Describe the assistance provided to asthmatic patients by Primary Care Paediatricians (PCP) in Spain and the material and human resources available for diagnosis and follow-up.
MethodsA cross-sectional descriptive study using an on-line survey, sent to PCP regarding the availability of diagnostic resources, carrying out programmed and educational activities, collaboration of nursing staff and their relationship with existing institutional plans to care for children with asthma. A latent class model (LCM) was used to describe the differences among paediatricians based on the variables studied.
ResultsOf the 708 answers, 675 were considered valid; 76% of the paediatricians had a spirometer, 75% specific IgE, 17% prick-test, 95% had placebo inhalers and 97% inhalation chambers. 57% performed programmed activities with their patients, while 56% shared their care of asthmatic patients with their nursing staff, but only 25% of the nurses were involved in the follow-up and 12% in education. LCM identified four patterns. The two groups with greater access to diagnostic resources counted on institutional plans/guidelines. However, the only variable differentiating the groups with more programmed and educational activities was the participation of nurses.
ConclusionsThe availability of asthma plans/guidelines and resources for diagnosis and follow-up is not sufficient to improve important aspects of primary care for children with asthma. Organisational changes are necessary to include programmed asthma-related visits and paediatric teams with greater involvement of the nurses when caring for these patients.
Asthma is the most frequent chronic disease throughout childhood. In Spain, it affects 10% of the infant population, with variations depending on geographic location.1
As a public health problem, asthma impacts both on the patients’ and their families’ quality of life; it leads to absenteeism at school and work, in addition to a high consumption of resources. In Spain, the estimated cost of asthma in children under the age of 16 was 532 million Euros/year. Of this, 40% is attributed to indirect costs (caregiver hours) and 60% to direct or healthcare costs (medical care, hospitalisation, diagnostic tests, treatment and transportation).2
National asthma guidelines have been created, especially in countries where it is a prevailing condition.3,4 Spain is a country with intermediate asthma prevalence, but until recently there was no national plan to guide a comprehensive approach to patients. Healthcare in Spain is easily accessible but is the responsibility of each individual region (called Autonomous Community). Some regional health services had previously developed their own plans/guidelines for the care of children and adolescents with asthma.5 Since 2003, a guideline of national scope has been developed6 and updated,7 following GINA4 recommendations, with the participation of all scientific societies in which asthma is the common field of interest. A specific guide on childhood asthma has also been published.8 It is expected that this will decrease variability in the clinical practice and standardise the criteria to better diagnose and control the disease.
Plans differ from guidelines in that they incorporate a definition of resources, both material and human, that are required for the health care provision following guidelines recommendations. So, as asthma guidelines recommend spirometry be performed on collaborating asthmatic children for both diagnostic and follow-up purposes,3,4,7,8 a suitable plan should advise that. The spirometer becomes an essential resource to be found at all healthcare centres.9,10 Likewise, it is important that allergic studies are performed by means of a prick-test or specific IgE levels, and these resources should be available to physicians caring for asthmatic children.10 Moreover, education is essential for optimal asthma control, and training for both patients and their families, provided by paediatricians and nurses through programmed individual and group activities is paramount.11
In the Spanish healthcare system, Primary Care Paediatricians (PCP) are the initial contact of children with the healthcare system,12 and they have responsibility for the care of common chronic diseases in childhood, like asthma. However, the availability of the resources they have is not homogeneous, and the asthma services they offer vary widely. The existence of a regional plan for care of asthmatic children, the availability of resources like spirometers or allergic tests, and the implication of paediatric nurses in the management of these children could be influential in the number and quality of the services offered to asthmatic patients.
The objective of this study is to describe the care provided to asthmatic patients by PCPs in Spain and the resources, both material and human, that these physicians have for the diagnosis and follow-up of the disease. Likewise, it analyses the relationship between existing asthma plans/guidelines in the various regions of Spain.
Material and methodsDesignThis research is based on a descriptive, cross-sectional study carried out using an online survey for PCPs in Spain to learn about the resources available to them and the type of care they provide their asthma patients.
SampleAll registered members of the Spanish Association of Primary Care Paediatricians (AEPap) in May of 2014 (n=3555). The AEPap is a scientific association made up of PCPs from all over Spain. In Primary Care (PC), paediatricians are distributed in the various Healthcare Centres located in the Autonomous Regions making up Spain; these specialists care for children and adolescents from birth until they are 14 years of age.
From a population of 3555 AEPap registered members, and a maximum indetermination criterion, we calculated that at least 347 valid responses would have been needed to make estimations with a 95% confidence level and a precision of ±5%.
Explicative dichotomous variables (yes/no)- •
Asthma plan: Programme or procedure that includes the planning, logistics, strategy, resources and coordination between levels of care (primary care and hospital) to improve the care and quality of life for the child and/or adolescent with asthma and their families. Such programmes are developed by technicians with the support of public healthcare administration in a given region.
- •
Asthma guideline: Document designed to serve as procedures based on scientific knowledge to standardise and improve healthcare and the quality of life of children and/or adolescents with asthma and their families. It is considered that an Autonomous Region has an asthma guideline when this has been developed by technicians in that Region, usually backed by public administration.
Both plans and guidelines have the common aim of improving healthcare and can positively influence it. Consequently, they have been included within the same variable.
- •
Programmed asthma visit: Specific office visit on the professional agenda (paediatrician/nurse) to attend asthma patients with an established schedule.
- •
Nurse participation: The nurse shares responsibilities, together with the paediatrician, for the care and education of asthma patients.
- •
Availability of spirometer at the healthcare centre
- •
Carrying out allergy tests at the healthcare centre. Access to determination of specific IgE levels at the reference lab and/or prick-test at the Healthcare Centre.
Thanks to the cooperation of the AEPap Secretariat, an email was sent to all members in May 2014 inviting them to participate in the study. It included a link to the survey. Answers were anonymous and were filled out online using Google Drive “Forms” during a limited, two-week period of time. As the emailing coincided with no festivities or holidays, it was understood that the email was received by most of the paediatricians. The survey included 33 items that assessed paediatricians’ socio-demographics, medical aspects and the resources available for diagnosis and the follow-up of asthma based on the recommendations of current clinical guidelines.3,4,7,8
Statistical analysisA descriptive analysis of the variables was carried out. To ascertain any possible differences in the assignment of human and material resources between Regions with and without asthma plans/guidelines, a bivariate analysis of the variable was performed by applying Pearson's chi-squared test (χ2). The level of statistical significance was considered p<0.05.
A latent class model (LCM) was used to study the possible existence of patterns associating educational and programmed activities with critical variables such as accessibility of resources, participation of nurses and availability of action plans or guidelines. Latent Gold 4.5® (Statistical Innovations Inc., Belmont, MA, USA) was used. LCM explores the existence of “classes,” groups or patterns that are not defined by the researcher and that explain the variability of the sample. The researcher only specifies the variables analysed, but does not pre-establish any condition that the classes must meet. LCM models were established with a number of classes between 1 and 5. The model chosen as the best was the one that both minimised the Akaike Information Criterion (AIC) and significantly improved the model adjustment with one less class than the bootstrap-LL2 test.
ResultsA total of 708 surveys were received from the group of 3555 members (20% response rate). Of these, 675 (95%) were considered valid for analysis; they corresponded to paediatricians working in primary care (PC). The remaining 33 were eliminated from the analysis as they corresponded to paediatricians who were not currently working in PC.
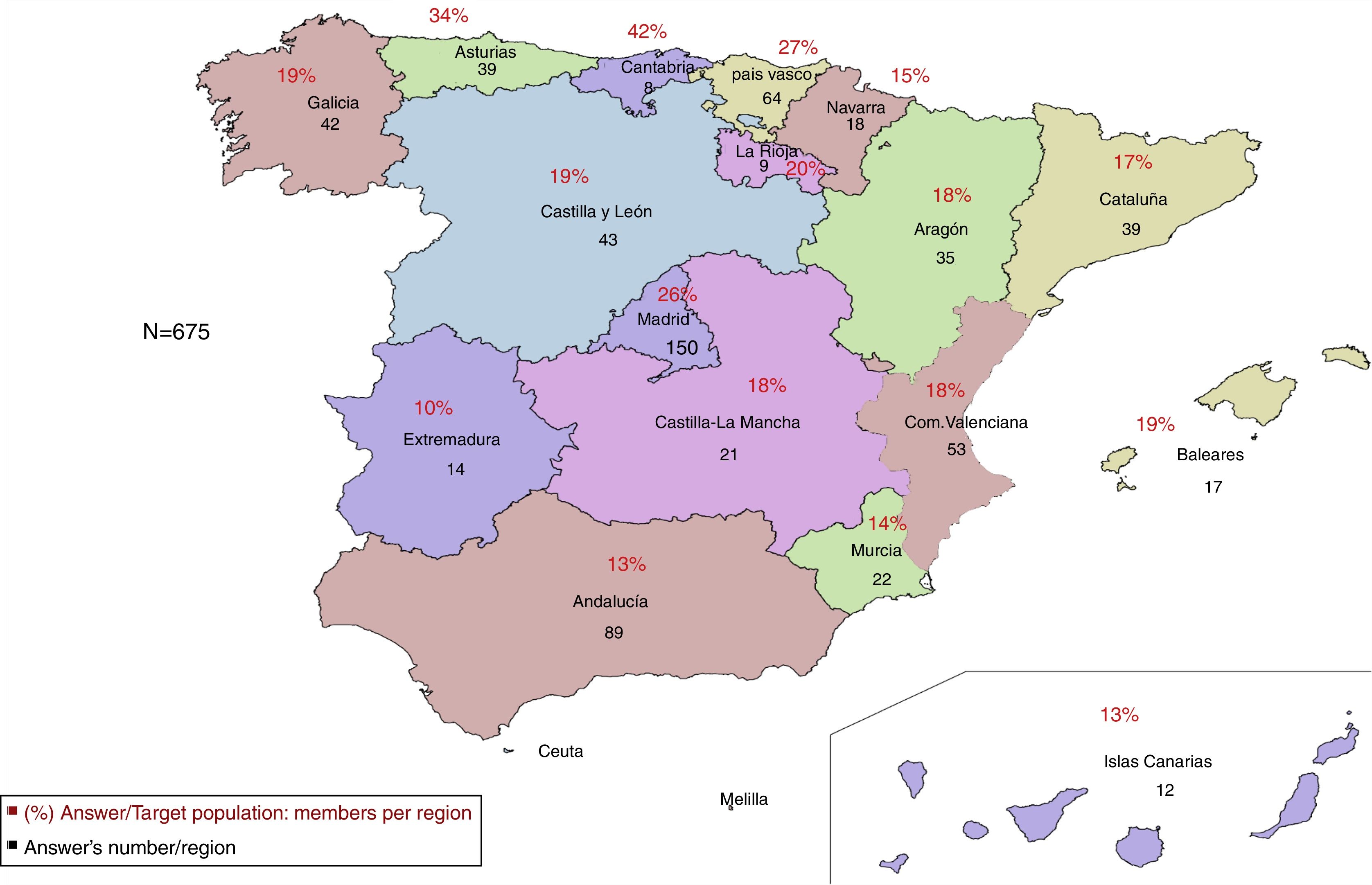
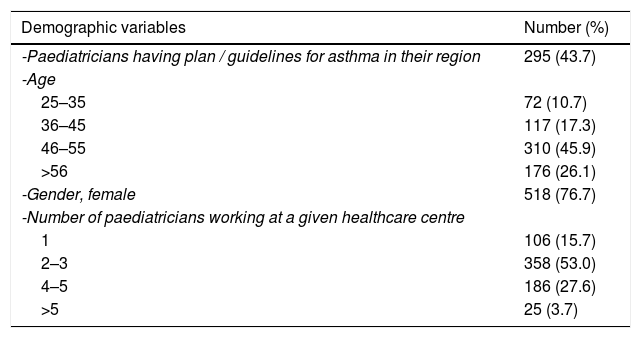
Data was obtained from paediatricians in the 17 Autonomous Communities (Fig. 1). Most of the respondents were women between the ages of 46 and 55 years who work in a healthcare centre with a team of two or three paediatricians (Table 1). 44% were Primary Care Paediatricians (PCP) in one of the eight regions that had developed and published asthma plans/guidelines (Andalusia, Aragon, Asturias, Balearic Islands, Cantabria, Castilla-León, Catalonia and the Basque Country).
Response rate per Region. Each Region of Spain is represented by the percentage % of paediatricians in a given Region who responded to the survey with regards to the number of AEPap members in that Region in May of 2014. The absolute values represent the number of paediatricians responding the survey in each Region.
Demographic variables: resources and planning.
| Demographic variables | Number (%) |
|---|---|
| -Paediatricians having plan / guidelines for asthma in their region | 295 (43.7) |
| -Age | |
| 25–35 | 72 (10.7) |
| 36–45 | 117 (17.3) |
| 46–55 | 310 (45.9) |
| >56 | 176 (26.1) |
| -Gender, female | 518 (76.7) |
| -Number of paediatricians working at a given healthcare centre | |
| 1 | 106 (15.7) |
| 2–3 | 358 (53.0) |
| 4–5 | 186 (27.6) |
| >5 | 25 (3.7) |
| Healthcare resources and planning | Number of paediatricians (%) answered yes |
|---|---|
| -Do you have a spirometer at your workplace? | 516 (76.4) |
| -Do you have a peak-flow metre at your workplace? | 396 (58.7) |
| -Have you been trained in the use and assessment of peak-flow? | 375 (55.6) |
| -Do you have prick-test material at your workplace? | 114 (16.9) |
| -May you request specific IgE? | 506 (75.0) |
| -May you request a sweat test? | 480 (71.1) |
| -May you perform or request exhaled nitric oxide levels? | 49 (7.3) |
| -Do you have an inhalation chamber for demonstrations? | 656 (97.2) |
| -Do you have placebos to teach inhalation techniques? | 639 (94.7) |
| -At your healthcare centre, is there a common programme for all paediatricians attending children with asthma? | 227 (33.6) |
| -In your healthcare district, is there a plan or programme attending children with asthma that coordinates Primary Care and the Hospital? | 116 (17.2) |
| -In your Region, is there a programme to attend childhood asthma? | 403 (59.7) |
At the healthcare centres, 76% of the paediatricians had access to spirometers, specific IgE (75%) and/or prick-test 17%. Almost all had some type of placebo inhaler (95%) and inhalation chambers (97%) to teach and educate in inhalation techniques (Table 1).
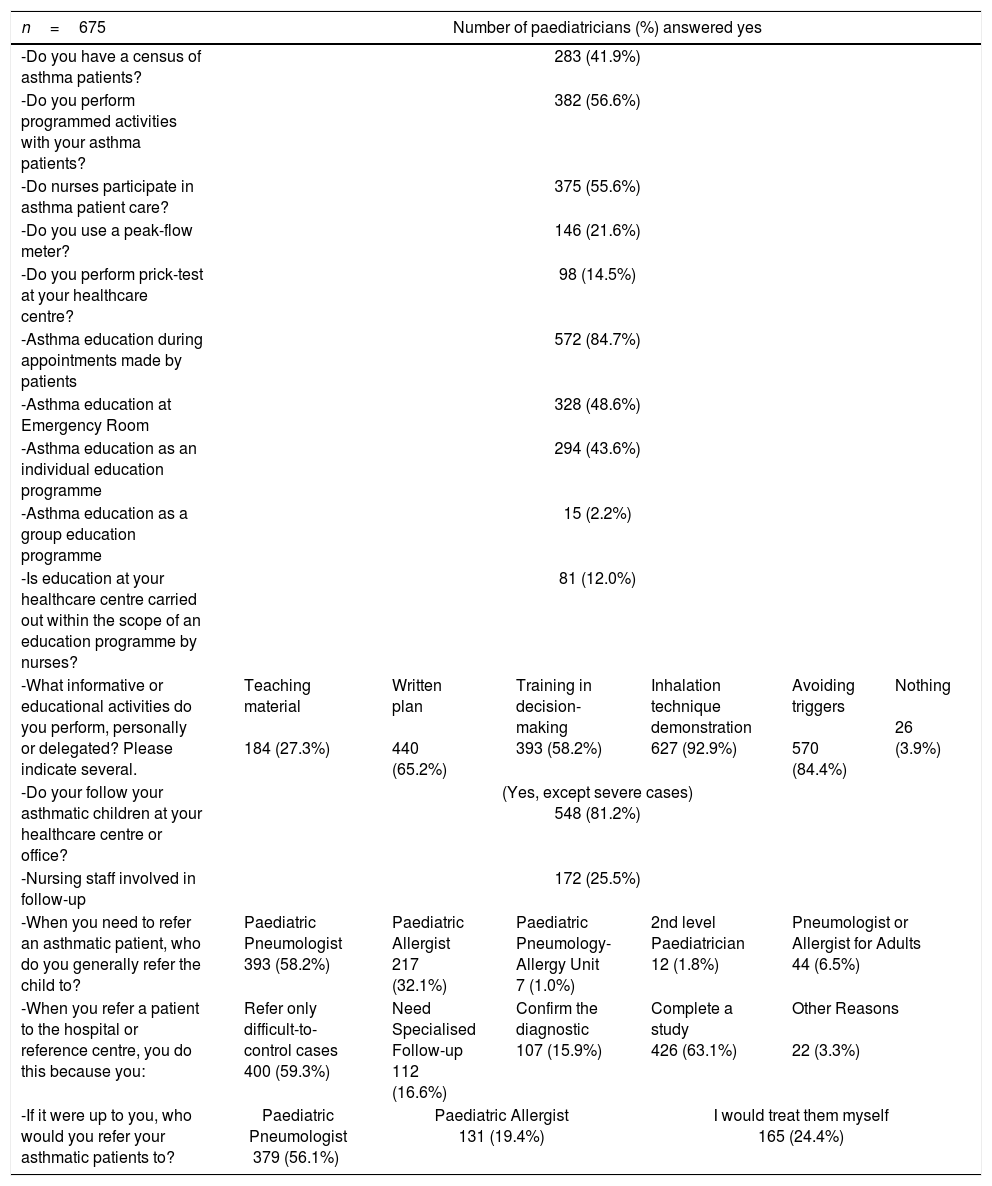
In terms of the attention provided, less than half of the paediatricians surveyed (42%) had a census of their asthma patients (Table 2). 57% performed programmed activities with their patients. Educating patients and/or families in asthma was, for the most part, done individually during appointments made by the patient (85%) rather than a visit programmed by the doctor. Only 2% offered group education. Inhalation techniques and how to avoid triggers were the main educational aspects covered, followed by a written action plan. Essentially, patients were referred to the hospital to complete the diagnosis or when asthma was difficult to control. Except in the cases of severe asthma, most paediatricians performed follow-up at the PC centre.
Characteristics of patient care.
| n=675 | Number of paediatricians (%) answered yes | |||||
|---|---|---|---|---|---|---|
| -Do you have a census of asthma patients? | 283 (41.9%) | |||||
| -Do you perform programmed activities with your asthma patients? | 382 (56.6%) | |||||
| -Do nurses participate in asthma patient care? | 375 (55.6%) | |||||
| -Do you use a peak-flow meter? | 146 (21.6%) | |||||
| -Do you perform prick-test at your healthcare centre? | 98 (14.5%) | |||||
| -Asthma education during appointments made by patients | 572 (84.7%) | |||||
| -Asthma education at Emergency Room | 328 (48.6%) | |||||
| -Asthma education as an individual education programme | 294 (43.6%) | |||||
| -Asthma education as a group education programme | 15 (2.2%) | |||||
| -Is education at your healthcare centre carried out within the scope of an education programme by nurses? | 81 (12.0%) | |||||
| -What informative or educational activities do you perform, personally or delegated? Please indicate several. | Teaching material 184 (27.3%) | Written plan 440 (65.2%) | Training in decision-making 393 (58.2%) | Inhalation technique demonstration 627 (92.9%) | Avoiding triggers 570 (84.4%) | Nothing 26 (3.9%) |
| -Do your follow your asthmatic children at your healthcare centre or office? | (Yes, except severe cases) 548 (81.2%) | |||||
| -Nursing staff involved in follow-up | 172 (25.5%) | |||||
| -When you need to refer an asthmatic patient, who do you generally refer the child to? | Paediatric Pneumologist 393 (58.2%) | Paediatric Allergist 217 (32.1%) | Paediatric Pneumology-Allergy Unit 7 (1.0%) | 2nd level Paediatrician 12 (1.8%) | Pneumologist or Allergist for Adults 44 (6.5%) | |
| -When you refer a patient to the hospital or reference centre, you do this because you: | Refer only difficult-to-control cases 400 (59.3%) | Need Specialised Follow-up 112 (16.6%) | Confirm the diagnostic 107 (15.9%) | Complete a study 426 (63.1%) | Other Reasons 22 (3.3%) | |
| -If it were up to you, who would you refer your asthmatic patients to? | Paediatric Pneumologist 379 (56.1%) | Paediatric Allergist 131 (19.4%) | I would treat them myself 165 (24.4%) | |||
56% of the paediatricians stated the nurses participated in asthma patient care, although only a fourth of these were involved in follow-up. Only 12% collaborated in the education programmes.
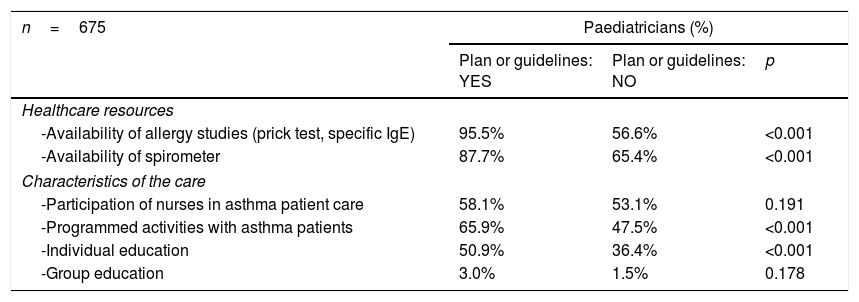
The bivariate analysis (Table 3) showed that in those Regions with asthma plans/guidelines, the paediatricians had more resources (spirometer and allergy tests) and offered more programmed activities and individual education than those with fewer resources (p<0.01). However, no differences were observed in the participation of nurses (p=0.191).
Bivariate analysis (Chi square): association between having asthma plan/guideline in the Region with the resources and assistance.
| n=675 | Paediatricians (%) | ||
|---|---|---|---|
| Plan or guidelines: YES | Plan or guidelines: NO | p | |
| Healthcare resources | |||
| -Availability of allergy studies (prick test, specific IgE) | 95.5% | 56.6% | <0.001 |
| -Availability of spirometer | 87.7% | 65.4% | <0.001 |
| Characteristics of the care | |||
| -Participation of nurses in asthma patient care | 58.1% | 53.1% | 0.191 |
| -Programmed activities with asthma patients | 65.9% | 47.5% | <0.001 |
| -Individual education | 50.9% | 36.4% | <0.001 |
| -Group education | 3.0% | 1.5% | 0.178 |
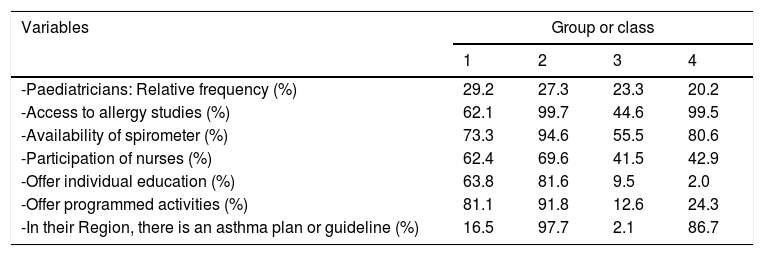
The latent class analysis selected a model with four classes or groups. Those four groups (Table 4) had a frequency that was quite similar (between 20 and 30% for each one). This could be described as:
Group 1: Paediatricians who, despite working in a Region with limited implementation of plans/guidelines and having moderate access to resources, a high nurse participation allows for many programmed and educational activities to be carried out.
Group 2: Paediatricians working in a Region that implements plans/guidelines, with high access to resources, high nurse participation and many programmed and educational activities.
Group 3: Paediatricians working in a Region without plans/guidelines, with low access to resources, low participation of nurses and hardly offering programmed and educational activities.
Group 4: Paediatricians who, despite working in a Region that implements plans/guidelines and with sufficient resources, have limited participation of nurses and offer few programmed and educational activities.
Profile of the groups formed in the Latent Class Analysis.
| Variables | Group or class | |||
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |
| -Paediatricians: Relative frequency (%) | 29.2 | 27.3 | 23.3 | 20.2 |
| -Access to allergy studies (%) | 62.1 | 99.7 | 44.6 | 99.5 |
| -Availability of spirometer (%) | 73.3 | 94.6 | 55.5 | 80.6 |
| -Participation of nurses (%) | 62.4 | 69.6 | 41.5 | 42.9 |
| -Offer individual education (%) | 63.8 | 81.6 | 9.5 | 2.0 |
| -Offer programmed activities (%) | 81.1 | 91.8 | 12.6 | 24.3 |
| -In their Region, there is an asthma plan or guideline (%) | 16.5 | 97.7 | 2.1 | 86.7 |
Currently, the importance of controlling asthma is stressed in order to decrease its morbidity, healthcare costs and improve patient's quality of life.3,4,7 However, this demands the necessary resources to be available and the implication and training of the healthcare staff attending these patients.
In the United States, where there are a number healthcare models, there is evidence that patients who usually use Primary Care services receive more preventive measures, are healthier and have lower mortality rates than those who are seen solely by specialists or receive other medical care. Reinforcing a healthcare model in which PC cares for chronic patients improves healthcare results, reduces medical overload and the costs for chronic patients with asthma.13 In another study with asthmatic adults in eleven European countries, most of the patients stated that it was their PC doctor who performed the control of their disease, with specialised nurses also being involved in some countries.14 In the European Union, from the Public Health point of view, PC is considered the cornerstone for the prevention and control of childhood asthma and allergic diseases.15
Given the characteristics of Spain's healthcare system, most children and adolescents with asthma initially consult their PCP, thus making it the ideal setting for early patient diagnosis and follow-up.
This is the first study providing information about how asthma is handled by including a sample with data from PCP in the 17 Autonomous Communities of Spain. The characteristics of the paediatricians described herein (age, predominance of women and number of professionals per healthcare centre) most probably adjusts to the reality of PCPs in Spain. It is noteworthy to see the diversity both in terms of resources as well as in how asthma is handled by paediatricians.
Our results show that those Regions with local asthma plans/guidelines have more resources than those without. However, this does not mean that guidelines are being used adequately. Initially, the bivariate analysis revealed that in those Regions with plans/guidelines and more resources, the paediatricians undertook more asthma-related programmed activities and education than in those Regions with none. Nevertheless, the latent class analysis showed that the participation of nurses played an important role in these activities. Paediatricians were involved in more educational activities and programmed visits with their asthma patients when they counted on greater participation from nurses, independently of the existence of plans/guidelines (Table 4).
A Cochrane Collaboration meta-analysis included five studies with asthmatic children and adults. It compared patient care done by general practitioners versus nurses. No differences were found in terms of the number of crises and the quality of life in the follow-up ranging from six months to two years. Thus, these same authors concluded that although the number of studies was limited, nurses could carry out follow-up of well-controlled asthma patients.16
In Spain, PC childhood-adolescent healthcare falls within the scope of paediatricians and nurses. However, not all paediatric teams have a paediatric nurse; this differs from one Region to another. Moreover, this responsibility varies greatly from one healthcare centre to another.17
In our study, over 80% of the paediatricians performed patient follow-up at the PC office, although having support nurses was not always a possibility. In the light of our results, the paediatrician-paediatric nurse teams should be reinforced at all PC healthcare centres. Greater implication of nurses should be promoted for asthma patient care.
Despite the procedures established in the guidelines to better control asthma,3,4,7,8,18,19 the reality is that in many cases the clinical practice at PC and hospitals does not meet said recommendations.20,21 Some guidelines provide specific indications for handling asthma in PC; nevertheless, barriers and possible solutions continue to be identified to facilitate adherence.22,23
The Primary Care model can also influence how asthma is cared for. In Canada, the quality of asthma care varies depending on the model used (co-payment, premium, etc.).24 Another study was carried in Washington DC at 22 Primary Care clinics or doctor's offices. The results show that the children who routinely took preventive and educational measures at their clinics were free of symptoms for more days and went to the emergency room less than those who did not receive such care.25
In Spain, the National Healthcare System established a list of common services, with chronic diseases being included in paediatrics, but without specifying them. Healthcare is the responsibility of the regional government and as such, each Region designs its own services.26 Some Regions have developed asthma plans/guidelines, but implementation and adherence are far from uniform. Therefore, it is not surprising that when paediatricians were asked whether or not they had a childhood asthma programme in their Region, there was not always concordance between Regions that had published plans/guidelines and the knowledge of these guidelines on behalf of their paediatricians. In any case, to facilitate implementation and adherence, not only are resources and the development of documents recommended, but it is also essential to disseminate information, create teams and train all those involved. It is crucial that assessment indicators be established, and results published. There is clear evidence that such plans or programmes are highly cost-effective for both patients and society in general.27
Sweden offers another perspective. There, PC professionals attending children with asthma (GPs or nurses who are experts in asthma) showed limited adherence to national guidelines. Among the quality indicators prioritised to assess the results of asthma care are the spirometer and allergy tests. Non-pharmacological treatment indicators, such as patient education and the administration of a written action plan are linked to improved adherence and asthma control.28 In Spain, the clinical practice guideline for childhood asthma also proposes the assessment of implementation indicators for both treatment and education (verify the correct use of inhalers and facilitate a written plan of action).8 Inadequate use of inhalers is the first cause of failed treatment. There is proof that children following an action plan based on symptoms have fewer night-time awakenings, miss less school and go the emergency rooms less.29
In a chronic disease such as asthma, education is an essential part of treatment. Some authors consider training and education a better option to control asthma than the development of new drugs.30 Asthma education not only decreases the risk of exacerbations and healthcare costs, but by controlling the disease better, it increases the quality of life for both patients and caregivers.31–32 In Spain, a study undertaken by PCP revealed that upon analysing socio-cultural aspects and family functioning, there is a clear and obvious relationship between asthma control in children and their parents’ quality of life.33
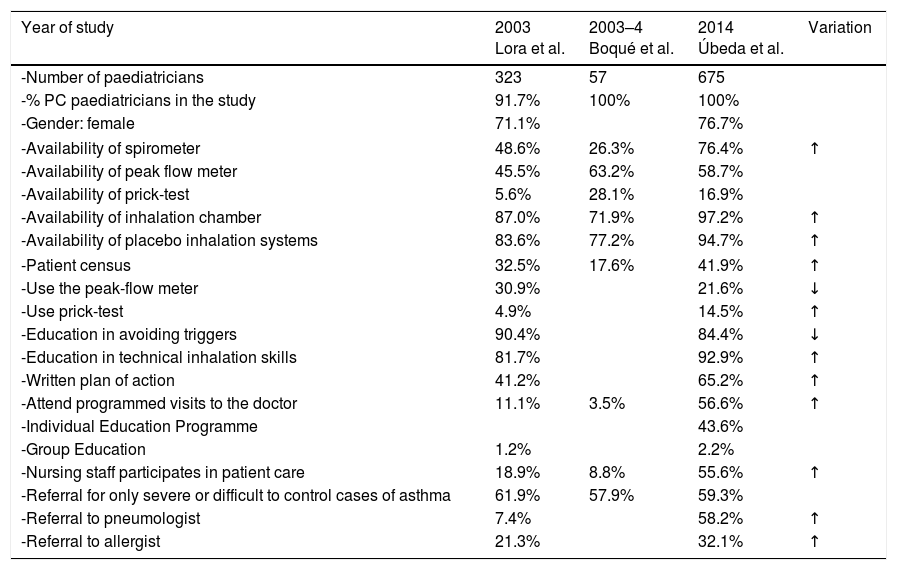
Other studies in Spain also reviewed how childhood asthma is handled in Primary Care. More than a decade ago, Lora et al.34 published an article about anonymous surveys, filled out by PCPs attending an asthma training course in seven different cities of Spain. Boqué et al.35 also reported local data for the island of Mallorca. Upon comparing our results with these studies (Table 5), it is observed that resources have increased in recent years; there are more programmed visits to the doctor, written plans of action are provided, and the involvement of nurses is greater. Both before and now, PCP see the importance of educating children in the use of inhalers and avoiding triggers, but not everyone provides a written action plan for treatment and how to react when a special situation arises.
Development of resources and asthma care for Primary Care Paediatricians.
| Year of study | 2003 Lora et al. | 2003–4 Boqué et al. | 2014 Úbeda et al. | Variation |
|---|---|---|---|---|
| -Number of paediatricians | 323 | 57 | 675 | |
| -% PC paediatricians in the study | 91.7% | 100% | 100% | |
| -Gender: female | 71.1% | 76.7% | ||
| -Availability of spirometer | 48.6% | 26.3% | 76.4% | ↑ |
| -Availability of peak flow meter | 45.5% | 63.2% | 58.7% | |
| -Availability of prick-test | 5.6% | 28.1% | 16.9% | |
| -Availability of inhalation chamber | 87.0% | 71.9% | 97.2% | ↑ |
| -Availability of placebo inhalation systems | 83.6% | 77.2% | 94.7% | ↑ |
| -Patient census | 32.5% | 17.6% | 41.9% | ↑ |
| -Use the peak-flow meter | 30.9% | 21.6% | ↓ | |
| -Use prick-test | 4.9% | 14.5% | ↑ | |
| -Education in avoiding triggers | 90.4% | 84.4% | ↓ | |
| -Education in technical inhalation skills | 81.7% | 92.9% | ↑ | |
| -Written plan of action | 41.2% | 65.2% | ↑ | |
| -Attend programmed visits to the doctor | 11.1% | 3.5% | 56.6% | ↑ |
| -Individual Education Programme | 43.6% | |||
| -Group Education | 1.2% | 2.2% | ||
| -Nursing staff participates in patient care | 18.9% | 8.8% | 55.6% | ↑ |
| -Referral for only severe or difficult to control cases of asthma | 61.9% | 57.9% | 59.3% | |
| -Referral to pneumologist | 7.4% | 58.2% | ↑ | |
| -Referral to allergist | 21.3% | 32.1% | ↑ | |
In the Boqué study, 95% of the paediatricians considered themselves able to perform the follow-up of asthmatic children in PC, although they mentioned barriers such as lack of time, absence of material and human resources, training and motivation. In our study, most paediatricians (81%) performed follow-up at their PC office. When paediatricians referred their patients to a hospital specialist, it was, for the most part, to complete a study or for hard-to-control cases of asthma. This is in line with previous Spanish studies, although now more patients are referred to a pneumologist rather than an allergist. Very few paediatricians (17%) responded that there was a programme in their healthcare district that coordinated both levels of medical coverage (PC and hospital). Clearly, this is an area for improvement.
Limitations of the studyThe authors of this article are well aware of the difficulties entailed when trying to extrapolate the results to Spain's entire PCP population, as the survey was sent to members of a single PC association, where most paediatricians work in the public sector. Another limitation is the low response rate; this is probably due to the deadline established for answers. A reminder email was not sent, which might have increased the response rate. However, most of the answers were received within the first 10 days. Although a selection bias is possible for the most motivated paediatricians, we think that our sample is representative in the sense that it incorporates the high variability in the disease handling and resource availability in Spain. This is the main strength, as including PCP from every Spanish region, we were able to show the strong relationship between planning of asthma care, professional involvement and quality of the asthma services provided. Despite these limitations, the results offer interesting data to compare with previous studies, and lead us to ponder on the subject to reach conclusions.
ConclusionsIn Spain there is a high variability in the care of children and adolescents with asthma. The availability of asthma plans/guidelines in the various Regions is associated with higher availability of resources, but this is insufficient to improve important aspects of the medical care provided to children with asthma. Paediatricians that count on greater involvement of their nurses carry out more programmed and educational activities, independently of whether or not there are plans/guidelines in that Region. Organisational changes are needed to include programmed visits and paediatric teams with greater participation of nurses in the care of these patients.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestNone of the authors have any conflict of interest regarding this paper.
The authors are grateful to all of the Spanish paediatricians who participated in the survey.