We read the article by Rodriguez-Frías et al. 1 with interest. The authors reported a seroprevalence of anti-HEV antibodies (IgG anti-HEV) between 2.2% and 7% in Spain. However, the prevalence of anti-HEV antibodies varies according to the population included in the study, and is even much higher in HIV infected patients. Data on the frequency of anti-HEV antibodies in these patients in Spain are scarce, and it is a controversial issue in other countries, such as England where Feane et al.2 reported a similar seroprevalence in controls and patients with HIV infection.
Therefore, we tested 178 plasma samples from 178 HIV-infected patients who attended our Infectious Disease Department for monitoring of HAART therapy between December 2011 and January 2012. Among them, 140 (78.65%) were males with a mean age of 46 years (range: 20–78). IgG anti-HEV antibodies were detected in serum by a commercial enzyme immunoassay (EIA) kit (HEV Ab, DiaPro Diagnostic Bioprobes, Milan, Italy) following the manufacturer's instructions. All positive samples were studied further for the presence of IgM anti-HEV antibodies (HEV IgM, DiaPro Diagnostic Bioprobes, Milan, Italy). A result was considered positive by both tests when the ratio of the sample optical density and the cut-off value was higher than 2. Positive results by EIA were confirmed by Western blot analysis (RecomBlot HEV IgG/IgM; Mikrogen, Martinsried, Germany). In addition, HEV RNA was amplified by reverse transcriptase (RT)-nested PCR3 in all serum samples with IgG or IgM anti-HEV. All the patients included in this study were living in urban or the surrounding areas of Madrid. IgG anti-HEV antibodies were found in 18 out of 178 (10.11%). IgM anti-HEV antibodies were detected in 1 out of 18 IgG anti-HEV positive samples, suggesting acute or recent infection. HEV RNA was positive in a IgG anti-HEV positive patient. None of them presented clinical symptoms related to viral acute hepatitis currently or in recent years. ALT and AST were normal in all the patients who had IgG, IgM anti-HEV and/or HEV RNA in serum.
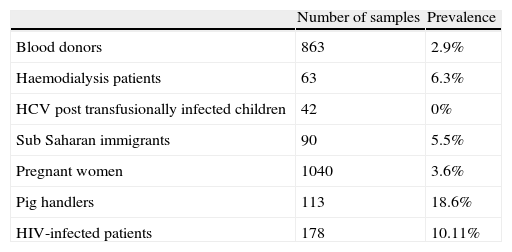
The seroprevalence of HEV infection has been studied in other probable risk groups, such as immigrants in Madrid4 (Table 1). Our results showed similar frequencies of detection of IgG anti-HEV antibodies in all the population tested, with the exception of pig handlers5 (18.6%) and HIV-infected patients (10.11%). In blood donors and pregnant women, the prevalence is 2.8% and 3.6%, respectively,6,7 significantly lower than in the HIV infected population, 10.11% (p<.01).
Prevalence of IgG anti-HEV among different groups of population in Spain according to Refs. 3–6.
| Number of samples | Prevalence | |
| Blood donors | 863 | 2.9% |
| Haemodialysis patients | 63 | 6.3% |
| HCV post transfusionally infected children | 42 | 0% |
| Sub Saharan immigrants | 90 | 5.5% |
| Pregnant women | 1040 | 3.6% |
| Pig handlers | 113 | 18.6% |
| HIV-infected patients | 178 | 10.11% |
Our data are similar to those reported by Jardi et al. in Catalonia,8 Spain. They found a prevalence of 9% among 238 HIV-infected patients. However, it is interesting that in healthy adults the prevalence is much higher in Catalonia9 than in Madrid,4 7% and 2.8%, respectively. This difference may be due to epidemiological characteristics of the patients studied (rural or urban areas, gender, age, profession), or methodology. The geographical situation of Madrid inside the country may also have a role, since a very high prevalence has been reported in southwest France.10
In summary, our results show a high seroprevalence of HEV infection in HIV positive patients different to that observed in blood donors, pregnant women, and other considered high risk groups (except pig handlers, as hepatitis E is a zoonosis and its reservoir is swine). The normal values of ALT and absence of clinical symptoms recorded in all the patients suggests that asymptomatic infection could have taken place frequently in the past in these patients, and they can be considered as a risk group for HEV infection.