A 63-year-old Hispanic woman with long-standing rheumatoid arthritis (RA) presented with one-month history of left shoulder pain and stiffness, fever, and a recently noted mass in the ipsilateral axillary fossa. She was being treated with methotrexate, hydroxychloroquine, sulfasalazine and nonsteroidal anti-inflammatory drugs (NSAIDS) for RA. The patient had no history of recent trauma, surgery or any intervention in the affected area. A painful, tender, ill-defined mass was noted during physical examination.
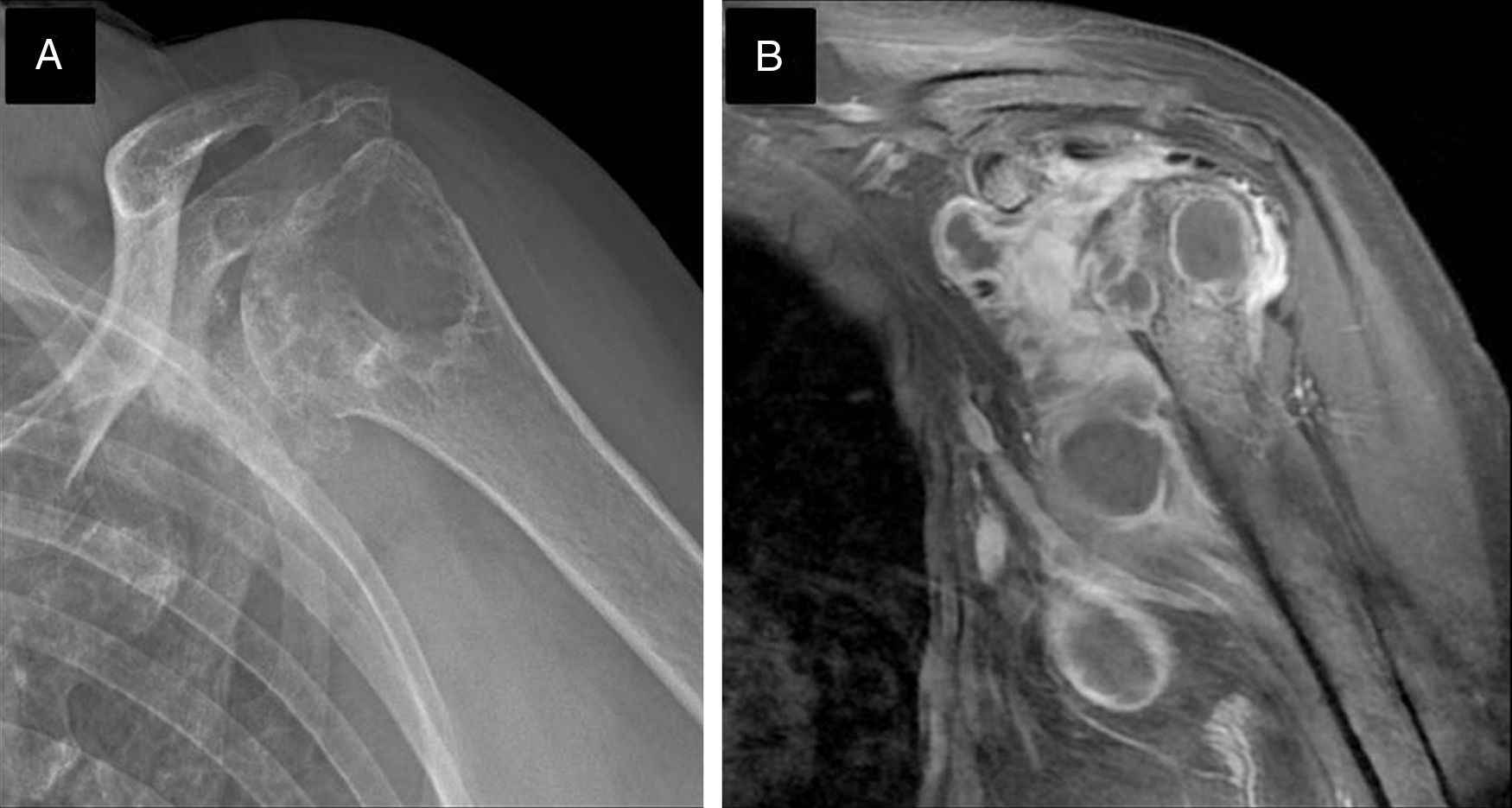
A shoulder X-ray (Fig. 1A) showed bone destruction, and magnetic resonance imaging with gadolinium enhancement (Fig. 1B), revealed a heterogeneous lesion, 12cm×7cm in size, associated to local destruction of the humeral head and multiple cold axillary abscesses.
Radiological features of osteoarticular infection of the left shoulder. (A) X-ray demonstrated articular erosive changes, osteopenia and a prominent humeral head cyst. (B) Coronal T1-weighted magnetic resonance images demonstrated profuse articular effusion, osteomyelitis and multiple abscesses in the axillary recess.
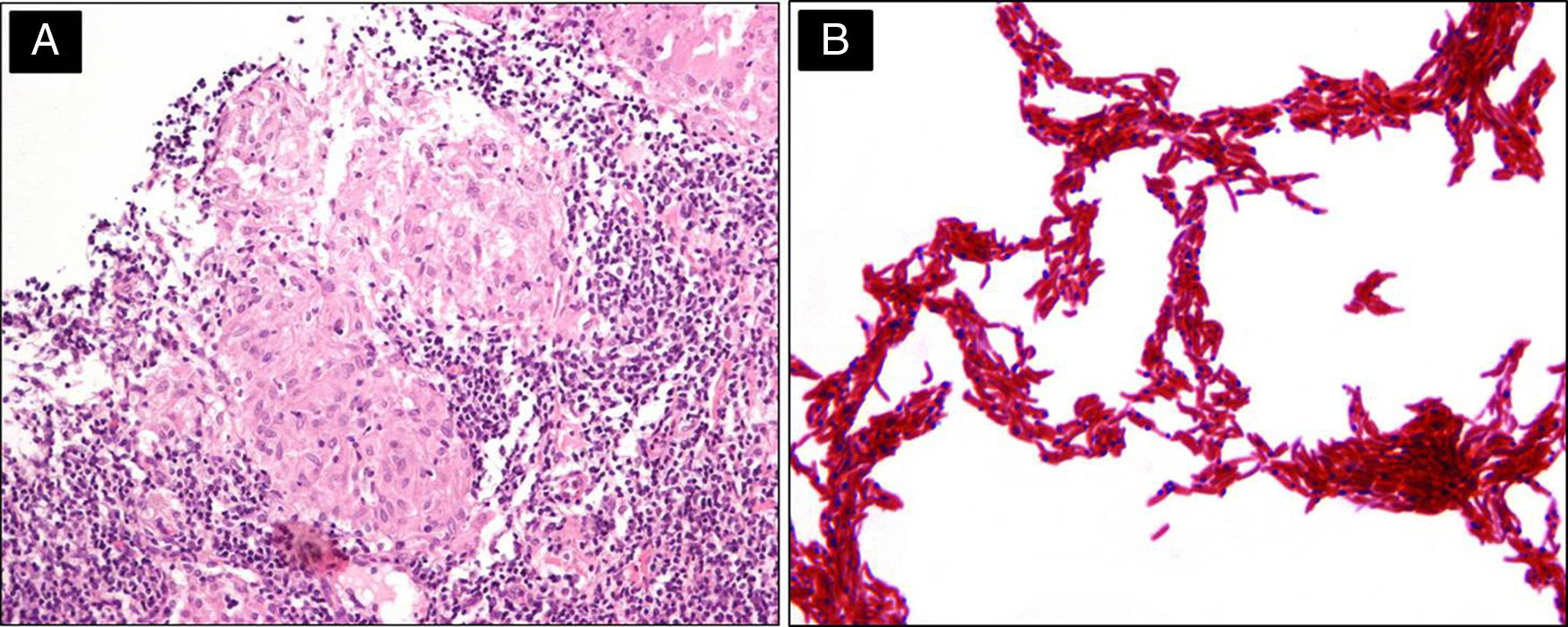
Tissue biopsy showed caseating granulomas (Fig. 2A). Abscess smear was positive for acid-fast bacilli. After 13 days, cultures were positive in MGIT (Mycobacteria Growth Indicator Tube) tubes and the culture smear revealed serpentine cords (Fig. 2B). Biochemical identification tests were conducted, and the mycobacteria were nitrate positive, niacin producing and pyrazinamidase test positive. This phenotypic pattern corresponded to Mycobacterium tuberculosis.
EvolutionThe patient was started on anti-TB treatment with isoniazid, rifampicin, ethambutol and pyrazinamide for 2 months, followed by isoniazid and rifampicin for an additional 10 months. Symptoms resolved and at last follow-up, 3 years after the biopsy, the patient was asymptomatic.
DiscussionWe report a patient with RA treated with multiple disease-modifying antirheumatic drugs (DMARDs) that developed a joint and bone infection with M. tuberculosis.
Mycobacterium is an uncommon pathogen causing acutely painful joints in adults. Approximately half of patients have an underlying comorbidity (diabetes mellitus, end-stage renal disease, autoimmune disease) leading to immune suppression and predisposition to the hematogenous spread of pathogens. Only a fifth of patients have a history of local injury. Histologically, caseating granulomatous inflammation is present in about two thirds of patients with MTB.1
One-third of the world's population is believed to harbor persistent or latent MTB infection, and 5–10% of these individuals develop the disease during their lifetime. There is a well-established association between RA and mycobacterial infection. It has been hypothesized that intrinsic characteristics of the disease such as abnormal T-cell regulation, antigen presenting dysfunction and the immunosuppressive effects of therapy, particularly the use of anti-TNF drugs and prednisone, predispose patients to these infections. In regions of low MTB prevalence and now, in the era of biologic therapy, the incidence rate of MTB infection is 5–20-fold greater with the use of anti-TNF therapy.2
The differential diagnoses in patients presenting with chronic mono-articular pain include shoulder impingement syndrome, chronic pyogenic osteomyelitis, Brodie's abscess and malignancies.3 Tuberculous osteomyelitis frequently appears as a “cold abscess”, with swelling, modest erythema or pain, and little or no local warmth.4
This case alerts clinicians to the possibility of mycobacterial infection particularly in susceptible hosts, even in the absence of obvious risk factors. The risk of infection challenges clinicians wishing to use immunosuppressive therapy, especially in this era of newer biologic and immunosuppressive drugs.
Conflicts of interestThe authors declare that there are no conflicts of interest.
The authors thanks to Bárbara Chávez Mazari, from the Laboratory of Clinical Microbiology for the biochemical identification of M. tuberculosis and image showing cord formation.