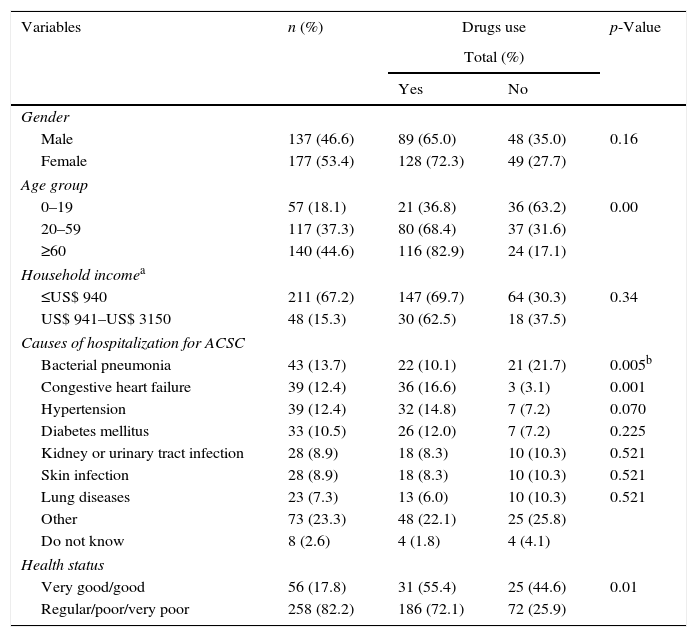
Brazil is currently expanding Primary Health Care (PHC)1 with the coexistence of two different models – the traditional model comprising Basic Health Units (BHU) and the Family Health Program (FHP). Hospitalizations for Ambulatory Care Sensitive Conditions (ACSC) have been used as an indicator to evaluate the quality of PHC,2 as they represent health problems that must be addressed and treated opportunely at this level of care. We have hypothesized that drug users would rate PHC more highly, since drugs can strengthen the relationship between users and the healthcare services. In a cross-section study conducted within two public inpatient services in Divinópolis city, Brazil, we compared the assessment of the PHC, as rated by patients hospitalized for ACSC, comprising users and non-users of drugs, referred to FHP or BHU. Participants were interviewed (n=314; 69.1% drug users) and asked to answer questions related to socio-demographic, clinical/therapeutic characteristics (Table 1) and to the PHC performance,3 comprising the key attributes accessibility, gatekeeping, longitudinality, comprehensiveness, coordination, family focus, community orientation and professional training. Responses follow a Likert-type scale ranging from zero to five, allowing the calculation of a general and partial indexes based on the arithmetic mean of the response scores. Groups were compared through Student's t-test (α=0.05).2
Sociodemographic characteristics and health status of drugs users versus non-users, Divinopolis, 2011 (n=314).
| Variables | n (%) | Drugs use | p-Value | |
|---|---|---|---|---|
| Total (%) | ||||
| Yes | No | |||
| Gender | ||||
| Male | 137 (46.6) | 89 (65.0) | 48 (35.0) | 0.16 |
| Female | 177 (53.4) | 128 (72.3) | 49 (27.7) | |
| Age group | ||||
| 0–19 | 57 (18.1) | 21 (36.8) | 36 (63.2) | 0.00 |
| 20–59 | 117 (37.3) | 80 (68.4) | 37 (31.6) | |
| ≥60 | 140 (44.6) | 116 (82.9) | 24 (17.1) | |
| Household incomea | ||||
| ≤US$ 940 | 211 (67.2) | 147 (69.7) | 64 (30.3) | 0.34 |
| US$ 941–US$ 3150 | 48 (15.3) | 30 (62.5) | 18 (37.5) | |
| Causes of hospitalization for ACSC | ||||
| Bacterial pneumonia | 43 (13.7) | 22 (10.1) | 21 (21.7) | 0.005b |
| Congestive heart failure | 39 (12.4) | 36 (16.6) | 3 (3.1) | 0.001 |
| Hypertension | 39 (12.4) | 32 (14.8) | 7 (7.2) | 0.070 |
| Diabetes mellitus | 33 (10.5) | 26 (12.0) | 7 (7.2) | 0.225 |
| Kidney or urinary tract infection | 28 (8.9) | 18 (8.3) | 10 (10.3) | 0.521 |
| Skin infection | 28 (8.9) | 18 (8.3) | 10 (10.3) | 0.521 |
| Lung diseases | 23 (7.3) | 13 (6.0) | 10 (10.3) | 0.521 |
| Other | 73 (23.3) | 48 (22.1) | 25 (25.8) | |
| Do not know | 8 (2.6) | 4 (1.8) | 4 (4.1) | |
| Health status | ||||
| Very good/good | 56 (17.8) | 31 (55.4) | 25 (44.6) | 0.01 |
| Regular/poor/very poor | 258 (82.2) | 186 (72.1) | 72 (25.9) | |
The attributes family focus and coordination were rated worst by drug users. However, a significant difference was observed only for coordination (p=0.003). This attribute assesses whether the provision of a mix of services and information caters to users’ needs and involves a link among the services promoting care continuity.4
By taking the model of PHC into account the attribute gatekeeping proved the exception on the comparison between drug users and non-users, being rated higher by drug users treated at BHU (p=0.01). This attribute assesses the actual use of the PHC unit as the first contact with the public health system upon each need for health care assistance.4 Considering the principles of FHP, this type of service was expected to gain a higher rating than BHU, but revealed only a modest expansion with no indication of improvement in quality and the existence of a reactive and episodic care model.5
The PHCI, as assessed by both groups, was around 60% of the maximum score (5 points) without differences between drug users and non-users (p>0.05). We believe our findings could be partially explained by the poor pharmaceutical services offered in the municipality, not allowing distinguishing the quality of the PHC services provided to drug users and non-users. A total of 64% of users reported that the prescribed drugs (n=932) were not always available from the public health services. Problems acquiring medications, can constitute a major cause of treatment failure, with consequent worsening of health status and even an increase in ACSC and avoidable hospitalizations, and most likely explain the poorer health status reported by drug users (Table 1). Another direct repercussion of this failure by PHC to regularly replenish drug stocks is the impact of this cost on the monthly budget of interviewees. Around 70% of the study population had an average income of up to three minimum wages and, among those reporting the amount spend on drugs, 30.6% reported spending over a third of a minimum wage on them, seriously impacting the family budget.6
Considering that availability of essential drugs should exceed 80%, the provision of drugs by the public health service in the city falls below recommended levels, highlighting a serious problem accessing medications with an inevitable impact on the quality of health care. This scenario suggests potential interruption in the provision of services and continuity of care, resulting in dissatisfaction among drug users.
FundingFoundation for Supporting Research in the State of Minas Gerais (FAPEMIG) (grant numbers APQ-03031/10 and APQ-04390/10).
Ethical approvalThis investigation complied with Resolution 196/96, which regulates human subject research. All the ethical principles contained in the Declaration of Helsinki were observed and the research project was approved by the Institutional Review Board/Research Ethics Committee of Hospital São João de Deus, Divinópolis, Minas Gerais state, file number 25/2011.
Conflict of interestNone.