The COVID-19 pandemic led Spain to order a state of alert with the cessation of non-essential activities on 14 March 2020, and to implement public health interventions (such as home confinement) and other health recommendations to prevent the spread of the SARS-CoV-2 virus (hand washing and the obligation to wear face-masks). These factors could have influenced the rate of viral conjunctivitis.
MethodIn this retrospective, noninterventional, descriptive study, the incidence of viral conjunctivitis in an emergency department of a national hospital is compared over two distinct time periods: pre-COVID (13 March-30 September 2019, one year before the start of the pandemic) and COVID (13 March-30 September 2020).
ResultsIn the first period there were 436 cases of conjunctivitis, of which 168 (38.5%) were confirmed cases of viral conjunctivitis 168 (38.5%), while in the second period there were 121 recorded cases, of which the most frequent were allergic and traumatic (23 cases; 19% each group), bacterial (15 cases; 12.3%) and viral (15 cases; 12.3%). The diagnosis of viral conjunctivitis is the one that suffered the most significant relative reduction (48.5%), while other types of conjunctivitis hardly changed their relative frequency between these two periods of time.
ConclusionsViral conjunctivitis is the most frequent infectious disease of the eye and has a transmission rate similar to that of coronavirus, so the measures implemented could positively affect its incidence.
La pandemia COVID-19 condujo a España al decreto de estado de alarma con cese de actividades no esenciales el 14 de marzo de 2020 y a intervenciones de salud pública, como el confinamiento domiciliario y otras recomendaciones sanitarias para evitar la propagación del virus SARS-CoV-2: la higiene de manos y la obligatoriedad de portar mascarillas. Estos factores podrían haber influido en la tasa de conjuntivitis virales.
MétodoEn este estudio descriptivo retrospectivo no intervencionista se compara la incidencia de conjuntivitis virales en un servicio de urgencias de un hospital nacional sobre dos periodos de tiempo: pre-COVID (13 de marzo a 30 de septiembre de 2019, un año antes del inicio de la pandemia) y COVID (13 de marzo a 30 de septiembre de 2020).
ResultadosEn el primer periodo hubo 436 conjuntivitis, de las cuales 168 (38,5%) fueron casos confirmados de conjuntivitis viral 168 (38,5%), mientras que en el segundo periodo hubo 121 registros, de los cuales los más frecuentes fueron las conjuntivitis alérgicas y las traumáticas, con 23 casos (19% cada grupo); las conjuntivitis bacterianas, con 15 casos (12,3%), y las conjuntivitis virales, con 15 casos (12,3%). El diagnóstico de conjuntivitis viral es el que experimenta una reducción relativa más importante (48,5%), mientras que otros tipos de conjuntivitis apenas cambian su frecuencia relativa entre estos dos periodos de tiempo.
ConclusionesLa conjuntivitis viral, como patología infecciosa más frecuente del ojo, tiene una transmisión similar a la del coronavirus, por lo que las medidas implantadas podrían afectar positivamente a su incidencia.
In late December 2019, patients with viral pneumonia due to an unidentified microbial agent were reported in Wuhan, Hubei Province, Central China. This disease outbreak, called COVID-19, increased substantially and was declared a pandemic by the WHO on March 11, 20201. The causal microorganism is a type 2 coronavirus, a positive single-stranded RNA virus that originates the severe acute respiratory syndrome, SARS-CoV-2. Transmission pathways between humans is similar to that of other coronaviruses, through infected people's secretions; mainly respiratory droplets, hands or fomites contaminated with secretions, followed by contact to the mouth, nose or eyes' mucous membrane2.
After its arrival in Spain (estimated date, February 14, 2020), there was a significant COVID-19 progression that led to public health interventions. The state of emergency and closure of schools and non-essential activities was decreed on March 14, 2020 confining the population in their homes3. No previous public health intervention can compare to the magnitude of restriction established by this epidemic. Compulsory outdoors mask mandates and other recommendations such as social distancing and maintaining hand hygiene, washing them with water and soap or hydroalcoholic gel, were implemented. Reports show that this unusual situation in Spain could be associated with a strong decrease in both pediatric and adult infectious diseases, which are usually spread in social gatherings through respiratory and contact pathways. In this sense, a decrease in both incidence and prevalence of diseases such as bronchiolitis, common cold or seasonal flu processes during the epidemic has been published4,5. In addition, the decrease in the incidence of conjunctivitis associated to these processes or standalone has been observed, albeit empirically.
At ocular level, one of the most frequent infections is viral conjunctivitis (1% of all primary care visits and emergencies). Viral conjunctivitis is the most frequent cause of conjunctivitis, representing up to 80% of all cases. Most are caused by adenoviruses (especially subtypes 7, 11 and 18), and produce two of the clinical entities commonly associated to viral conjunctivitis: pharyngoconjunctivitis and epidemic keratoconjunctivitis6. Viral conjunctivitis can appear as an isolated disease or associated with systemic viral infections, such as upper respiratory tract infections (URTIs) and measles. Most infections are caused indirectly after respiratory inhalation, while the conjunctiva rarely serves as a virus entry point for the guest7, and in these cases local infection can be initiated through direct inoculation after ophthalmological procedures (tonometry and other ocular explorations), by contact with secretions of an infected patient, or in certain locations with higher viral concentration (for example, swimming pools)8. After an incubation period of 5–15 days, the patient exhibits red eyes, itching, burning, a foreign body sensation and often secretion and ocular discomfort that persist from 5 to 15 days7. Under slit lamp exploration, most patients have unilateral or bilateral acute follicular conjunctivitis, and unilateral cases frequently become bilateral a few days later. Preauricular lymphadenopathy might be present, and a history of URTIs is common. The symptomatic picture is usually acute and self-limiting, although very contagious. Treatment is merely a support and aimed at improving patient discomfort6. The most important element is infection spread prevention. To achieve this, doctors should wear gloves while examining infected patients and practice frequent and careful hand wash. Any equipment and instruments used during exploration must be cleaned with disinfectant solutions such as 10% sodium hypochlorite, hydrogen peroxide or alcohols such as 70% isopropyl alcohol9. Furthermore, patients and their families have to be instructed to act with caution at home, washing their hands often and keeping the patient's towels and bed sheets separated from the rest. Children must be kept out of schools from 5 to 7 days since the onset of symptoms.
In this work, the hypothesis of possible reduction of viral conjunctivitis cases in the national emergency system during the COVID-19 pandemic is considered, and attempts to relate this fact to the use of the hygienic-social measures mandated during the pandemic.
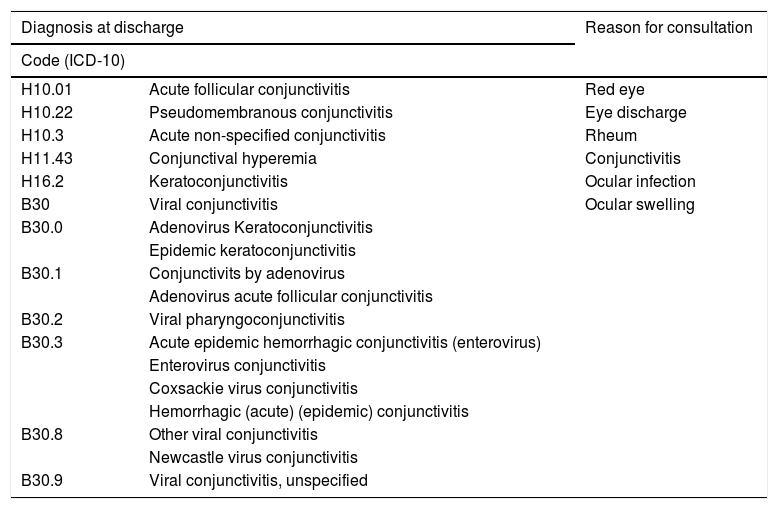
MethodsA retrospective, non-interventional descriptive study that compares the incidence of viral conjunctivitis in an emergency room service admission from a third-level Spanish hospital over two different periods of time: before COVID (March 13 to September 30, 2019, a year before the pandemic) and COVID (March 13 to September 30, 2020) is presented. A search on the hospital Electronic Clinical History Application (Hcis, DXC-HCIS®) within the emergency listings from both adults and children, including diagnoses (ICD-10)10 generally used in clinical trials to describe this pathology (Table 1) by the emergency ophthalmologist, in both written and coded diagnostic boxes was performed.
Most used diagnoses in the study to describe acute viral conjunctivitis according to the International Catalog of Diseases Version 10 (ICD-10)10.
| Diagnosis at discharge | Reason for consultation | |
|---|---|---|
| Code (ICD-10) | ||
| H10.01 | Acute follicular conjunctivitis | Red eye |
| H10.22 | Pseudomembranous conjunctivitis | Eye discharge |
| H10.3 | Acute non-specified conjunctivitis | Rheum |
| H11.43 | Conjunctival hyperemia | Conjunctivitis |
| H16.2 | Keratoconjunctivitis | Ocular infection |
| B30 | Viral conjunctivitis | Ocular swelling |
| B30.0 | Adenovirus Keratoconjunctivitis | |
| Epidemic keratoconjunctivitis | ||
| B30.1 | Conjunctivits by adenovirus | |
| Adenovirus acute follicular conjunctivitis | ||
| B30.2 | Viral pharyngoconjunctivitis | |
| B30.3 | Acute epidemic hemorrhagic conjunctivitis (enterovirus) | |
| Enterovirus conjunctivitis | ||
| Coxsackie virus conjunctivitis | ||
| Hemorrhagic (acute) (epidemic) conjunctivitis | ||
| B30.8 | Other viral conjunctivitis | |
| Newcastle virus conjunctivitis | ||
| B30.9 | Viral conjunctivitis, unspecified | |
As a result, two spreadsheets were obtained (Microsoft Office Excel® 2007), one corresponding to the 13/03-30/09/2019 period and another corresponding to the 13/03-30/09/2020 period, generated by the program and called Excel diagnóstico 2019 and Excel diagnóstico 2020, that contained the clinical history number, patient name, date of birth, age, emergency room admission date and diagnosis.
To avoid the loss of cases without ICD-10 diagnosis by this system, a decision to expand the search within these emergency listings also selecting reason for consultation was made (which is found in 100% of patients, since it is mandatory data for Manchester staging and subsequent filtering for the emergency specialist). As reasons for consultation, the most frequently used by the triaging emergency staff were chosen: red eye, ocular secretion, rheum, conjunctivitis, ocular infection and ocular swelling. Two other new Excel® sheets generated by the program were obtained, called Excel motivo de consulta 2019 and Excel motivo de consulta 2020 that contained the same basic data. The two spreadsheets of each year were merged in a third Excel sheet called Excel fusión (one for 2019 and another for 2020). A total of 436 conjunctivitis records were obtained for the 2019 analyzed period (before COVID) and 121 records for the 2020 analyzed period (COVID).
In this study, no samples of conjunctival exudate or serology were collected for the determination of causal microbiological diagnosis. Diagnosis was based on anamnesis, the epidemiological survey, regional lymph nodes exploration by palpation and slit lamp ocular exploration of both eyes with anesthetic eye drops and fluorescein instillation performed by the emergency ophthalmologist.
ResultsThe first analysis was carried out with the 436 before COVID period records and the 121 COVID period records.
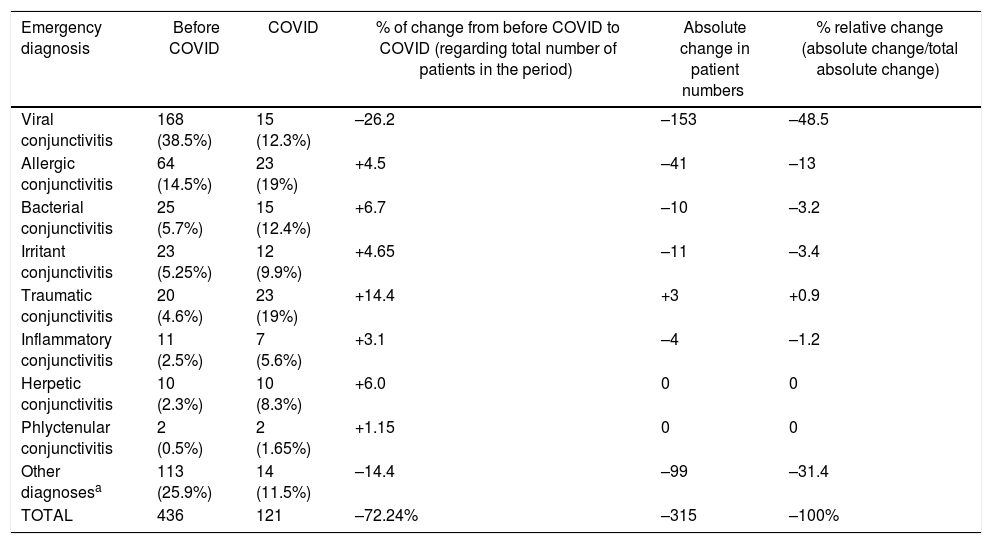
Out of the 436 before COVID period conjunctivitis records, 168 (38.5%) remained as confirmed cases of viral conjunctivitis, the second most frequent type being allergic with 64 cases (14.5%), bacterial with 25 cases ( 5.7%), irritant with 23 cases (5.25%), traumatic with 20 cases (4.6%), inflammatory with 11 cases (2.5%), herpetic with 10 cases (2, 3%) and phlyctenular with 2 cases (0.5%); the rest were diagnostic errors (subconjunctival bleeding, uveitis, keratitis, etc.) (Table 2).
Most frequently diagnosed conjunctivitis in emergencies (prior to ICD-10 coding) in the period before COVID (March 13 to September 30, 2019) and during COVID (March 13, 2020 to September 30, 2020).
| Emergency diagnosis | Before COVID | COVID | % of change from before COVID to COVID (regarding total number of patients in the period) | Absolute change in patient numbers | % relative change (absolute change/total absolute change) |
|---|---|---|---|---|---|
| Viral conjunctivitis | 168 (38.5%) | 15 (12.3%) | –26.2 | –153 | –48.5 |
| Allergic conjunctivitis | 64 (14.5%) | 23 (19%) | +4.5 | –41 | –13 |
| Bacterial conjunctivitis | 25 (5.7%) | 15 (12.4%) | +6.7 | –10 | –3.2 |
| Irritant conjunctivitis | 23 (5.25%) | 12 (9.9%) | +4.65 | –11 | –3.4 |
| Traumatic conjunctivitis | 20 (4.6%) | 23 (19%) | +14.4 | +3 | +0.9 |
| Inflammatory conjunctivitis | 11 (2.5%) | 7 (5.6%) | +3.1 | –4 | –1.2 |
| Herpetic conjunctivitis | 10 (2.3%) | 10 (8.3%) | +6.0 | 0 | 0 |
| Phlyctenular conjunctivitis | 2 (0.5%) | 2 (1.65%) | +1.15 | 0 | 0 |
| Other diagnosesa | 113 (25.9%) | 14 (11.5%) | –14.4 | –99 | –31.4 |
| TOTAL | 436 | 121 | –72.24% | –315 | –100% |
In the 121 COVID period conjunctivitis records, the most frequent types were allergic and traumatic with 23 cases in each group (19%), viral and bacterial with 15 cases (12.3% each), irritant with 12 cases (9.9%), herpetic with 10 cases (8.3%), inflammatory with 7 cases (5.8%) and phlyctenular with 2 cases (1.65%); the rest were diagnostic errors. It should be noted that out of the 121 cases of conjunctivitis, 4 of them were confirmed cases of COVID-19, but only one of them manifested acute follicular conjunctivitis; the remaining 3 cases did not manifest follicles and could not be confirmed viral conjunctivitis (Table 2).
If the worldwide emergency activity of the year 2020 compared to 2019 is estimated based on these data, the number of ophthalmology emergency consultations suffered a drop from 2019 to 2020 of 72.24%, which affected all diagnoses, i.e., the number of patients with a viral, allergic, etc. conjunctivitis diagnosis, was theoretically decreased by 72.24% due to home confinement and other pandemic-related effects. However, viral conjunctivitis diagnosis is the type that experiences the greatest drop in absolute numbers of all possible conjunctivitis diagnoses during the analyzed COVID period (153 less cases than the previous year), the second diagnosis in numerical decrease being allergic conjunctivitis (41 less cases in 2020 compared to 2019). If this absolute numerical value is relativized in relation to the global decrease in ophthalmological visits in emergency care numbers (315 less patients attended in 2020 compared to 2019) the diagnosis with the most important percentage drop remains viral conjunctivitis, with 48.5% less emergency consultations. In second place, other diagnostic errors cataloged as conjunctivitis in a first screen is observed, with 31.4% less prevalence, and in third place allergic conjunctivitis, with a 13% less.
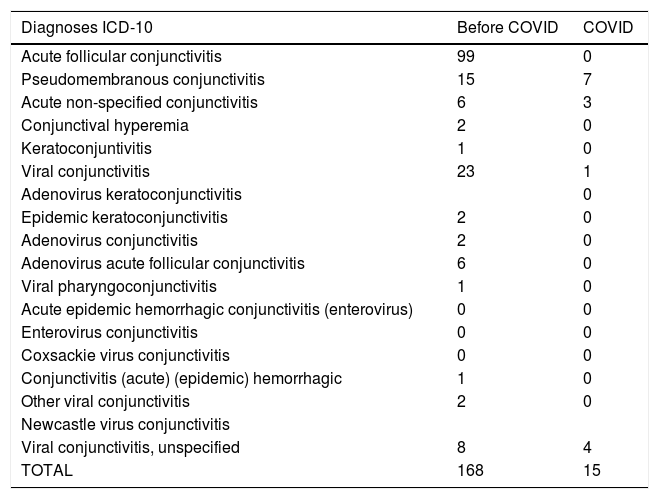
To avoid the influence of diagnostic errors mistaken with conjunctivitis (which constitute up to 25.9% of Excel fusión 2019 and 11.5% of Excel fusión 2020), a second screen of the spreadsheets was performed, so that in all cases obtained by searching reason for consultation, the final diagnoses given to the patient by the ophthalmologist were all confirmed one by one (which was written in the free text space of the emergency discharge report in the clinical history itself but it did not appear in the written diagnostic boxes as a coded diagnosis), and if they did not correspond to any of those selected from the ICD-10 code, were deleted. After also eliminating duplicate patients, files that had basic information missing or incongruous diagnoses, a total of 168 viral conjunctivitis patient records were obtained for the period 13/03-30/09/19 (Excel fusión 2019 final, before COVID period) and a total of 15 viral conjunctivitis patient records the period 13/03-30/09/20 (Excel fusión 2020 final, COVID period) These two new spreadsheets only include diagnoses compatible with ICD-10 for viral conjunctivitis diagnosis (Table 1). The patient distribution by diagnosis is shown in Table 3.
Number of final patients attributed to each ICD-10 diagnosis for viral conjunctivitis in each time period analyzed: period before COVID (March 13 to September 30, 2019) and COVID period (March 13, 2020 to 30 September, 2020), after clearing the initially obtained spreadsheets.
| Diagnoses ICD-10 | Before COVID | COVID |
|---|---|---|
| Acute follicular conjunctivitis | 99 | 0 |
| Pseudomembranous conjunctivitis | 15 | 7 |
| Acute non-specified conjunctivitis | 6 | 3 |
| Conjunctival hyperemia | 2 | 0 |
| Keratoconjuntivitis | 1 | 0 |
| Viral conjunctivitis | 23 | 1 |
| Adenovirus keratoconjunctivitis | 0 | |
| Epidemic keratoconjunctivitis | 2 | 0 |
| Adenovirus conjunctivitis | 2 | 0 |
| Adenovirus acute follicular conjunctivitis | 6 | 0 |
| Viral pharyngoconjunctivitis | 1 | 0 |
| Acute epidemic hemorrhagic conjunctivitis (enterovirus) | 0 | 0 |
| Enterovirus conjunctivitis | 0 | 0 |
| Coxsackie virus conjunctivitis | 0 | 0 |
| Conjunctivitis (acute) (epidemic) hemorrhagic | 1 | 0 |
| Other viral conjunctivitis | 2 | 0 |
| Newcastle virus conjunctivitis | ||
| Viral conjunctivitis, unspecified | 8 | 4 |
| TOTAL | 168 | 15 |
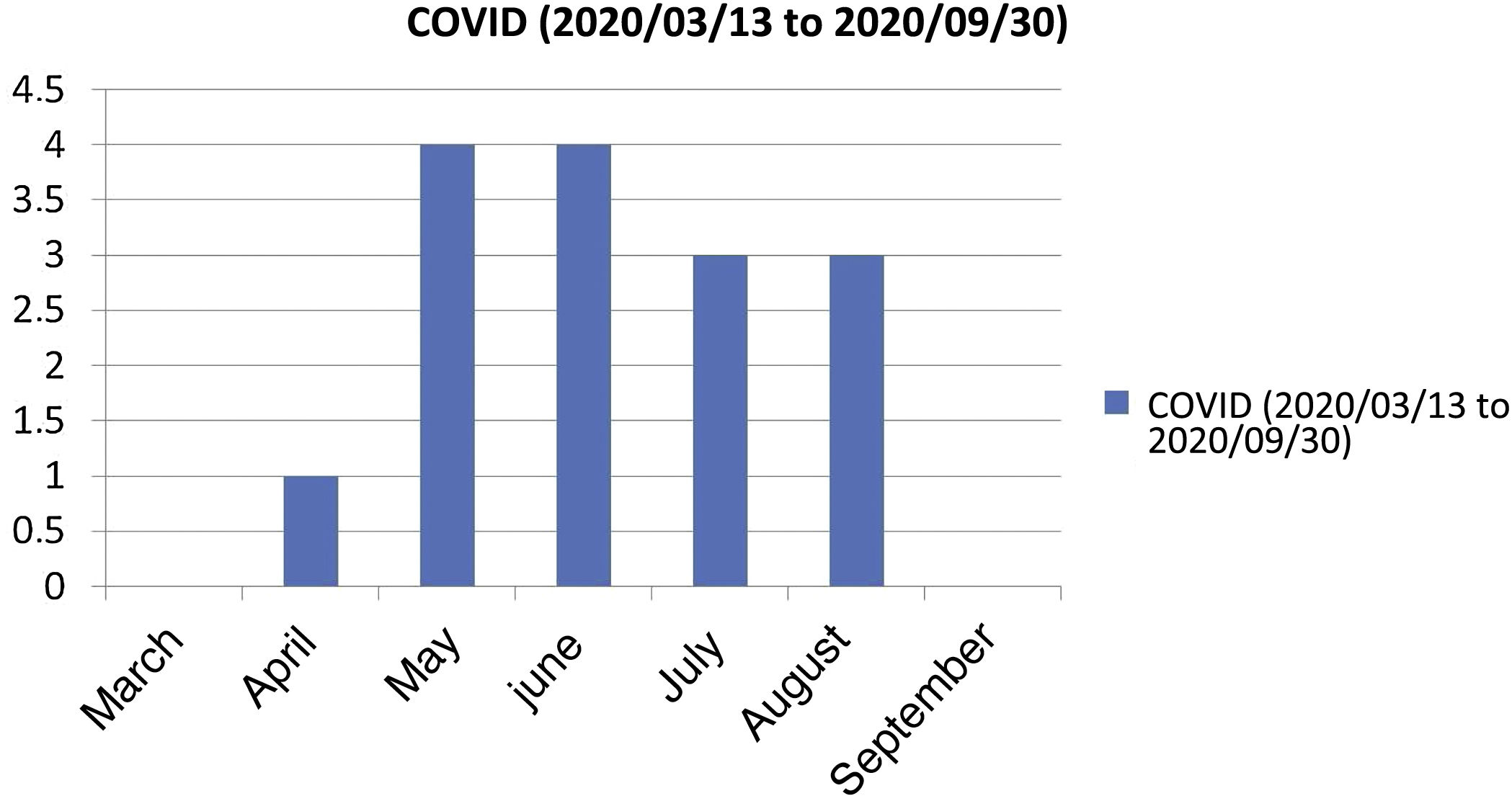
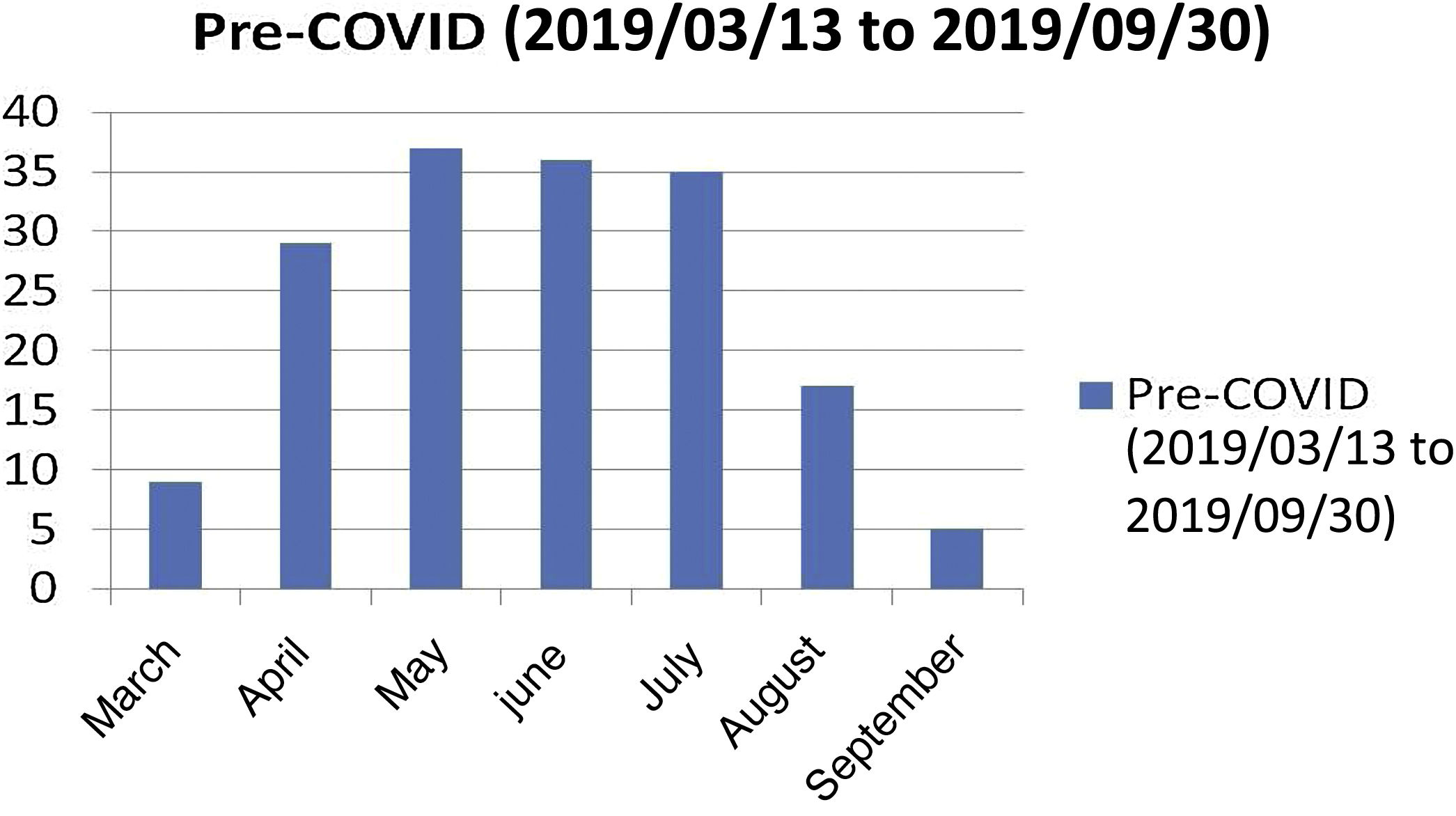
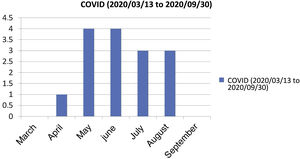
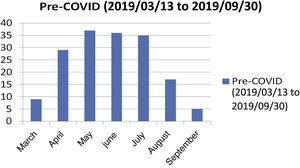
This second analysis shows that during the 6-month period between 13/03/2020 (COVID-19 pandemic became official) up to the data collection closure date on 09/30/2020, 15 diagnoses compatible with ICD-10 standards for viral conjunctivitis, without no cases registered during the months of March or September 2020, and with a maximum number of patients per month in the months of May and June (the distribution of diagnosed viral conjunctivitis cases per month in each period is shown in Figs. 1 and 2). This contrasts significantly with the number of diagnosed and collected cases in the same time frame from the previous year (13/03-30/09/2019), in which the average number of patients diagnosed with viral conjunctivitis was 26.5 patients (not taking the month of March into account, since it is not a complete month and therefore the average cannot be performed).
The only case of viral conjunctivitis that complied with ICD-10 diagnostic criteria and microbiologically confirmed as positive for SARS-CoV-2 was a pseudomembranous unilateral conjunctivitis that presented follicles in ophthalmological exploration, diagnosed in May 2020.
DiscussionDuring the COVID-19 pandemic in Spain and mainly motivated by the state of emergency declaration, a restriction on personal and collective circulation was enforced in the population, limited to carrying out exclusively first necessity activities, such as attending health centers or assisting vulnerable people. Transportation, both public and private, was reduced by at least half, and cultural, artistic, sports and similar activities were suspended. All of this, added to the “fear” of contracting the COVID-19 disease, limited patients visits to the emergency services of health centers and hospitals throughout Spain. This explains the decrease of patients treated in emergencies in all medical specialties, including ophthalmology. Although the data is estimated, in an ophthalmological center similar to that of our study, patient care in the emergency room decreased more than 70% in 2020 compared to 2019.
Out of all ophthalmological pathologies, this work analyzed one of the most frequent reasons for consultation, conjunctivitis7, and viral conjunctivitis in particular, which at the time of year analyzed (March to September) are the most common, since its frequency is higher in spring and summer6. The viruses that cause this pathology most frequently, adenoviruses, share transmission mechanisms and even clinical signs very similar to those of coronavirus11, and therefore it can be assumed that measures applied to contain the spread during the COVID-1912,13 pandemic and the preventing recommendations from various medical organizations and ophthalmological societies14–18 have also an effect in decreasing viral conjunctivitis propagation. Despite the obvious case decrease due to the emergency state and home confinement, after performing a careful data analysis it can be concluded that from all the types of conjunctivitis admitted in emergency care, viral conjunctivitis experienced the biggest decrease. According to the relative percentage of change analysis (absolute change or difference in total number of patients diagnosed with conjunctivitis of a given type, for example viral, in the period of 2020 relative to the period of 2019 and divided by the absolute change total or difference in number of all conjunctivitis diagnoses in the period of 2020 compared to 2019), viral conjunctivitis decreases by 48.5% in 2020 in contrast to 2019, far from the second type, allergic conjunctivitis, that only decreased 13%. In absolute values, the number of patients attended with a final viral conjunctivitis diagnosis was reduced by 91% (only 15 cases in 2020 compared to 168 in 2019), while the number of patients with allergic conjunctivitis remains 64% of cases (23 cases in 2020 compared to 64 in 2019). Other conjunctivitis diagnoses do not present as much variation between these two time intervals.
The reasons that could explain this marked decrease in viral conjunctivitis compared to other types of conjunctivitis may be in the hygiene measures implemented as a result of the pandemic, which have affected the transmission pathway of SARS-CoV-2 and other respiratory viruses (like the adenovirus that causes most viral conjunctivitis). Among these measures, use of facial masks, washing hands, ventilation of spaces with high concentration of people and surface disinfection with diluted bleach, chlorine or alcohol derivatives at 70% (which have also shown to be effective against adenoviruses19,20).
This study would be the first to demonstrate the benefits of the hygienic-social measures implemented during the pandemic for the prevention of community propagation of viral conjunctivitis.
Our study has limitations, since cases of conjunctivitis whose patients have not attended the emergency department but have gone to other health centers or cases where the patients simply decided to stay at home have not been collected in this study. Despite this, it can be acknowledged that the case loss percentage would affect all types of conjunctivitis and not just viral types. Another limitation would be the lack of microbiological confirmation of conjunctivitis diagnoses, although it is not usually necessary, being an ophthalmological clinical diagnosis.
ConclusionsDuring the COVID-19 pandemic (a period of 6 months has been analyzed since the beginning of the pandemic in Spain, on March 13th 2020) a decrease in conjunctivitis incidence has been observed in comparison to the same period of the previous year, and more notably in viral type conjunctivitis incidence, in relation to other red eye diagnoses made in the emergency service from a third-level Spanish national hospital. This finding is related to the implementation of hygiene-social measures imposed in the emergency state and recommended by multiple health organizations.
FundingThis work has not received funding from public or private institutions.
Conflict of interestNo conflicts of interests have been declared by the authors.
Please cite this article as: Conde Bachiller Y, Puente Gete B, Gil Ibáñez L, Esquivel Benito G, Asencio Duran M, Dabad Moreno JV. Pandemia COVID-19: impacto sobre la tasa de conjuntivitis virales. Arch Soc Esp Oftalmol. 2022;97:63–69.