t feel healthy at all. I was totally stressed out about what happened.” (interview 13, physician) “A few days later, I had a heart attack.” (interview 10, nurse) |
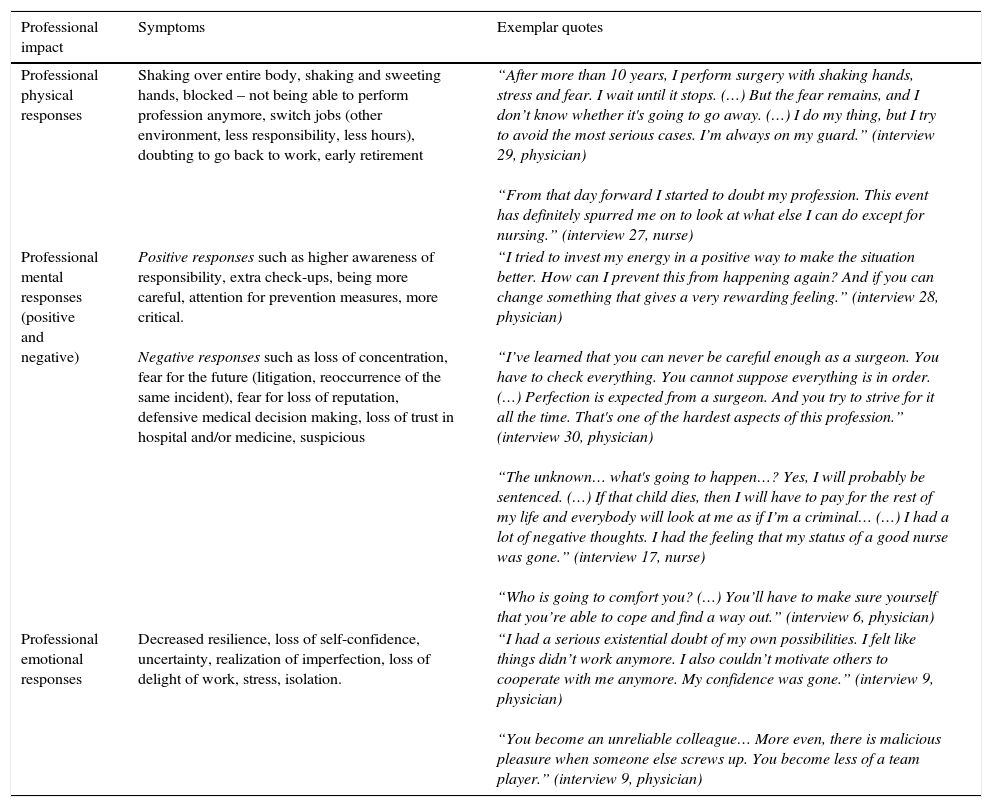
Reported symptoms that have an effect on the professional life of the involved clinician.
| Professional impact | Symptoms | Exemplar quotes |
|---|---|---|
| Professional physical responses | Shaking over entire body, shaking and sweeting hands, blocked – not being able to perform profession anymore, switch jobs (other environment, less responsibility, less hours), doubting to go back to work, early retirement | “After more than 10 years, I perform surgery with shaking hands, stress and fear. I wait until it stops. (…) But the fear remains, and I don’t know whether it's going to go away. (…) I do my thing, but I try to avoid the most serious cases. I’m always on my guard.” (interview 29, physician) “From that day forward I started to doubt my profession. This event has definitely spurred me on to look at what else I can do except for nursing.” (interview 27, nurse) |
| Professional mental responses (positive and negative) | Positive responses such as higher awareness of responsibility, extra check-ups, being more careful, attention for prevention measures, more critical. Negative responses such as loss of concentration, fear for the future (litigation, reoccurrence of the same incident), fear for loss of reputation, defensive medical decision making, loss of trust in hospital and/or medicine, suspicious | “I tried to invest my energy in a positive way to make the situation better. How can I prevent this from happening again? And if you can change something that gives a very rewarding feeling.” (interview 28, physician) “I’ve learned that you can never be careful enough as a surgeon. You have to check everything. You cannot suppose everything is in order. (…) Perfection is expected from a surgeon. And you try to strive for it all the time. That's one of the hardest aspects of this profession.” (interview 30, physician) “The unknown… what's going to happen…? Yes, I will probably be sentenced. (…) If that child dies, then I will have to pay for the rest of my life and everybody will look at me as if I’m a criminal… (…) I had a lot of negative thoughts. I had the feeling that my status of a good nurse was gone.” (interview 17, nurse) “Who is going to comfort you? (…) You’ll have to make sure yourself that you’re able to cope and find a way out.” (interview 6, physician) |
| Professional emotional responses | Decreased resilience, loss of self-confidence, uncertainty, realization of imperfection, loss of delight of work, stress, isolation. | “I had a serious existential doubt of my own possibilities. I felt like things didn’t work anymore. I also couldn’t motivate others to cooperate with me anymore. My confidence was gone.” (interview 9, physician) “You become an unreliable colleague… More even, there is malicious pleasure when someone else screws up. You become less of a team player.” (interview 9, physician) |
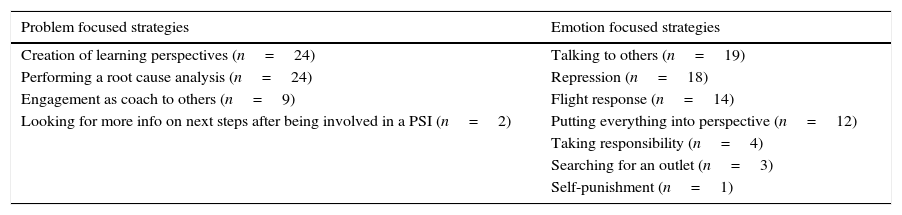
We identified four problem focused coping strategies and seven emotion focused coping strategies (see Table 3).
Problem focused and emotion focused coping strategies used by the second victims in this study.
| Problem focused strategies | Emotion focused strategies |
|---|---|
| Creation of learning perspectives (n=24) | Talking to others (n=19) |
| Performing a root cause analysis (n=24) | Repression (n=18) |
| Engagement as coach to others (n=9) | Flight response (n=14) |
| Looking for more info on next steps after being involved in a PSI (n=2) | Putting everything into perspective (n=12) |
| Taking responsibility (n=4) | |
| Searching for an outlet (n=3) | |
| Self-punishment (n=1) |
Many respondents tried to create a learning perspective. They wanted to learn from what happened, they were more critical and double-checked their work more often. Others became more of a perfectionist.
“I am very paranoid about delicate operations. I will triple check these. I’m not averse to asking a colleague – even if it is a younger or less experienced person – to check my calculations. I try to coach young colleagues to pay attention for patient safety” (Interview 2, nurse).
“It made me a stronger person. I’ve found a new drive to improve certain skills. I try to invest this new energy into positive things” (Interview 28, physician).
By performing a root cause analysis (RCA), second victims tried to found out what went wrong. They would write down what happened or look up additional information in the literature. Whenever it became clear that the PSI was the result of a system error, it provided some relief. In this manner responsibility was shared by the team.
“Putting everything together, writing down my part in this event, writing down the external factors which had an influence, what is the part of the patient in all this, whatever lies in ones power to change it or not,… It is the coincidence of so many factors that lead to the fatal incident. You have to be able to put this into perspective” (interview 22, nurse).
Some second victims engaged themselves as a ‘coach’ to others after the event. They wanted to share their experience, educate their colleagues about the event and the impact it had on their well-being. They want to make sure this would not happen to others.
“I wanted to avoid these things to happen again in the future. I immediately discussed the flaws and shortcomings within the system with the head midwife. I will look up more information and start a course for my colleagues” (interview 28, physician).
Many respondents expressed the urge to receive more information on the necessary steps after involvement in a PSI: Who had to be contacted, what paperwork needed to be completed. Many did not know what was going to happen next which caused additional stress. There was fear for a possible lawsuit, prosecution or even jail time.
“What helped me the most, was my wife. She is lawyer and has a totally different view on these things. She said to me: “If there is damage, it has to be compensated. You have insurance for that. So if something goes wrong, make sure your papers are in order and then you don’t have to worry anymore” (interview 9, physician).
“I didn’t know what the consequences were going to be. I started to imagine all kinds of things. I was like: what if I have to go to jail? Who's going to take care of my children?” (interview 15, midwife).
Emotion focused coping strategiesAn often used emotion focused coping strategy was talking to others. Talking about the event helped the healing process.
“I tried to cope by telling other people what happened, colleagues, students, friends and also at home” (interview 31, nurse).
Others coped by denying the entire event. They suppressed and held everything back. They immediately went back to work, acting as if nothing happened. These second victims took a hard line and posed as inaccessible, by which they did not allow any help. Suppression of feelings was very destructive. These second victims were often very much on their own and suspicious towards their colleagues’ judgements.
“I didn’t feel responsible enough for what happened. I kept myself busy with all the other patients. I took care of them, I took care of the other staff, but I didn’t take care of myself. (…) I’ve been running away” (interview 26, nurse).
“The hard thing was that I had to rely on the expertise and the judgement of my colleagues. But since the event it happened that I was doubtful about their judgement and I decided to send the patient for a second opinion in another hospital” (interview 30, physician).
Some second victims fled and distanced themselves, e.g. they avoided similar patients, changed wards, hospital or thought about leaving health care entirely.
“I was afraid to enter a patient room… You have to, but you don’t want to. Anyway, I changed wards. I really did want to work on that other ward, this was my way to flee from what happened” (interview 19, nurse).
“Afterwards I wanted to quit as a midwife. There was a job opening at a mortician, I applied for that job” (interview 15, midwife).
Some tried to cope with the aftermath of the event by putting it into perspective. Some were able to put everything into perspective by separating their work life from their private life.
“My work and my private life are totally separated. I can focus 100% on my job and put everything what happened at work aside when I’m at home. (…) I think if you take everything home, that you have no life anymore. You cannot stand still. Life goes on” (interview 10, nurse).
Some second victims were able to accept the situation by accepting responsibility for it.
“I apologized in the name of the entire group. By doing so, you take responsibility. I don’t mind taking responsibility and hereby acknowledging the error. To apologise, helps you to cope with your emotions” (interview 23, nurse).
Others looked for a way to reduce the stress and negative emotions. For example, gardening, take a moment's rest, or intensive exercise.
“Shortly after, I’ve put myself alone in the garden, which did good. Alone in the garden, thinking about nothing” (interview 32, nurse).
“I’m very sporty. So I went for a good run and I process it in the meantime.” (interview 23, nurse).
There was one second victim who took everything very personal and thought she deserved to be punished. A lawsuit would have been deserved.
“You can’t expect that the patient says “oh she made a minor error, that's okay”. No, the patient is allowed to be angry, allowed to react like that. The patient is allowed to file a lawsuit, although that's what I think? I think so” (interview 8, nurse).
How were they supported and how was this appreciated? Which support did they need?Who did they receive support from?The second victims in this study received support from various individuals. The support was not always appreciated. They received support from the home front, such as partners, friends, and family members. Many received support from colleagues that were not involved in the PSI or from colleagues who were. Some received professional support from psychologists or the ombudsman. Finally some received support from colleagues who were not involved in the event, but who had experienced a similar event.
Support from the home front was appreciated due to its non-judgemental nature or when family members have the same professional background. Support from the home front without a clinical background was not appreciated since “they have no knowledge of the way things work in health care”. Second victims were also limited in telling what happened since they are bound by laws of confidentiality.
“I could talk to my husband about it… However I’m bound by the law of confidentiality, so I could not tell him everything. It's also difficult for someone who doesn’t work in a hospital, to grasp the full impact of what happened” (interview 15, midwife).
“It was an advantage that I could talk to my friends who do not work in medicine, because then you can talk about other stuff. And then you don’t have to think about what happened anymore” (interview 33, physician).
Support was also received from colleagues who were not directly involved in the PSI, for instance supervisors, colleagues of the ward and management. This was perceived as helpful when these supporters wanted to be responsive and to reassure them. It was perceived as unhelpful when they were mostly just curious about what happened and not really interested in the second victim's well-being.
“A supervisor with whom I had a good connection with, looked at me and said “Are you okay?” And I was like “pfff, sure…” and I nodded a little bit. But then I felt tears coming up and I said “well, not so good…” and then she asked me what's going on and she took me outside for a while to talk. That helped” (interview 13, physician).
“I talked to colleagues about it, but they are looking at it more in a way of “oh yes, he should have done it this way or that way. Allow me to say, to be able to tell your story to them, is not easy. (…) It's more about what really happened and where it went wrong, instead of “how are you?” (interview 28, physician).
Support from colleagues directly involved in the same event was perceived both positive and negative. It was positive whenever these colleagues showed understanding and when they could go over the situation together to share responsibility. Since these colleagues were present during the PSI, they could perfectly empathize with what happened. By doing so the second victim felt less alone. However, it could also be perceived as negative support when colleagues directly involved in the event acted judgmental or were closed for discussion. In these cases, there was no opportunity to ventilate about emotions.
“The physician has had a long talk with me, about what happened, and how they were going to fix it. That helped a lot. (…) The explanation of the physician and also the support of the nurses who were there during the same shift, helped me the most. Just because they were present during the event” (interview 18, nurse).
“I haven’t received any support from the physician that was present at the time. This was really difficult for me. (…) I thought she looked at me as the person who committed the error. Then, afterwards, when I was home, I had a conversation with her, but that was very cool. (…) I don’t expect from everyone to be able to cope with this event, but I had expected more from the physician. I had expected more understanding” (interview 17, nurse).
Some second victims looked for professional support, such as psychologists, psychiatrists or the ombudsman. This professional help was much appreciated since it was personalized and objective. These professional supporters were empathic and would listen with an open, non-judgmental mind. For example, the help of the ombudsman was much appreciated since he mediated for contact with the first victim.
“My supervisor said to me “look, if you need to talk to someone, you can always contact this psychologist” (…) and so I did. And yes, this conversation was helpful. Also because she was a total objective person, who was used to coping with emotions” (interview 33, nurse).
“What helped me the most, was the ombudsman. It felt really good to have someone as a “buffer” between myself – who was responsible – and the patient. (…) He helped to communicate with one another” (interview 9, physician).
Some respondents also mentioned support from other second victims that were not involved in their case but had experienced similar clinical events. The support from colleagues who had been involved in another PSI and who were very open about this was truly appreciated. They were not only understanding but also non-judgmental.
“To know that you’re not the only one to whom this has happened before… Someone else has experienced a similar event and he is still here… Then you feel much more able to talk about it, because you know you this person will not judge you since he has experienced the same” (interview 1, midwife).
Received supportThe most received support in the aftermath of the event was primarily emotional support. The appreciation of support varied depending on the organizational safety culture.
Emotional support or psychological first aid was very personal and involved showing empathy, respect, listening, understanding, solidarity, appreciation or confirmation of the second victim's capacities. Those who had received minimal to no emotional support or psychological first aid, felt misunderstood and left alone with their grief. Their colleagues ignored what happened and what it meant to the persons involved. Those who did receive emotional support were able to ventilate and talk about what happened.
“There is no one in that time period that asked me “how are you?”. No, they looked at me as if I were the black sheep. I had to defend myself constantly and keep myself upright. I was on my own” (interview 24, physician).
“Some ask how you’re feeling. They want to know what they can do to help. And they comfort you too. I don’t know why, but it is comfortable when they tell you “your reaction is normal, this has happened to others as well”. (…) Then you feel less alone” (interview 13, physician).
Another important finding was that emotional support could be unwanted, especially when it was too soothing and unctuous. It did not help the second victims when individuals minimized the second victim's experience.
“Lots of colleagues told me “okay yes, everybody makes mistakes, don’t worry about it”. But I made a mistake which made a big difference for the patient. I appreciated them not pointing fingers at me, but I didn’t accept the fact that they minimized this kind of mistake and that the only thing they had to say is “everybody makes mistakes sometimes”(interview 20, nurse).
In some cases professional therapy was suggested. Those who accepted the offer, thought it was useful, but it could also be ‘too much’.
“Someone said to me “there is a special support team, maybe you should talk to someone of that team”. In the meanwhile I was already talking to my general practitioner and my psychotherapist. So I felt like, in the long run I will have about 101 therapists, and how will that help me….” (interview 17, nurse).
Information regarding the next steps in the aftermath of the PSI involved informational support on what has to be done by the healthcare organization in the form of an investigation. This included analysing what happened that caused the event. There was a need to understand and learn. For example, involvement in a root cause analysis was very much appreciated by the impacted clinician. When it became clear that in some cases the PSI was truly a complication, a mistake or a system error, instead of a medical error, this meant great relief. However in some cases, the involved healthcare professional was excluded from participation. This made everything more difficult to process. Many second victims would like to have offered recommendations to avoid similar events in the future.
“It is important to have a supervisor that listens to you and gives you advice, someone who takes initiative to analyse the event. So that the correct conclusions can be drawn and measures taken that it will never happen again. Instead of excluding the involved health professional, reach out to the person and organize a root cause analysis” (interview 2, nurse).
Help with legal or administrative tasks was appreciated. Although when this was the only kind of support they received, it was less valued.
“They asked immediately what they could do to help with administrative tasks. On this level they were very supportive, however on emotional level I did not receive any support that moment or later in time” (interview 7, nurse).
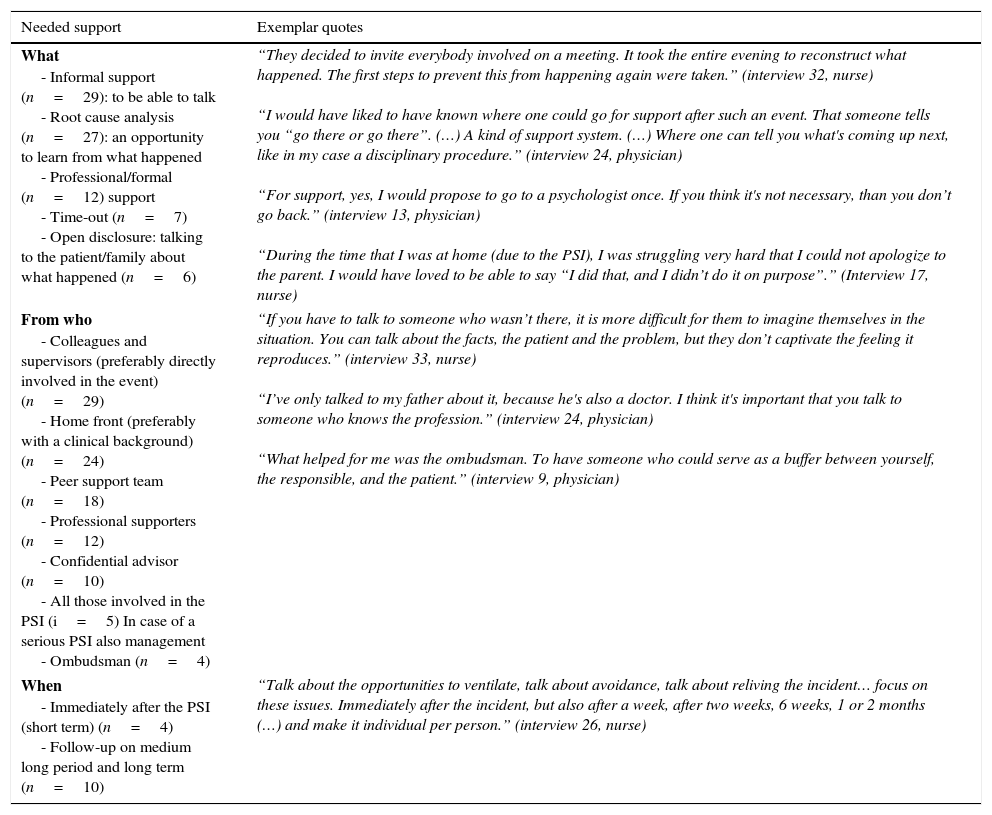
Which support did they need?Needed support after a PSI is demonstrated in Table 4. Several sources of support were mentioned: Informal support (just to be able to talk), performing a root cause analysis so that they have an opportunity to learn from what happened, more professional/formal support, the possibility for a time-out from work and the importance of open disclosure by informing the patient/family about what happened.
Needed Support according to the second victims in this study.
| Needed support | Exemplar quotes |
|---|---|
| What - Informal support (n=29): to be able to talk - Root cause analysis (n=27): an opportunity to learn from what happened - Professional/formal (n=12) support - Time-out (n=7) - Open disclosure: talking to the patient/family about what happened (n=6) | “They decided to invite everybody involved on a meeting. It took the entire evening to reconstruct what happened. The first steps to prevent this from happening again were taken.” (interview 32, nurse) “I would have liked to have known where one could go for support after such an event. That someone tells you “go there or go there”. (…) A kind of support system. (…) Where one can tell you what's coming up next, like in my case a disciplinary procedure.” (interview 24, physician) “For support, yes, I would propose to go to a psychologist once. If you think it's not necessary, than you don’t go back.” (interview 13, physician) “During the time that I was at home (due to the PSI), I was struggling very hard that I could not apologize to the parent. I would have loved to be able to say “I did that, and I didn’t do it on purpose”.” (Interview 17, nurse) |
| From who - Colleagues and supervisors (preferably directly involved in the event) (n=29) - Home front (preferably with a clinical background) (n=24) - Peer support team (n=18) - Professional supporters (n=12) - Confidential advisor (n=10) - All those involved in the PSI (i=5) In case of a serious PSI also management - Ombudsman (n=4) | “If you have to talk to someone who wasn’t there, it is more difficult for them to imagine themselves in the situation. You can talk about the facts, the patient and the problem, but they don’t captivate the feeling it reproduces.” (interview 33, nurse) “I’ve only talked to my father about it, because he's also a doctor. I think it's important that you talk to someone who knows the profession.” (interview 24, physician) “What helped for me was the ombudsman. To have someone who could serve as a buffer between yourself, the responsible, and the patient.” (interview 9, physician) |
| When - Immediately after the PSI (short term) (n=4) - Follow-up on medium long period and long term (n=10) | “Talk about the opportunities to ventilate, talk about avoidance, talk about reliving the incident… focus on these issues. Immediately after the incident, but also after a week, after two weeks, 6 weeks, 1 or 2 months (…) and make it individual per person.” (interview 26, nurse) |
When asked about preferred support services, informal support was most desired from colleagues, supervisors or the home front. In case of an open, just culture in the organization, the second victim preferred to talk to colleagues from within their own organization. When there was a culture of blame in the organization, respondents preferred to talk to people with the same medical background, however not from the same organization. Talking to a peer support team was mentioned as well as talking to professionals, such as psychologists or psychotherapists who have a neutral view on the incident and are capable of supporting the second victim emotionally. This need was only mentioned by those second victims who had experienced a serious impact after the PSI.
Because there was no time limit for recovering from an event, the time they needed emotional support was identified as short term as well as long term. Others declared that at one point you need closure.
The respondents within this study suggested that none of these support systems are possible if there is not an organizational patient safety culture. A ‘no blame-no shame’ culture was necessary to feel safe to discuss and learn from the clinical event.
There was also a need for education and training regarding the second victim experience, to increase awareness of the phenomenon. In many cases there wasn’t a possibility to talk about what happened, let alone the provision of emotional support. Supervisors and managers needed to ensure an empathic approach and receive training on provision of psychological first aid for clinicians suffering as second victims. This education and training should begin in college settings for everyone entering healthcare professions.10
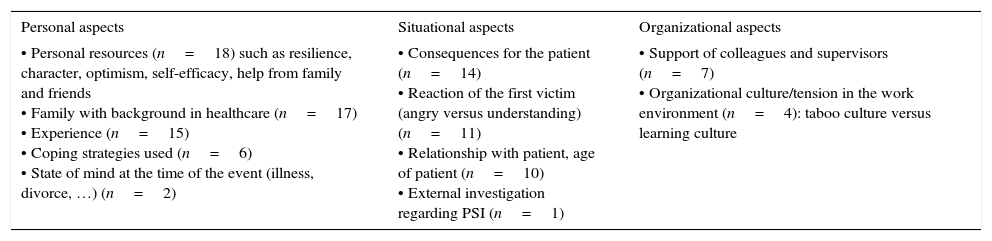
Which aspects determine whether one becomes a second victim to a greater or smaller extent?Not every respondent in this study experienced the same level of second victimhood. This is not a clear cut theme. Respondents emphasized aspects that determined the impact of involvement in a PSI: individual, situational and organizational aspects (see Table 5).
Aspects that influence whether a healthcare professional becomes a second victim to a greater or smaller extent.
| Personal aspects | Situational aspects | Organizational aspects |
|---|---|---|
| • Personal resources (n=18) such as resilience, character, optimism, self-efficacy, help from family and friends • Family with background in healthcare (n=17) • Experience (n=15) • Coping strategies used (n=6) • State of mind at the time of the event (illness, divorce, …) (n=2) | • Consequences for the patient (n=14) • Reaction of the first victim (angry versus understanding) (n=11) • Relationship with patient, age of patient (n=10) • External investigation regarding PSI (n=1) | • Support of colleagues and supervisors (n=7) • Organizational culture/tension in the work environment (n=4): taboo culture versus learning culture |
For individual aspects, it appeared that personal resources such as resilience, character, optimism, self-efficacy, and help from family and friends are important. Self-efficacy is the extent or strength of one's belief in one's own ability to complete tasks and reach goals. This characteristic trait helps determine how a second victim copes in the aftermath of an event.
“I have a stressful profession, but I can cope. (…) I mean, I experience some rough things, but I can place this in my life” (interview 28, physician).
Family members with healthcare backgrounds in healthcare helped in many cases, since they are able to understand what happened. Experience of the healthcare professional could work in both positive and negative ways. Because of their long experience they might be able to put everything into perspective, in other cases the event was the last straw.
“It's good that it happened to me, I have 30 years of experience, and that it didn’t happen to a student or someone who just started to work. Because if this happens to you as a student or starter, I think that's a reason to quit, yes” (interview 7, nurse).
Problem focused coping strategies seemed to be the most useful, since it lead to a learning perspective and constructive changes in practice. Another individual aspect that influenced the impact is the state of mind at the time of the event.
At the level of the incident itself (situational aspects), it appeared that the consequences for the patient, the reaction of the patient towards what happened, the relationship between the healthcare professional and the patient, and a possible external investigation played a significant role. Respondents in this study stated that the consequences for the patient determined for a great deal the impact on the healthcare professional. The more severe the patient's harm from the event, the more stressful the entire situation was for the involved clinician. On the other hand, review of the raw data and comparison of the symptoms, coping strategies, received and needed support between two groups of outcome for the first victims, namely death or no death, there was no considerable difference between the two groups.
“The patient didn’t die. (…) Otherwise this would have had an even bigger impact on me. This man is active again. After a few weeks, a month, two months, he recovered completely” (interview 11, physician).
The reaction of the first victim was a critical consideration. If they reacted in an understanding or angry manner, this greatly influenced the second victim response.
“When I went into the patient's room to take care of her, her husband pointed me outside again and said “I’m sorry, but I can‘t see your face anymore. Your face disgusts me” (interview 15, midwife).
Also the clinician relationship with the patient was important, whether they had cared for them for some time, whether they could relate or connect with them in age or situation (children, young parents), etc.
“I took care of her for 8 weeks. I remember washing her hair, even though it was a very busy shift. You try to do your best. (…) Yes, her death was very painful” (interview 25, nurse).
An external investigation by external bureau or police worsened the situation for the second victim. It increased anxiousness and nervousness and made coping more difficult.
“The police came by, several times. (…) I had to talk to them, show them everything. (…) And yes, that had an emotional impact on me” (interview 27, nurse).
At the organizational level it appeared that the overall patient safety culture was a deciding factor. In many cases the second victim did not feel safe to report nor ask for help. In some healthcare organizations there existed a culture of blame, which made it even more difficult. In this type of culture, colleagues reacted in negative ways by gossiping and belittling the second victim.
“Your environment victimizes you. Your colleagues create a mistrustful atmosphere and try to damage your reputation. (…) It ruins the atmosphere, so you actually become a bad colleague yourself, because you have the sense that they are telling things you cannot defend yourself against. (…) I had the feeling I was being singled out and that they’ve put me in a bad light” (interview 9, physician).
The possibility of open and transparent disclosure of the PSI to the first victim, made a great difference as well. Being open and honest created relief on the part of the suffering healthcare clinician.
“I wanted to contact the patient later on and tell her my version of the story, however I wasn’t allowed to. (…) It would have meant a great deal to me” (interview 15, midwife).
DiscussionImpactThe findings of this study confirm findings regarding emotional and professional impact in previous international literature.9,22,24 Regardless of culture or country of origin, these are normal human reactions to an abnormal situation. In some cases, a second victim could have continued emotional distress and develop posttraumatic stress.9,27 There are contradictions in literature as to whether the level of harm for the patients is in direct relation with the impact for the healthcare professional.14 This study illustrates that next to harm for the patient, other aspects also influenced the impact: such as individual, situational and organizational aspects.
CopingA theoretical model that helps to understand the impact of being involved in a PSI is the Job Demands-Resources Model by Bakker and Demerouti. This model proposes that job resources (such as supervisor and co-worker support, job content, etc.), as well as individual characteristics (e.g. self-efficacy), can buffer against the negative effect of work stressors28 such as a PSI. It illustrates that when an unexpected PSI occurs, the healthcare professional needs sufficient resources (such as informal and organizational support) at his disposal to help successfully cope with these events. Depending on the individual situation, using a certain coping strategy can lead to a positive or negative outcome for the involved clinician. Not every coping strategy is useful in every situation.29 In this study problem focused coping such as the creation of learning perspectives and performing a root cause analysis, seemed to be the most used coping strategy. Both coping strategies are suggested in literature as useful in helping second victim recovery.8 Negative emotional coping strategies such as repression and flight were also common.
SupportThe support needed after involvement in a PSI was being able to talk to someone (preferably someone also involved in the event), participate in an RCA, receive professional or formal peer support, a time-out and being able to share with the patient and/or his family. However support is a second step. The first step is being able to discuss event specifics and its impact on the clinician. In general, respondents were afraid to talk openly about PSIs. This taboo might hinder setting up appropriate support systems. In the study from Burlison et al.30 the importance of being able to talk to a respected peer, the possibility of a time-out and support from an organizational peer support team is confirmed. Results of this study regarding the need for support resembled the findings of Scott et al.17 It validated that support rendered at three levels of intensity are not only helpful but are desired by the second victim (informal support from colleagues, formal organizational support from a trained support team and professional counselling support).31 These three levels of support ensure that the wide range of support needs is covered.
An unexpected finding was that social support might not be desired by the clinician. Not every person benefitted from immediate supportive attention.32 Each event is a unique experience requiring other types of support. The point of support is to validate and enhance the voice of the second victim, not to smother it or take it over.14 The rendered support should be individualized based on the unique needs and desires of the suffering clinician.
When rendering support, attention must be paid to the different professional groups within health care. It was often said by the physician-respondents in this study, that they did not feel like current support systems are set up for them since “those support systems are for the nursing staff”. Physicians in many countries, such as Belgium, are self-employed not employees of a hospital and therefore do not truly feel connected to the hospital. From their capacity as independent healthcare workers in the hospitals, they too should be able to make use of organizational support systems.
DeterminantsThere are contradictions in literature on whether the outcome of the PSI for the patient is in direct relation with the impact for the healthcare professional.14 As a result, the authors investigated what aspects influence the gravity of the impact for the health professional.
Some respondents mentioned personal resources as being the most important factor to cope with the PSI. They referred to their resilience, hardiness, optimism and self-efficacy. They also mentioned their experience and state of mind at the time of the event. The respondents believed that due to their personal character they were able to put things aside and go on with their lives.33 Years of clinical experience in the field of health care worked in both ways. The event could have a great impact due to the health professional's limited experience. On the other hand, a ‘seasoned’ clinician with years of experience and cumulative clinical stressors may evoke a second victim response.
The clinician's state of mind at the time of the event also seems to be an important factor. Respondents feeling ill at the time of the event or were involved in personal issues at home, such as a divorce, felt more fragile. Participants described the impact of the PSI as being greater when personal stressors were present.
Next to the patient harm and personal characteristics of the healthcare professional, also situational aspects were relevant for the impact of a PSI. These included the reaction of the first victim (angry versus understanding), the relationship with the patient (have they cared for them before), the age of the patient (an event with an older patient was rated as less severe than with a child), and the possibility of an external investigation to further explore the case events seem to make it worse.14 Another aspect discussed in literature but excluded from this study, is involvement in a lawsuit due to the PSI. It is proven that litigation of the event can have a severe long-lasting impact on the clinician.34
The organizational patient safety culture was also mentioned to influence the impact of a PSI. Respondents often did not feel safe to discuss the PSI. They feared professional repercussions, legal liability, negative patient or family reactions and reputation loss.35 The appropriate ethical reaction consists of reporting the event and open disclosure, however if they fear disciplinary actions, this might feel like a no-win situation for the clinician. We must emphasize that an open, no blame-no shame culture is an important condition for this to be possible. The clinicians’ perception of psychological safety within the context of the work environment is important. Healthcare professionals need to discuss what transpired during care of the patient. Seeking support and discussing the emotional implications may represent a stigma of weakness.14 In some cases, the involved healthcare professional was directed not to talk about the event to the patient.36 Open disclosure and conversations with the first victim helps recovery for both parties after a PSI.37
Implications for practiceMany health professionals did not feel safe discussing a PSI in their respective hospitals. It is necessary to change a healthcare organization's culture of patient safety to increase transparency and post-event institutional learning before we can develop and implement organizational support systems for clinicians suffering as second victims.
The intensity of the impact may not be immediately obvious, not even to the second victim. The second victim's needs could therefore be mistaken, unless the organization can mobilize people with broader experience who can help interpret early or unclear signals.14 Every second victim reacts differently. Individualized support should be carefully coordinated, especially since for some clinicians social support is unwanted.
It is important to remember that every healthcare professional can become a second victim. And since health professionals in training are exposed to clinical practice they can become second victims as well.10 Colleges and universities preparing tomorrow's health professionals should be aware of this risk and need to incorporate second victim awareness into curriculums.
Second victims were very often interested in care processes that can be improved.14 They should be offered the opportunity to participate in improvement projects of care processes as someone with keen insights into the vulnerabilities of the existing processes.
Strengths and limits of the studyThis multisite study was not dependent on organizational culture. As this was a qualitative study, representativeness was not pursued. However saturation was obtained which indicates that major experiences and feelings of second victims are addressed. General patterns were identified among the different professions and outcomes of the PSIs. Most of the PSIs in this study were serious events (bias by extreme case sampling), however this is not a correct representation of reality. Events without harm to the patient are rarely reported. This can explain why less serious incidents were less mentioned in this study. On the other hand, it may be that a physician, nurse or midwife identifies oneself as a second victim more often, when the outcome for the patient was more serious.
Cases with judicial consequences were excluded from the study since we were looking for the ‘pure’ effect of a PSI on well-intending clinicians. Hu et al.34 state that (the risk of) litigation has an “additional” harmful effect on healthcare professionals.
Further research is needed to prevent healthcare professionals in becoming a second victim. More specifically, research is needed study the effectiveness of several support systems after being involved in a PSI. We should look at which aspects have the most influence on the impact. In addition, research is also needed to study the stressful impact of litigation on the clinician and most effective ways to offer support to minimize the impact.
Consequences of PSIs can be very severe for the involved healthcare professional. Second victims have the need to talk about what happened. Talking about PSIs however still remains difficult perhaps that is why the home front was identified as an important source of emotional support. The presence of transparent, no blame – no shame patient safety culture is a critical first step for recovery for the second victim. Each patient event should be evaluated individually, since not every second victim experiences the same response or impact especially since support may be unwelcome. The care for second victims after a PSI calls for a multifactorial and individual approach, both on the short and long term. Short term support includes emotional first aid from colleagues within a culture of support and respect. Long term support includes professional support or some time-off, so that follow-on patients are not put at an increased risk of a PSI themselves. Individual, situational and organizational aspects influence the impact of being involved in a PSI. Understanding what went wrong is of great importance, since the healthcare professional, the organization itself and other (future) patients will benefit from it.
FundingNone declared.
Conflicts of interestNone declared.
We hereby would like to acknowledge and thank all physicians, nurses and midwives willing to talk about their event and therefore contribute to this research.