The future of General Practice/Family Medicine, as an academic and scientific discipline, will be not only the clinical activity of GPs but also the creation of own content through research; a PhD is a good start. The complexity of the PhD supervisor–student relationship is well known and it has even been compared to the doctor–patient relationship.1 A good relationship may decrease the challenges of a PhD for young GPs.
The aim of this study was to characterize the style of the PhD supervisor in primary care from the perspective of the supervised, and to compare the differences between the experienced supervisor behaviour and the preferred/ideal behaviour.
A cross-sectional, descriptive study was conducted. Twenty-nine PhD students/young PhD graduates (bellow 45 years old) that were also practicing GPs (or GP Trainees) were approached by email to participate in the study. To the best of the author's knowledge they represent the Portuguese national sample.
The questionnaire on supervisor–doctoral student interaction (QSDI), an instrument developed to study the supervisor–student relationship,2 was available for filling in online. It was administered in English. Participants were instructed to fill in two versions of the QSDI: one asking for the experienced supervisor behaviour and the other for the preferred/ideal behaviour. For each question a 5-point Likert scale (from never/not at all to always/very) was used. The questionnaire was completely anonymous.
Standard descriptive analyses were performed. Means and standard deviations were reported to facilitate comparison with previous studies. Student's t-test was used to compare the experienced supervisor behaviour to the preferred/ideal behaviour. p values <0.05 were considered statistically significant.
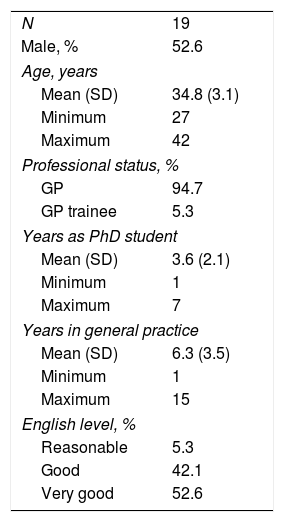
Nineteen PhD students/young PhD graduates agreed to participate (response rate of 65.5%). Background characteristics of respondents are summarized in Table 1.
Characteristics of the sample.
| N | 19 |
| Male, % | 52.6 |
| Age, years | |
| Mean (SD) | 34.8 (3.1) |
| Minimum | 27 |
| Maximum | 42 |
| Professional status, % | |
| GP | 94.7 |
| GP trainee | 5.3 |
| Years as PhD student | |
| Mean (SD) | 3.6 (2.1) |
| Minimum | 1 |
| Maximum | 7 |
| Years in general practice | |
| Mean (SD) | 6.3 (3.5) |
| Minimum | 1 |
| Maximum | 15 |
| English level, % | |
| Reasonable | 5.3 |
| Good | 42.1 |
| Very good | 52.6 |
There were no significant differences between the experienced and the preferred supervisor behaviour regarding the scales “giving PhD students freedom and responsibility”, “uncertain”, “dissatisfied”, and “admonishing”.
In addition, participants perceived their supervisors as displaying less “leadership”, “helping/friendly”, “understanding”, and “strict” behaviours than they should ideally display. In detail, participants consider that supervisors should ideally: (i) give more thorough feedback on students’ work (p=0.011), (ii) explain more comprehensively when students ask something (p=0.03), (iii) give more clear guidance (p=0.012), (iv) give more advice (p=0.004), (v) anticipate more possible misunderstandings between the two (p<0.001), (vi) support more (p=0.008), (vii) be more reliable (p=0.049), (viii) listen more (p=0.003), (ix) pay more attention (p=0.015), (x) be more quick to criticize (p=0.007), (xi) be more critical (p=0.014), (xii) be more strict when evaluating the supervised progress (p=0.042), (xiii) demand more (p=0.08), and (xiii) be faster correcting supervised mistakes (p=0.014).
Consistent with previous research,2 this study found that the average PhD supervisor profile is one that displays much leadership, help and friendliness, comprehension and provision of supervised responsibility and freedom. The strict behaviour is moderate and supervisors do not show a lot of uncertain, dissatisfied or admonishing behaviour.2
The main limitation of the current study is the size of the sample; it may not be representative of the entire population of PhD students/young PhD graduates in primary care. Even so, the response rate of 65.5% was adequate. Future research with larger samples will be possible as increasing numbers of GPs enrol in PhD programmes. For example, it would be worthwhile to study if the immaturity in the professional career as a GP could change the ideal supervisor behaviour (i.e. a needier supervised). Investigating the supervisors’ behaviour from their own point of view will also be an important effort for understanding the full spectrum of the relationship.
Although any extrapolation of the results should be done with caution, the current study found that the PhD supervisor profile in primary care is not different from the profile found in other settings. Nonetheless, in primary care some supervisor behaviours need to be improved.