Telemedicine is a real-time interactive communication method where patients are assessed and treated remotely. Epilepsy is one of the most frequent neurological disorders in childhood. However, specialists and subspecialists are scarce in rural settings. In neurology, telemedicine has been shown to be useful in the treatment of epilepsy and other neurodevelopmental disorders.
MethodsWe gathered data from patients diagnosed with epilepsy and managed through telemedicine consultations from January 2011 to February 2020. We collected data on the number of consultations, town/city of origin, treatment, aetiology, seizure type, treatment adherence, loss to follow up, discharges, and comorbidities.
ResultsWe identified a total of 467 patients (180 girls and 287 boys). The largest age group was pre-school children, with 160 cases (34.2%). Seizures were focal in 253 cases (54.2%) and generalised in 214 (45.8%). Seizure aetiology was unknown in the majority of patients (69.3%). Ninety percent of patients presented good treatment adherence, and 76.8% were seizure-free. Regarding treatment, 351 patients (75%) were receiving monotherapy, and the most frequently prescribed drug was magnesium valproate, in 225 patients (64.2%). A total of 158 patients (33.8%) presented 1 comorbidity, and 19 (4%) presented 2 comorbidities.
ConclusionsIn our study, telemedicine proved to be effective in the treatment and follow-up of paediatric patients with epilepsy living in rural settings. Its usefulness in other neuropaediatric disorders should also be evaluated.
La telemedicina es un método de comunicación interactiva en tiempo real donde los pacientes son valorados y tratados por el médico en diferentes ubicaciones. La epilepsia es de los padecimientos neurológicos más frecuentes en la infancia. Es conocida la dificultad de contar con especialistas y subespecialistas en áreas no urbanas. En neurología, la telemedicina ha demostrado el beneficio en el tratamiento de epilepsia y otros trastornos del neurodesarrollo.
MétodoSe revisó la base de datos de telemedicina de enero del 2011 a febrero 2020 con diagnóstico de epilepsia. Se obtuvo número de consultas recibidas, ciudad de origen, tratamiento, etiología, tipo de crisis, apego al tratamiento, pacientes desertados, altas y comorbilidades.
ResultadosSe identificaron 467 pacientes, 180 femeninas y 287 masculinos. Por edad el grupo predominante fue el prescolar con 160 casos (34.2%). Respecto al tipo de crisis epiléptica 253 pacientes presentaron crisis focales (54.2%) y 214 crisis generalizadas (45.8%). La etiología más frecuente es la desconocida con 69.3% de casos. El 90% tienen buen apego al tratamiento y el 76.8% se encuentran sin crisis. 351 pacientes se encuentran con monoterapia (75%) y el fármaco más utilizado es el valproato de magnesio en 225 (64.2%). 158 pacientes presentan 1 comorbilidad (33.8%) y 19 con 2 comorbilidades (4%).
ConclusionesLa telemedicina es una herramienta digital que en nuestro estudio demostró ser eficaz en el tratamiento y seguimiento de pacientes pediátricos epilépticos en comunidades rurales de nuestra entidad. Debe seguir valorándose su utilidad en otros trastornos neuropediátricos.
Epilepsy is one of the most frequent neurological diseases in childhood. In most cases, the point of first contact between these patients and the healthcare system is the paediatrics department or the family medicine department.1 The scarcity of specialists and subspecialists in non-urban settings is well known. As a result, these patients often need to be transferred to distant hospitals, which involves high costs and results in increased care burdens at these reference centres.2
Telehealth is the use of communication technologies (telephones, smartphones, and wireless devices, with or without video) to provide medical care. Through these technologies, it has been possible for nearly 50 years not only to send images or medical histories but also to perform detailed clinical assessments and provide specialised treatments.3 The terms “telemedicine” and “telehealth” are frequently used interchangeably. Telemedicine is an interactive, audio- and video-based method of real-time bidirectional communication between patients and physicians that enables remote patient assessment, monitoring, and treatment. Teleconsultation, another telehealth modality, is the synchronous or asynchronous use of different technologies for communication between physicians to establish a diagnosis or treatment. Telepractice is the term used for communication exclusively between a patient and a physician. Telecare is when a patient is assessed, educated, or treated at home by a healthcare professional or a social worker, while tele-education enables remote training of healthcare professionals.4
The use of telemedicine in neuroscience is not new. In 1999, a telestroke programme was launched for patients with stroke,5 and was found to be safe and efficacious in reducing neurological sequelae and healthcare costs. In 2005, the programme was approved and telemedicine was recommended for the treatment of stroke.6,7 Subsequent studies have reported their experience with telemedicine for the management of such other conditions as traumatic brain and spinal cord injury, epilepsy, migraine, and dementia.8
This technology has also been used in paediatrics departments for over 30 years, for regular consultations, patient assessment and follow-up, and education programmes for patients and healthcare professionals from almost all subspecialties. Although few studies have addressed the application of telemedicine in the field of paediatric neurology, they have demonstrated the benefits of these technologies for the management of epilepsy and neurodevelopmental disorders.9–12
The State Telemedicine Network of San Luis Potosí, established in 2011, is formed by first- and second-level healthcare units in the state's 58 municipalities. This programme is targeted at the population with difficulties accessing specialised medical care. It aims to consolidate an efficient, universal State Healthcare System, with the ultimate goal of providing care to the state's population and protecting the most vulnerable groups.
This study evaluates the efficacy of the telemedicine programme in the diagnosis and treatment of paediatric patients with epilepsy at Hospital Central Dr. Ignacio Morones Prieto, in the city of San Luis Potosí, Mexico.
Material and methodsOur study was approved by our hospital's research ethics committee. All procedures were conducted in accordance with the World Health Organisation standards for human research and the Mexican General Health Law, and personal data were managed in compliance with Mexican data protection legislation. We reviewed the hospital's database to identify patients evaluated through telemedicine by the paediatric neurology department between January 2011 and February 2020. We selected only those patients who were assessed due to epilepsy, and gathered the following epidemiological data: number of patients, sex, age (grouped as follows: neonates, 0–28 days of life; infants, 29 days–1 year, 11 months, and 29 days; preschool children, 2 years–6 years, 11 months, and 29 days; school-age children, 7 years–11 years, 11 months, and 29 days; and adolescents, 12–15 years), number of consultations, town/city of origin, treatment, aetiology, and seizure type according to the latest International League Against Epilepsy (ILAE) classification,13 neuroimaging study results, electroencephalography results, treatment adherence, loss to follow-up, discharges, and comorbidities.
The cost analysis was based on data provided by the healthcare department of the state of San Luis Potosí (Table 1). Statistical analysis was performed using Microsoft Excel and the MegaStat add-in. Qualitative variables are expressed as absolute and relative frequencies (percentages) and quantitative variables as means and standard deviation.
Cost of in-person consultations per paediatric patient.
| Route | Transportation costs | Loss of productivity | Total savings |
|---|---|---|---|
| Huasteca-Valles | $1700.00 | $253.44 | $1953.44 |
| Huasteca-SLP | $5200.00 | $253.44 | $5453.44 |
| Valles-SLP | $4200.00 | $176.72 | $4376.72 |
| Río Verde-SLP | $2020.00 | $176.72 | $2196.72 |
| Matehuala-SLP | $1825.00 | $176.72 | $2001.72 |
$: Mexican pesos; SLP: San Luis Potosí.
We identified a total of 467 patients diagnosed with epilepsy: 180 girls (38.5%) and 287 boys (61.4%). Pre-school children constituted the most numerous age group (160 cases; 34.2%), followed by school-age children (139; 29.7%), adolescents (97; 20.7%), infants (70; 15%), and one neonate (0.21%).
A total of 253 patients (54.2%) presented focal-onset seizures, and 214 (45.8%) presented generalised seizures. The most frequent aetiology was unknown causes (69.3%), followed by structural lesions (20.13%), genetic or infectious causes (1.5%), and autoimmune causes (0.4%). Seven percent of patients presented an epileptic syndrome.
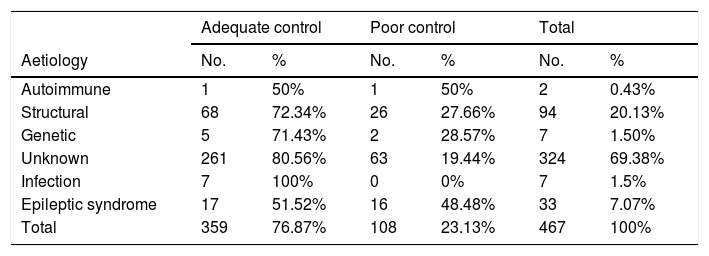
Nearly 90% of patients (422) showed adequate treatment adherence. Epilepsy was adequately controlled in 359 patients (76.8%) and poorly controlled in 108 (23.1%). By aetiology, seizure freedom was achieved in all cases of infectious origin, 80.5% of cases with unknown aetiology, 72.3% of patients with structural lesions, 71.4% of patients with genetic causes, 50% of cases of autoimmune epilepsy, and 52.5% of patients with epileptic syndromes (Table 2). Epilepsy was refractory in 32 patients (6.8%).
Seizure control by epilepsy aetiology.
| Adequate control | Poor control | Total | ||||
|---|---|---|---|---|---|---|
| Aetiology | No. | % | No. | % | No. | % |
| Autoimmune | 1 | 50% | 1 | 50% | 2 | 0.43% |
| Structural | 68 | 72.34% | 26 | 27.66% | 94 | 20.13% |
| Genetic | 5 | 71.43% | 2 | 28.57% | 7 | 1.50% |
| Unknown | 261 | 80.56% | 63 | 19.44% | 324 | 69.38% |
| Infection | 7 | 100% | 0 | 0% | 7 | 1.5% |
| Epileptic syndrome | 17 | 51.52% | 16 | 48.48% | 33 | 7.07% |
| Total | 359 | 76.87% | 108 | 23.13% | 467 | 100% |
Regarding the number of antiepileptic drugs (AED) used, 351 patients (75%) were receiving monotherapy, 84 (18%) were receiving 2 drugs, and 32 patients (6.8%) were receiving 3 or more AEDs (Table 3). By seizure type, 190 of the 253 patients with focal seizures were receiving monotherapy (75%), 44 were receiving 2 AEDs (17%), and 19 were receiving 3 or more AEDs (7.5%), whereas 161 of the 214 patients with generalised seizures were receiving monotherapy (75.2%), 40 were receiving 2 AEDs (18.6%), and 13 were receiving 3 or more AEDs (6%).
The AED most frequently used in monotherapy in our sample was magnesium valproate (MVP; 225 patients [64.2%]), followed by carbamazepine (CBZ; 54 [15.4%]), levetiracetam (LEV; 44 [12.5%]), and other AEDs (28 patients [8%]), including phenobarbital (PB), topiramate (TPM), and vigabatrin (VBT). In the patients receiving 2 AEDs, the most frequent drug combinations were MVP + LEV (24 patients [28.5%]), MVP + TPM (19 [22.6%]), and LEV + CBZ (6 [7.14%]); 35 patients received other drug combinations. In the group of patients with focal seizures, the AED most frequently administered in monotherapy was MVP (113 patients [59.4%]), followed by CBZ (41 [21.5%]), and LEV (22 [11.5%]); 14 patients (7.3%) were receiving other AEDs. In the group of patients with generalised seizures, the AED most frequently administered in monotherapy was MVP (113 patients [70.1%]), followed by LEV (22 [13.6%]) and CBZ (13 [8%]); 13 patients (8%) were receiving other AEDs.
Of the 351 patients receiving treatment in monotherapy, seizures were adequately controlled in 301 and were poorly controlled in 50 (85% vs 14.2%). Of the 84 patients receiving 2 AEDs, 50 presented adequate seizure control and 34 presented poor seizure control (59.5% vs 40.4%), and of the 32 patients receiving 3 or more AEDs, seizure control was adequate in 8 and poor in 24 (25% vs 75%) (Table 3).
Regarding comorbidities, 158 presented 1 comorbidity (33.8%), 19 patients presented 2 comorbidities (4%), and 290 patients presented no comorbidities (62%). Our patients presented the following comorbidities: neurodevelopmental disorders (107 patients [22.9%]), neurological diseases (31 [6.64%]), cerebral palsy (21 [4.5%]), endocrine disorders (11 [2.36%]), autoimmune diseases (2 [0.43%]), heart diseases (2 [0.43%]), psychiatric disorders (10 [2.14%]), genetic syndromes (5 [1%]), and other conditions (4 [0.86%]) (Table 4).
Comorbidities in our sample.
| Comorbidities | No. | % |
|---|---|---|
| Neurodevelopmental disorders | 107 | 22.91% |
| Autoimmune disorders | 2 | 0.43% |
| Heart diseases | 2 | 0.43 |
| Endocrine disorders | 11 | 2.36% |
| Neurological diseases | 31 | 6.64% |
| Psychiatric disorders | 10 | 2.14% |
| Cerebral palsy | 21 | 4.50% |
| Genetic disorders | 5 | 1.07% |
| Other | 4 | 0.86% |
| None | 290 | 62.10% |
We recorded a total of 1813 remote consultations, with a mean of 3.88 consultations per patient (range, 1–29). We calculated patient transfer costs saved according to data provided by the healthcare department of the state of San Luis Potosí (Table 1). In the Altiplano area, a total of 399 consultations were held, with a mean cost per consultation of 1825 Mexican pesos, which amounts to a total of 728,175 pesos saved. In the Media area, with 430 consultations and a mean transportation cost of 2020 pesos, telemedicine saved a total of 868,600 pesos. In the Huasteca area, 984 consultations were held, with a mean cost of 5200 pesos per consultation, which amounts to a total of 5,116,800 pesos saved. The total saving for all 3 areas was 6,713,575 pesos.
DiscussionTelemedicine is increasingly used in the follow-up of patients with a wide range of diseases; neurology was a pioneering field in the use of telemedicine for the treatment of numerous conditions, including epilepsy.3,4 Epilepsy has an incidence of 0.5%–2% worldwide. It is one of the most frequent neurological disorders managed at paediatric neurology departments; adequate diagnosis and treatment of epilepsy are essential to improve these children's quality of life.14
Different studies into the epidemiology of epilepsy report a higher incidence and prevalence in men, with some exceptions, including juvenile myoclonic epilepsy and generalised absence seizures. Sex-related differences in seizure type may be explained by the influence of such hormones as oestrogen, progesterone, and androgens in neurodevelopment, neuroprotection, memory, and seizures.15 Our results are consistent with those reported in the literature, as 61.4% of our sample were boys and 38.5% were girls.
In our study, 54.1% of seizures were focal and 45.8% were generalised. Haddad et al.16 analysed epidemiological variables in adults with epilepsy attended at telemedicine consultations and also found a higher percentage of patients with focal seizures (62.5%, vs 29% with generalised seizures). According to the literature, the most common aetiology of epilepsy is unknown causes, in up to 70% of cases17; this was also the case in our sample, with 69.8% of patients presenting epilepsy of unknown origin, followed by structural lesions, in 20.1%.
Regarding pharmacological treatment, the ILAE recommends that treatment should aim to achieve complete seizure freedom; this is accomplished in approximately 70% of cases, although seizures persist in up to 20% of patients despite the administration of one or more AEDs.18 In the study by Haddad et al.,16 two-thirds of patients were seizure-free at the last consultation. Similarly, 76.8% of our patients achieved seizure freedom (Z = 3.01; P = .003). By seizure type, most patients with adequately controlled epilepsy in our study had focal seizures (56.8%, vs 43.1% with generalised seizures; P = .04). This finding stands in contrast with the literature, as focal seizures tend to be treatment-resistant due to possible structural causes.17,19 In our sample, the aetiology most frequently associated with successful seizure control was infection, with 100% of these patients achieving seizure control, followed by unknown (80%), structural (72%), genetic (71%), and autoimmune causes (50%); among patients with epileptic syndromes, seizure control was achieved in 52% of cases. These differences were statistically significant (P = .001). According to the literature, patients with epilepsy of unknown aetiology respond best to treatment. Some epilepsies, for example epileptic syndromes, present biological refractoriness; these patients have poorer prognosis in terms of seizure control, cognitive development, and social skills. This in consistent with our results, as a lower percentage of this group of patients presented adequate seizure control. Such conditions as mesial temporal sclerosis and cortical dysplasia cause drug-resistant epilepsy17,19; however, in our sample, a higher percentage of patients with epilepsy of structural causes achieved adequate seizure control than the percentage reported by the ILAE (70%).
At present, numerous drugs have been approved for the treatment of epilepsy; pharmacological treatment must be established based on such specific variables as age, seizure type, and whether the patient has a specific epileptic syndrome. CBZ and oxcarbazepine (OXC) are considered first-line treatments for focal seizures and complementary treatments for generalised tonic–clonic seizures (GTCS).18,20 A meta-analysis of paediatric patients showed that CBZ and MVP were equally effective for treating focal seizures and GTCS.21 According to the available evidence on the efficacy and effectiveness of AEDs, only CBZ, PB, phenytoin, TPM, and MVP are efficacious for the treatment of focal seizures in children.22 MVP is considered a first-line treatment for generalised seizures and is one of the most frequently indicated AEDs for patients with epileptic syndromes associated with a high risk of GTCS, such as juvenile absence epilepsy.21,22 In our study, the AED most frequently used in monotherapy for focal seizures was MVP (60%), followed by CBZ (21%), and LEV (12%); 7% of patients used other AEDs in monotherapy. According to the literature, MVP and CBZ are the 2 AEDs most frequently prescribed for focal seizures. Regarding generalised seizures, the AED most frequently used in monotherapy was MVP (70%), followed by LEV (14%) and CBZ (8%); 8% of patients were receiving other AEDs. Again, MVP and LEV are also the 2 AEDs most frequently prescribed for generalised seizures in the literature.20–22
It is well known that approximately 25% of patients do not respond to monotherapy and require a combination of 2 or more AEDs to control seizures. Furthermore, 20%–30% of patients are refractory despite receiving adequate combination therapy.23 In the study by Haddad et al.,16 62.5% of patients were receiving at least 2 AEDs; in our study, in contrast, 75% of patients were receiving 1 AED, 18% were receiving 2 AEDs, and 7% were receiving 3 or more AEDs. In the subgroup of patients achieving adequate seizure control, 83% were receiving one AED, 14% were receiving 2 AEDs, and 3% were receiving 3 or more AEDs (P = 1.02 × 10−17). Furthermore, 75% of patients with focal seizures achieved seizure control with only one AED, 17% with 2 AEDs, and 7.5% with 3 or more AEDs; similar results were observed in the group of patients with generalised seizures (75%, 18%, and 6%, respectively), with no statistically significant differences. The drug most frequently used in monotherapy was MVP (64.2%), and the most frequent combination of 2 drugs was MVP + LEV (28.57%).
In our programme, 81 patients (17%) were discharged due to remission of epilepsy; of these, 89% had epilepsy of unknown aetiology, 10% had epilepsy of structural aetiology, and 1% had epilepsy of genetic aetiology. No studies have provided information on this point. A total of 187 patients (40%) were lost to follow-up; 127 of these (68%) presented adequate seizure control until their last consultation, whereas the remaining 60 (32%) had not achieved seizure control. The reasons that patients were lost to follow-up through the telemedicine service were changes in the type of healthcare system (37 patients), change of residence to a different state (5 patients), and the closure of 3 telemedicine centres, with 19 patients continuing with medical care directly at our hospital. Our study did not analyse patient satisfaction with the telemedicine programme, although other studies report that over 70% of patients preferred remote consultations as telemedicine enables more regular follow-up, the care provided was satisfactory, and they did not have to travel to another town or city to receive care.24–29 Rodríguez et al.30 evaluated the satisfaction of specialists, in this case neurologists, with telemedicine and found that they supported the use of this technology for the treatment and follow-up of neurological patients.
In our study, and in line with the literature, 38% of patients presented comorbidities.31,32 The most frequent were neurodevelopmental disorders, in 23% of patients. The patients who were evaluated by the psychology, psychiatry, or rehabilitation departments were referred to centres in their communities, or attended through teleconsultations when these specialists or subspecialists were not available.
Although cost savings vary between patients (cost of transportation, loss of productivity for one or two individuals, food, accommodation if necessary), analysing the economic impact of telemedicine is essential. A total of 1813 consultations were held through our programme, resulting in significant cost savings both for the healthcare system and for patients and their families.
During the COVID-19 pandemic, physical distancing has been one of the measures implemented to reduce the spread of the virus. In this context, telemedicine has played a pivotal role in the design of new healthcare policies, with online consultations preventing the saturation of healthcare services and the need for patients to travel to these centres.33,34 Several countries have established telemedicine networks for the follow-up of patients with SARS-CoV-2 infection, enabling the detection of patients who need to be transferred to a hospital to continue treatment. Since then, telemedicine has been used not only in patients with COVID-19 but also in such other fields as urology, ophthalmology, and chronic diseases requiring long-term treatment, including oncohaematological, systemic, dermatological, and neurological conditions.29,35–37 During the pandemic, our telemedicine network enabled the continuation of treatment for neurological patients, with only those patients requiring hospital admission or assessment and treatment at reference hospitals being transferred to these centres.
ConclusionsOur telemedicine network is a useful alternative for providing care to patients with epilepsy, as it was associated with similar effectiveness to in-person consultations; seizure control and treatment adherence were even higher than reported in previous studies.
Furthermore, the programme involves significant cost savings for families and for the healthcare system due to the decrease in the number of in-person consultations held at our hospital. In the future, telemedicine may be used in the evaluation of electroencephalography and neuroimaging study results, which would contribute to a further decrease in hospital transfers. During the pandemic, telemedicine has enabled the follow-up of patients with epilepsy; this tool should therefore be used in many other fields of medicine. Patient satisfaction with telemedicine should be evaluated with a view to improving care quality.
FundingThis study has received no specific funding from any public, commercial, or non-profit organisation.
Conflicts of interestNone.