The benefit of preventive measures and of acute treatment for ischaemic stroke relies on knowledge of the disease among the general population. The aim of this study was to evaluate the knowledge of ischaemic stroke in a school community in Bogota (Colombia).
MethodsWe conducted a descriptive cross-sectional cohort study using an online survey that was sent to the members of the school community. The survey gathered sociodemographic data and enquired about respondents’ knowledge of ischaemic stroke.
ResultsWe received 146 completed surveys. Of all respondents, 72% were pupils’ parents, 20.3% teachers, and 7.5% administrative staff. All respondents resided in urban areas, and 82.2% had a high socioeconomic level. The most frequently mentioned risk factors for ischaemic stroke were stress (28.9%), sedentary lifestyles (23.9%), diet (23.3%), arterial hypertension (20.5%), and smoking (14.4%). A total of 8.9% of respondents did not name any risk factor. The most frequently mentioned symptoms of stroke were headache (26%), motor impairment (19.9%), language impairment (15%), vertigo (12.3%), and altered level of consciousness (10.3%). Regarding stroke management times, 87.7% of respondents selected up to 6 h after onset as the optimal time window to seek medical assistance; 86.1% said they did not know which hospital to go to in the event of an ischaemic stroke, and only 2.7% of respondents indicated intravenous thrombolysis as a therapeutic option available in Colombia.
ConclusionKnowledge about ischaemic stroke in this population was poor. Public stroke education campaigns are needed in this community.
El beneficio de las medidas de prevención y de la terapia aguda del infarto cerebral dependen del conocimiento de la población acerca de la enfermedad. El objetivo de este estudio fue evaluar el conocimiento sobre el infarto cerebral en una comunidad educativa, de Bogotá, Colombia.
MétodosFue un estudio descriptivo de cohorte transversal tipo encuesta enviada a los integrantes de una comunidad educativa, la cual incluía: datos sociodemográficos y preguntas acerca del conocimiento del infarto cerebral.
ResultadosSe obtuvieron 146 encuestas diligenciadas. El 72% de los encuestados fueron padres de familia, 20,3% profesores y 7,5% trabajadores del centro educativo. Todos residen en zonas urbanas y el 82,2% pertenecen a estratos socioeconómicos altos. Los factores de riesgo para infarto cerebral descrito con mayor frecuencia fueron: estrés (28.9%), sedentarismo (23,9%), dieta (23,3%), hipertensión arterial (20,5%) y tabaquismo (14,4%). El 8,9% no identificaron factores de riesgo. Los síntomas de infarto cerebral descritos con mayor frecuencia fueron: cefalea (26%), compromiso motor (19,9%), alteración del lenguaje (15%), vértigo (12,3%) y alteración de la conciencia (10,3%). El 87,7% de los encuestados seleccionó la opción de acudir a urgencias en las primeras 6 horas después del inicio de los síntomas. El 86,1% manifestó no saber a qué centro hospitalario dirigirse en caso de un infarto cerebral y el 2,7% de los encuestados señalo la trombólisis intravenosa como opción terapéutica.
ConclusiónEl conocimiento acerca del infarto cerebral en esta población es escaso. La implementación de campañas masivas de educación sobre infarto cerebral para la comunidad es necesaria.
Ischaemic stroke is the most frequent form of cerebrovascular disease, the leading cause of disability in older adults, and the second leading cause of death in Colombia, and is associated with significant social, economic, and family costs.1 Most strokes are preventable and are associated with known risk factors.2,3 Furthermore, scientific, pharmacological, and technological advances made in the last 25 years have led to a paradigm shift in the treatment of ischaemic stroke, reducing mortality rates and disability in the long term.2,4 However, successful prevention and acute treatment of ischaemic stroke require understanding of the subject in the community.
The majority of the global population does not recognise the symptoms and risk factors of ischaemic stroke.5,6,7Moreover they are also unaware of management times for optimal treatment, which hospital to travel to, or how to activate the local emergency system to ensure eligibility for cerebral reperfusion treatment.5,6 Among Spanish speakers in Latin America, the small number of studies into knowledge about ischaemic stroke in the community have shown similar results.6 While the community may consult various sources for information on cerebrovascular disease, depending on certain demographic factors, studies show that most of this information is from non-medical sources.5,8,9 Finally, women interviewed about cerebrovascular disease reported that they did not understand and were not well-informed about the disease, and did not perceive cerebrovascular disease as a cause of death.9,10
The first step in implementing public health information strategies is to establish the current understanding of ischaemic stroke. This information will facilitate the development of specific education programmes adjusted to the needs of the community in order to strengthen, modify, and expand understanding of the disease, improving the efficacy of prevention and treatment interventions.
The aim of this study was to evaluate the knowledge about ischaemic stroke in a school community in Bogota (Colombia), in the healthcare district served by the hospitals at which the authors work.
MethodsStudy design and populationWe conducted a descriptive, cross-sectional cohort study using a survey to determine the level of knowledge about ischaemic stroke in a school community. The survey was designed by the authors and reviewed and corrected by a sociologist with knowledge of linguistics.
The survey comprised three sections. The first included a description of the study and explained that participation was voluntary. The second collected sociodemographic data: age, sex, role in the school community (staff, pupil, parent), place of residence, and socioeconomic stratum for public services (nominal classification from 1 to 6, with 6 being the highest). The third section included five questions on knowledge about ischaemic stroke: two closed questions, two open-ended questions, and one semi-closed question. Questions enquired about risk factors, symptoms, and treatment of ischaemic stroke (see appendix: Table 1). The survey was hosted on the Google Drive platform. The study population was the community of a private school (primary and secondary education) in north-eastern Bogota, with a database including 900 individuals (staff, pupils, and parents). The survey was distributed by e-mail to all community members older than 18 years. Data were collected between 15 February and 1 March 2017.
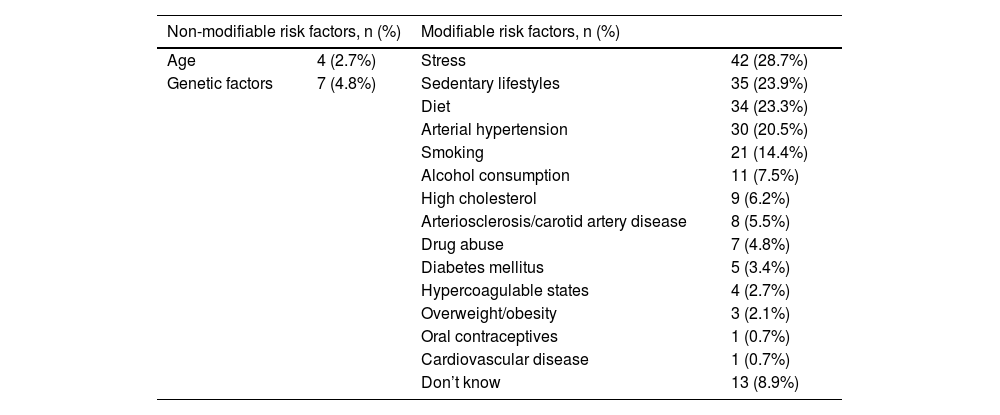
Risk factors for ischaemic stroke, according to 146 survey responses from members of a school community in Bogota, Colombia (2017).
| Non-modifiable risk factors, n (%) | Modifiable risk factors, n (%) | ||
|---|---|---|---|
| Age | 4 (2.7%) | Stress | 42 (28.7%) |
| Genetic factors | 7 (4.8%) | Sedentary lifestyles | 35 (23.9%) |
| Diet | 34 (23.3%) | ||
| Arterial hypertension | 30 (20.5%) | ||
| Smoking | 21 (14.4%) | ||
| Alcohol consumption | 11 (7.5%) | ||
| High cholesterol | 9 (6.2%) | ||
| Arteriosclerosis/carotid artery disease | 8 (5.5%) | ||
| Drug abuse | 7 (4.8%) | ||
| Diabetes mellitus | 5 (3.4%) | ||
| Hypercoagulable states | 4 (2.7%) | ||
| Overweight/obesity | 3 (2.1%) | ||
| Oral contraceptives | 1 (0.7%) | ||
| Cardiovascular disease | 1 (0.7%) | ||
| Don’t know | 13 (8.9%) | ||
To analyse responses to the open-ended questions, addressing risk factors and symptoms of ischaemic stroke, the authors read all the responses, interpreted them semiologically, and categorised them according to common terms. In the descriptive analysis, qualitative data are expressed as absolute frequencies and percentages. Quantitative variables following a normal distribution are expressed as means and standard deviations (SD). Missing data were not imputed.
Ethics approvalThe study was conducted in accordance with the applicable Colombian legislation regarding healthcare research (Resolution 8430 of 1993 and Law 23 of 1981). As this is a non-interventional study with no associated risk, informed consent was not required (Resolution 8430 of 1993). The study was approved by our centre’s research and ethics committee. The authors certify the veracity and accuracy of the information reported, and have no conflicts of interest to declare.
ResultsSociodemographic characteristicsWe received a total of 146 responses during the study period. The mean time taken to complete the questionnaire was 8.5 (SD+/-1.5) min. Respondents’ mean age was 40 (SD+/-10) years, and 68.3% (n = 99) of respondents were women . Parents of pupils accounted for 72% (n = 103),of responses teachers for 20.3% (n = 29), and administrative staff for 7.5% (n = 11). All respondents lived in urban areas, with 80% (n = 116) residing in Bogota. The great majority ( 79.5%, n=92) lived in the areas of Usaquén and Chapinero in Bogota; these areas are served by the hospitals at which the authors work. According to the public services stratification system, 40.1% (n = 57) lived in stratum 6 areas, 23.2% (n = 33) in stratum 5, 21.1% (n = 30) in stratum 4, 10.6% (n = 15) in stratum 3, 4.2% (n = 6) in stratum 2, and 1 individual in stratum 1.
Stroke risk factorsThe risk factors mentioned by respondents, grouped into modifiable and non-modifiable factors, are presented in Table 1. Thirteen respondents (8.9%) did not know any risk factors for ischaemic stroke. With regard to non-conventional or uncommon risk factors, stress was the most frequently mentioned (28.7%). Among the conventional (common) risk factors mentioned, sedentary lifestyles (23.9%), diet (23.3%), arterial hypertension (20.5%), and smoking (14.4%) were most frequent. One individual was able to list five risk factors for ischaemic stroke.
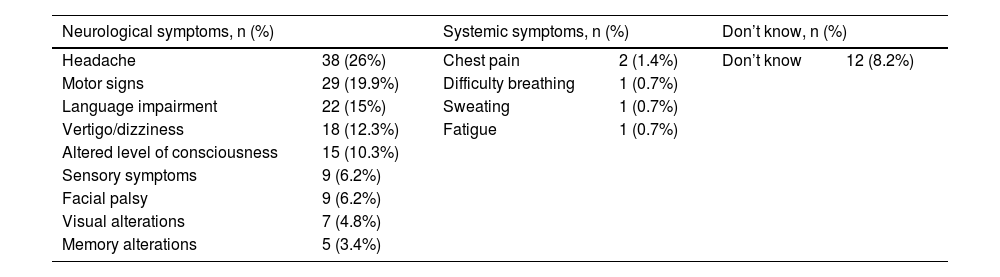
Symptoms of ischaemic strokeThe symptoms mentioned by respondents, which were analysed and classified by the authors as neurological or systemic symptoms, are presented in Table 2. Headache was mentioned by 26% of respondents, motor signs by 19.9%, and language alterations by 15%. Twelve respondents (8.2%) did not know any symptom of ischaemic stroke.
Symptoms of ischaemic stroke, according to 146 survey responses from members of a school community in Bogota, Colombia (2017).
| Neurological symptoms, n (%) | Systemic symptoms, n (%) | Don’t know, n (%) | |||
|---|---|---|---|---|---|
| Headache | 38 (26%) | Chest pain | 2 (1.4%) | Don’t know | 12 (8.2%) |
| Motor signs | 29 (19.9%) | Difficulty breathing | 1 (0.7%) | ||
| Language impairment | 22 (15%) | Sweating | 1 (0.7%) | ||
| Vertigo/dizziness | 18 (12.3%) | Fatigue | 1 (0.7%) | ||
| Altered level of consciousness | 15 (10.3%) | ||||
| Sensory symptoms | 9 (6.2%) | ||||
| Facial palsy | 9 (6.2%) | ||||
| Visual alterations | 7 (4.8%) | ||||
| Memory alterations | 5 (3.4%) | ||||
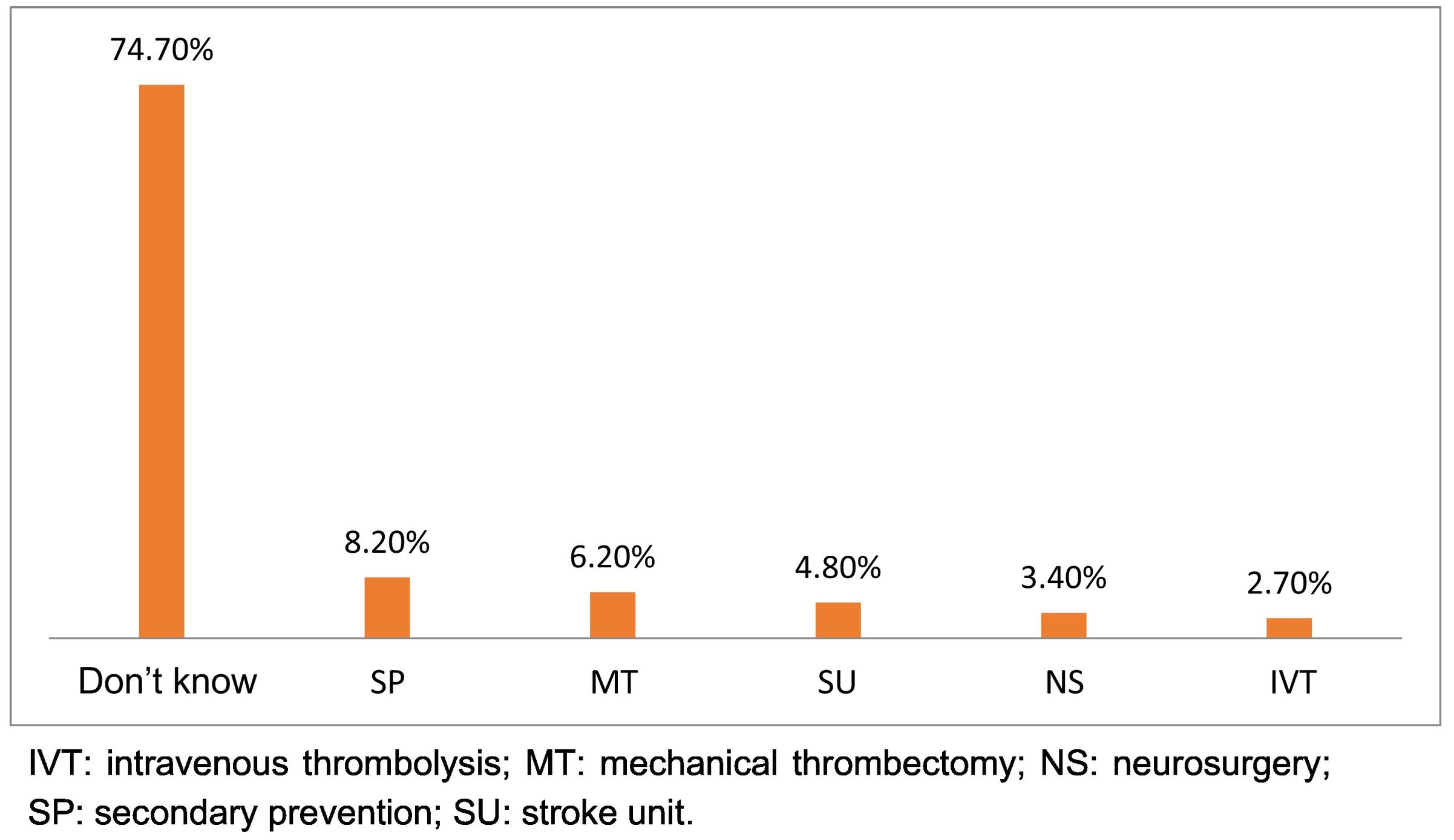
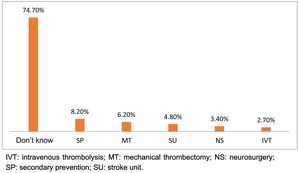
All respondents knew that medical attention should be sought in the event of a stroke. A total of 87.7% (n = 128) responded that attention should be sought in the first 6 h after symptom onset, with 13.9% knowing which centre to attend. Regarding treatments for ischaemic stroke, 74.7% of respondents did not know which treatments were available in Colombia. Secondary prevention was selected by 8.2% (n=12) of respondents , mechanical thrombectomy by 6.2% (n = 9), stroke units by 4.8% (n = 7), neurosurgical procedures by 3.4% (n = 5), and intravenous thrombolysis by 2.7% (n = 4) (Fig. 1).
DiscussionSurvey respondents from this school community in Bogota displayed poor knowledge of the risk factors, symptoms, and treatments available for ischaemic stroke. Despite living in an urban setting (100%) and their young age (40 years) and high socioeconomic level (82.2% were residents of stratum 4, 5, or 6 areas), the percentage of respondents who knew any particular symptom or risk factor for ischaemic stroke never surpassed 30%. Furthermore, 74.7% of respondents did not know what treatments for ischaemic stroke were available in Colombia. While all respondents recognised the need to seek medical attention in the event of stroke, with most selecting the first 6 h after onset as the optimal time, most did not know which hospital to attend.
It is noteworthy that stress (a non-conventional or uncommon risk factor for ischaemic stroke) was mentioned so frequently (28.7%), as reported in other studies.11,12 The 10 conventional or common risk factors, associated with 80% of ischaemic strokes, were mentioned by a low percentage of respondents. Despite 91.1% of respondents mentioning at least one risk factor, only one individual was able to list five, and cardiac or cardiovascular disease was only mentioned by one respondent. According to previous studies, 45%–85% of the population knows at least one risk factor.12–14 In the Spanish-speaking population, the most frequently recognised risk factor is arterial hypertension, followed by alcohol consumption and smoking. On the contrary, older age, diabetes mellitus, dyslipidaemia, and heart disease are less well-recognised as risk factors for ischaemic stroke.11 Studies show very heterogeneous levels of knowledge of the risk factors for ischaemic stroke in the community, although they consistently find that very few individuals are able to identify the majority of conventional (common) known risk factors.
While headache only presents in approximately 30% of cases, it was identified by our respondents as a symptom of stroke, as in previous studies.5,10 Other Colombian studies have found that 65%–70% of individuals surveyed do not know the symptoms of ischaemic stroke.8,13 Motor and language symptoms, which present high sensitivity and moderate specificity for recognising stroke, were only mentioned by 10%–20% of respondents. It is also noteworthy that the presence of such systemic symptoms as chest pain is often identified as a symptom of ischaemic stroke.5,11 The poor knowledge of risk factors and symptoms of ischaemic stroke may constitute an obstacle to the implementation of prevention and treatment interventions.
Finally, regarding the treatment of stroke, which was the focus in the last three questions of the survey, all respondents recognised the need to seek medical attention. The majority believed that attention should be sought in the first 6 h after onset, but few respondents (13.9%) knew which hospital to attend. Previous studies report heterogeneous results, with 24%–63% of individuals surveyed knowing that the treatment of ischaemic stroke is time-dependent.5,11 Our survey did not address responses to transient neurological symptoms. However, previous studies have evaluated behaviour in the event of transient symptoms, finding that 13.7%–56.9% of respondents would attend the emergency department on the day that symptoms present.11 In contrast, a study conducted in Colombia in 2011 found that 88% of respondents would not take appropriate action if they presented stroke.13
Most respondents (74.7%) did not know what types of treatment were available for ischaemic stroke in Colombia. Only 8.9% selected cerebral reperfusion measures (6.2% for mechanical thrombectomy and 2.7% for intravenous thrombolysis) as a therapeutic option to treat ischaemic stroke. This is consistent with the results of two previous studies conducted in Colombia: Díaz-Cabezas8 reports that only 1.4% of Colombian survey respondents knew about the existence of thrombolytic treatments.
The strengths and limitations of our study are related to the study population and design. Survey respondents resided in the healthcare district served by the hospitals at which the authors work. The findings will facilitate the creation of targeted, specific public information strategies. We consider the sample size sufficient to ensure reliable results. Finally, the survey was easy to complete and to understand, and the open-ended items did not include leading questions.
The study is not free of limitations. For example, respondents were selected by convenience sampling, and the socioeconomic level of the study population was high (although level of education was not recorded). The survey was only distributed to one school community. The survey focused on ischaemic stroke, but did not address all aspects; likewise, haemorrhagic stroke was not addressed. Furthermore, due to limited resources, the survey was not externally validated, no public information intervention was implemented in the study population, and we have not evaluated changes in knowledge of ischaemic stroke since the survey was conducted (2017).
As in previous studies conducted in the region, our study population showed a poor level of knowledge of various aspects of stroke. Our results underscore the need for public health education strategies to improve knowledge of the risk factors, cardinal symptoms, and available treatments for ischaemic stroke, and to identify the hospitals equipped to treat the disease.
ConclusionsRespondents displayed poor knowledge of the risk factors, symptoms, and available treatments for ischaemic stroke. As the efficacy of prevention and reperfusion interventions for ischaemic stroke depends on this knowledge, it is important to dedicate resources to determining public understanding of the disease in order to implement specific information campaigns adjusted to the needs of each community.
Conflicts of interestThe authors have no conflicts of interest to declare.
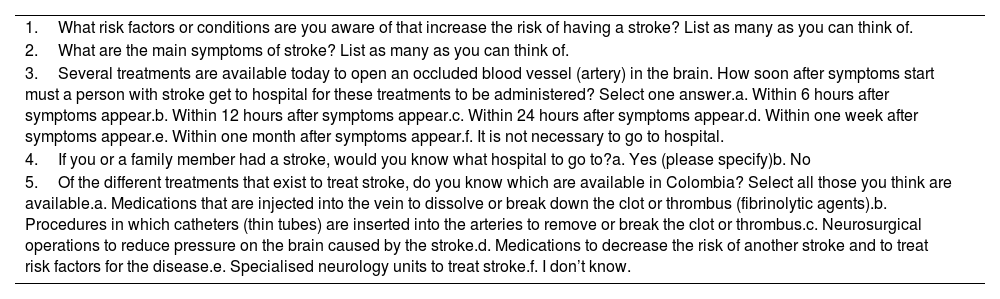
Questions on public knowledge of cerebrovascular disease (risk factors, symptoms, and treatment).
| 1.What risk factors or conditions are you aware of that increase the risk of having a stroke? List as many as you can think of. |
| 2.What are the main symptoms of stroke? List as many as you can think of. |
| 3.Several treatments are available today to open an occluded blood vessel (artery) in the brain. How soon after symptoms start must a person with stroke get to hospital for these treatments to be administered? Select one answer.a. Within 6 hours after symptoms appear.b. Within 12 hours after symptoms appear.c. Within 24 hours after symptoms appear.d. Within one week after symptoms appear.e. Within one month after symptoms appear.f. It is not necessary to go to hospital. |
| 4.If you or a family member had a stroke, would you know what hospital to go to?a. Yes (please specify)b. No |
| 5.Of the different treatments that exist to treat stroke, do you know which are available in Colombia? Select all those you think are available.a. Medications that are injected into the vein to dissolve or break down the clot or thrombus (fibrinolytic agents).b. Procedures in which catheters (thin tubes) are inserted into the arteries to remove or break the clot or thrombus.c. Neurosurgical operations to reduce pressure on the brain caused by the stroke.d. Medications to decrease the risk of another stroke and to treat risk factors for the disease.e. Specialised neurology units to treat stroke.f. I don’t know. |