To explore and understand the experiences of the patients with severe asthma throughout their patient journey.
DesignQualitative ethnographic study based on an ethnographic approach.
LocationBarcelona, Sevilla and Madrid.
Participants and contextTen adult (>18 years) persons (six females and four males) diagnosed with severe asthma were selected from public healthcare settings by purposive sampling.
MethodSemi-structured in-depth interviews performed by an expert anthropologist in the patients’ homes. Data was collected using a video and audio recorder and analyzed by three researchers using the sense-making methodology.
ResultsLife experiences were classified into four main areas: life experiences throughout the patient journey, attitudes towards the disease and healthcare professionals, unmet needs regarding knowledge and self-management, and relationship with doctors and healthcare providers. Within each area, several topics and subtopics emerged, allowing to distinguish three initial phases of the disease and three attitudinal profiles.
ConclusionsDuring the initial phases of severe asthma, participants underestimated its severity and symptoms, resulting in disease denial and passivity. Participants associated disease severity with chronicity, which was internalized years after its diagnosis, delaying patients’ adaptation to the disease and their ability of to self-manage it. Participants noticed gaps in health-related information and communication and needed a comprehensive understanding of their disease from the beginning.
Explorar y comprender las experiencias de los pacientes con diagnóstico de asma grave a lo largo de su enfermedad.
DiseñoEstudio cualitativo basado en una aproximación etnográfica.
EmplazamientoBarcelona, Sevilla y Madrid.
Participantes y contextoDiez personas adultas (>18 años) (6 mujeres y 4 varones) diagnosticadas con asma grave fueron seleccionadas del sistema de salud público mediante muestreo intencionado.
MétodoEntrevista en profundidad, semiestructurada, realizada por un antropólogo experto en los domicilios de los pacientes. Los datos fueron recogidos mediante grabación de audio y vídeo, analizados por 3 investigadores mediante la metodología sense making.
ResultadosLas vivencias se clasificaron en 4 áreas principales: vivencias durante el patient journey, actitudes frente a la enfermedad y los profesionales de la salud, necesidades no cubiertas respecto al conocimiento y gestión de la enfermedad y relación con los médicos y los profesionales de la salud. En cada área surgieron diversos temas y subtemas que permitieron identificar 3 fases entre las vivencias iniciales y 3 perfiles actitudinales.
ConclusionesDurante las fases iniciales del emotional patient journey, los participantes infravaloraron la gravedad y síntomas de su enfermedad, actitud que condujo a su negación y pasividad. Los participantes asociaron gravedad de la enfermedad con cronicidad, la cual es internalizada años después del diagnóstico, retrasando la adaptación del paciente a la enfermedad y su habilidad para gestionarla. Los participantes detectaron lagunas en la información relacionada con la salud y la comunicación, y manifestaron la necesidad de tener una visión global de su enfermedad desde el principio.
- •
Asthma is a chronic disease that causes a severe emotional burden to patients and, if uncontrolled, can increase its severity and the risk of exacerbations.
- •
A number of factors associated with diagnosis and management, including those of psychosocial nature, influence patient care.
- •
A good relationship between patients and healthcare professionals, together with patient education, are considered essential to achieve an effective management of asthma.
- •
Patients with severe asthma underestimated their disease severity and showed an attitude of alienation and passivity, especially during the initial phases of the disease.
- •
Participants associated disease severity with chronicity, which was internalized years after its diagnosis, resulting in delayed adaptation of their lifestyle to living with asthma.
- •
Once patients became aware of their severe asthma, they acknowledged the need of more disease-related education and better communication with healthcare providers from the beginning.
Asthma is a chronic heterogeneous condition that constitutes a severe public health problem worldwide.1 Inhaled or systemic corticosteroids are the conventional treatment to control asthma symptoms with the ultimate goal of reducing the risk of exacerbations, which often require hospitalization.2,3 An estimated 3–15% of asthma patients have severe asthma (SA), a distinct form of the disease characterized by the lack of response to these treatments or the need of very high doses to achieve disease control.4,5 Asthma symptoms limit patients’ daily activities, and long-term oral corticosteroid (OCS) treatment causes severe side effects, both resulting in an emotional burden that strongly affects patients’ quality of life, often in an undisclosed way.2,6–10
In addition to the emotional distress, a number of factors associated with disease diagnosis and management that affect quality of care have been identified. The diagnosis of asthma and its different subtypes is challenged by factors that make patients appear to have poor control of their asthma (i.e., significant comorbidities, and poor compliance with medication and improper inhaler technique) as well as the fluctuating pattern of asthma severity. Thus, despite the efforts to propose a uniform definition and assessment in clinical guidelines, asthma is often misdiagnosed, delaying referral to the specialist.1,4,11–13
Currently, the cornerstone of an effective asthma management includes maintaining adequate symptom control and avoiding exacerbations to reduce lung function impairment and adverse events of chronic OCS use.1,14 These goals are unlikely to be achieved without good communication between the patient and the healthcare professional that enables patients to gain the knowledge, confidence, and skills for self-management of the disease.1 In this regard, patient education has been associated with improved lung function and reduced frequency of asthma symptoms, whereas poor health-related literacy has been associated with greater mortality and morbidity of asthma patients.15,16
In addition to the role of disease self-management in health outcomes, other psychosocial factors, such as health beliefs, may influence effective asthma management and control.17 However, due to the insufficiency of studies focused on the life experiences of asthma patients, a global understanding of their own perception and their attitudes towards the disease is still missing.9,18 This qualitative ethnographic study aims at understanding the life experiences of patients with SA and their evolution throughout their patient journey, including their communication and interaction with specialists.
Participants and methodsStudy designThis was a qualitative study including adult (>18 years) patients diagnosed with SA. To obtain detailed accounts of the patients’ point of view of their journey with SA and to capture and understand their beliefs and attitudes towards their disease, we used ethnographic interviews. This technique consists in a face-to-face, contextualized, and in-depth interview conducted at the participants’ homes. In addition to the data obtained from conversation, this technique enables the researcher to obtain data from non-verbal language and observation of patients’ homes, allowing researchers to extract information from the subjective experiences of patients. Ethnographic methods understand reality from a phenomenological perspective, which focusses on comprehending the individual's life experiences or individual's subjectivity to acquire relevant knowledge.
Sample, participants and contextsPurposive sampling was used to recruit a representative sample of patients with SA from three cities from Spain: Barcelona, Sevilla and Madrid. Participants were initially screened by a short telephone interview to confirm their eligibility, and selected participants were scheduled for an ethnographic interview. A sample of 10 patients, balanced by gender, main asthma specialist (allergist or pulmonologist), treatment (biological or conventional), age segment (18–44, 45–64, and >65 years), and time since diagnosis (<1 year to >5 years) was deemed sufficient for data saturation and variability. Participants and those with relatives employed in an advertising agency, a market research company, or any newspaper, magazine, radio or TV; or that worked in a pharmaceutical or health-related company as clinicians, researchers, consultants or had any other role were excluded from the study.
All study participants participated voluntarily in the study and signed an informed consent and confidentiality agreement. The study was conducted in accordance with the Local Personal Data Protection Law (LOPD 15/1999) and the codes of conduct of the European Pharmaceutical Market Research Association (EphMRA).
Data collectionData was collected by a male consultant anthropologist with extensive expertise in performing ethnographic health studies. The ethnographer did not have any previous relationship with the patients and conducted a 2-h semi-structured interview at the participant's home. All the interviews were documented by the ethnographer using observation notes, audio and video recording, and photographs. The interview was divided into four blocks, including (1) patient and context (i.e., personal, familiar, and social); (2) perception of SA, its symptoms, and impact; (3) disease history and evolution, including first symptoms and diagnosis, management and expectations for the future; and (4) communication and relationship with the asthma specialist, expectations and needs. Block 1 aimed to understand the subjectivity of the patient and pave the way to establish a rapport for the rest of the interview, and block 2 aimed to obtain data regarding patients’ perspectives, beliefs and experiences related with severe asthma. During blocks 3 and 4 of the interview, participants were asked to complete two exercises. The first exercise, “Timeline”, consisted in identifying the different feelings experienced during disease evolution using a timeline ranging from before SA until the present and a panel of nouns describing feelings. The second exercise, “Role Playing”, consisted in adopting the role of an asthma specialist attending a SA patient to explore how patients would like to be cared for and to understand the most painful points of their experience. The rationale of these two exercises was to gain access to the patients’ feeling and wishes, which are more easily accessible through game-like exercises than direct questions. After the interview, the patient took the interviewer on a guided home tour, describing the different spaces and rooms, their uses, and the patient's opinion about them. During the home tour, the interviewer took photographs of the different spaces and asked questions related to the topics raised during the interview and later compared this information with that obtained during the interview. Additionally, throughout the interview, the ethnographer made note of the space, organization, and objects in the patient's home, the patient's appearance (outfit, accessories, self-care, posture), non-verbal communication, lack of correspondence between verbal answers and body language, use of electronic devices, and interaction with other persons present in the house.
Data processing and analysisInterviews were transcribed to provide a detailed record, which was complemented with the observation notes, photographs, and audio and video recordings. To eliminate any potential bias due to the potential subjective interpretation of the researcher, data were processed by three researchers. The different kinds of data obtained (i.e., verbal language, non-verbal language, and home observation) were triangulated to obtain a deep and comprehensive understanding of the phenomena.19,20 Data was interpreted using the sense-making methodology, an inductive analysis to identify patterns in the main topics to be studied from repeated and consistent evidence. The topics investigated in this study were life experiences (i.e., from occurrence of the first symptoms until diagnosis and prescription of first treatment), attitudes towards the disease and healthcare professionals, needs regarding disease knowledge and perception, and patients’ relationship and communication with doctors and healthcare providers, to ultimately confer a meaning to each of the experiences.21 Researchers iteratively re-examined data in order to validate and/or refine these themes and patterns. This iterative analysis helped to establish connections between different patients’ accounts, unveil robust patterns in their journey with SA, and assure the accuracy of the findings.
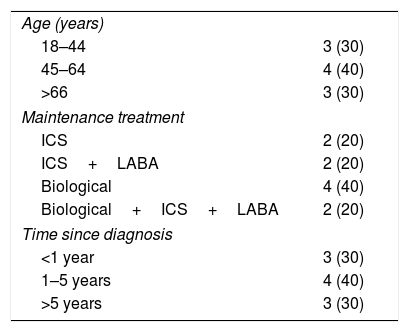
Results and discussionCharacteristics of study participantsThe study sample consisted of 10 patients, whose demographic, clinical and treatment characteristics are summarized in Table 1. Participating patients, of which six were female, were distributed in similar proportions among the three age and time-since-diagnosis segments.
Demographic and clinical characteristics of study participants; n (%)=10.
| Age (years) | |
| 18–44 | 3 (30) |
| 45–64 | 4 (40) |
| >66 | 3 (30) |
| Maintenance treatment | |
| ICS | 2 (20) |
| ICS+LABA | 2 (20) |
| Biological | 4 (40) |
| Biological+ICS+LABA | 2 (20) |
| Time since diagnosis | |
| <1 year | 3 (30) |
| 1–5 years | 4 (40) |
| >5 years | 3 (30) |
ICS: Inhaled corticosteroids; LABA: long-acting beta agonist.
The life experiences of patients with SA evolved throughout their journey. Three different phases were identified within initial life experiences (i.e., from occurrence of first symptoms until diagnosis and prescription of first treatment) (Table 2). In phase 1, patients noticed the occurrence of first symptoms but considered them anecdotal (i.e., due to stress and difficulty to sleep at night), normalizing their symptoms as a response to their fear of having a disease. In phase 2, symptoms progressively worsened, in most cases leading to the first crisis and subsequent diagnosis of asthma. In spite of the soothing effect of this finding, viewed as a mild condition, patients were traumatized and lived in fear of another asthma exacerbation, while remaining unaware of the impact that asthma could have in all aspects of their lives. After receiving the first successful treatment (Phase 3), patients progressively became unconcerned about follow-up visits and medical indications due to the reassuring effect of prescribed rescue medications and the perceived lack of severity of their asthma.
Main topics identified within initial life experiences of patients with severe asthma.
| Main topics | Quotes |
|---|---|
| Phase 1: First symptoms | |
| • Awareness that certain daily activities become unusually tiring• Awareness that small efforts induce symptoms• Normalization of symptoms | “Sometimes I had to run to catch the train and I turned purple and people always asked me, ‘Are you feeling ok?”’ 64, BCN“It must be a cold.” 36, BCN“I find it hard to climb the stairs.” 64, BCN“I think I have an allergy.” 32, SVL“I had to quit the game early because I was suffocating.” 38, BCN |
| Phase 2: Crisis and diagnosis | |
| • In shock after first crisis• Fear of another asthma attack• Lack of understanding of the impact of asthma | “I started wheezing and I suddenly felt I couldn’t breathe, I was suffocating.” 66, SVL“It started in the early morning, I was with my father and we didn’t know what to do...” 22, MAD“I am in shock, I don’t know what is happening to me.” 43, BCN“It is not that serious, it is just asthma.” 22, MAD“It is not a big deal, I can go on with my life as usual.” 44, MAD“I was away with my husband in a rural farm and I felt sick due to the dust and the animals.” 43, BCN |
| Phase 3: First treatment | |
| • Fear of sudden worsening• Doctor's indications are based on common sense rather than scientific evidence• Asthma can be controlled with rescue medication• Unawareness of asthma severity | “I thought I had everything under control with the inhaler. I carried it with me everywhere and felt reassured.” 43, BCN.“The doctor tells me that I am not constant with my medication and that I have to take better care of myself.” 66, SVL“I go on with my life; this is nothing and, if something happens to me, I always have the inhaler with me.” 22, MAD“I realized that the doctor did not really understand what was happening to me. At each visit, he told me something different.” 32, SVL |
Underestimation of the disease was persistently identified in the life experiences reported throughout the three initial phases of the SA patient journey. Similarly, a previous quantitative study had shown that, once diagnosed, 20% of patients underestimated their asthma severity.22 In fact, most participants in this study acknowledged that, before diagnosis, they underestimated asthma and tended to identify it as a medical condition associated with the elderly and stigmatized patients diagnosed with asthma since childhood. Hence, their view of asthma before and after diagnosis agrees with that of the general population, who tends to lack awareness of asthma as a differentiated disease.2 Based on these observations, various authors have stressed the need to increase awareness of asthma as a potentially severe condition among the general population as well.2,7,8,10 In this regard, the perception of asthma as a non-severe condition and, accordingly, not needing proper care, has been previously identified as one of the main barriers to treatment adherence.17,23 Hence, it is possible that the underestimation of asthma during the first phases of the disease has detrimental consequences to health-related outcomes (i.e., risk of exacerbations) in SA patients.
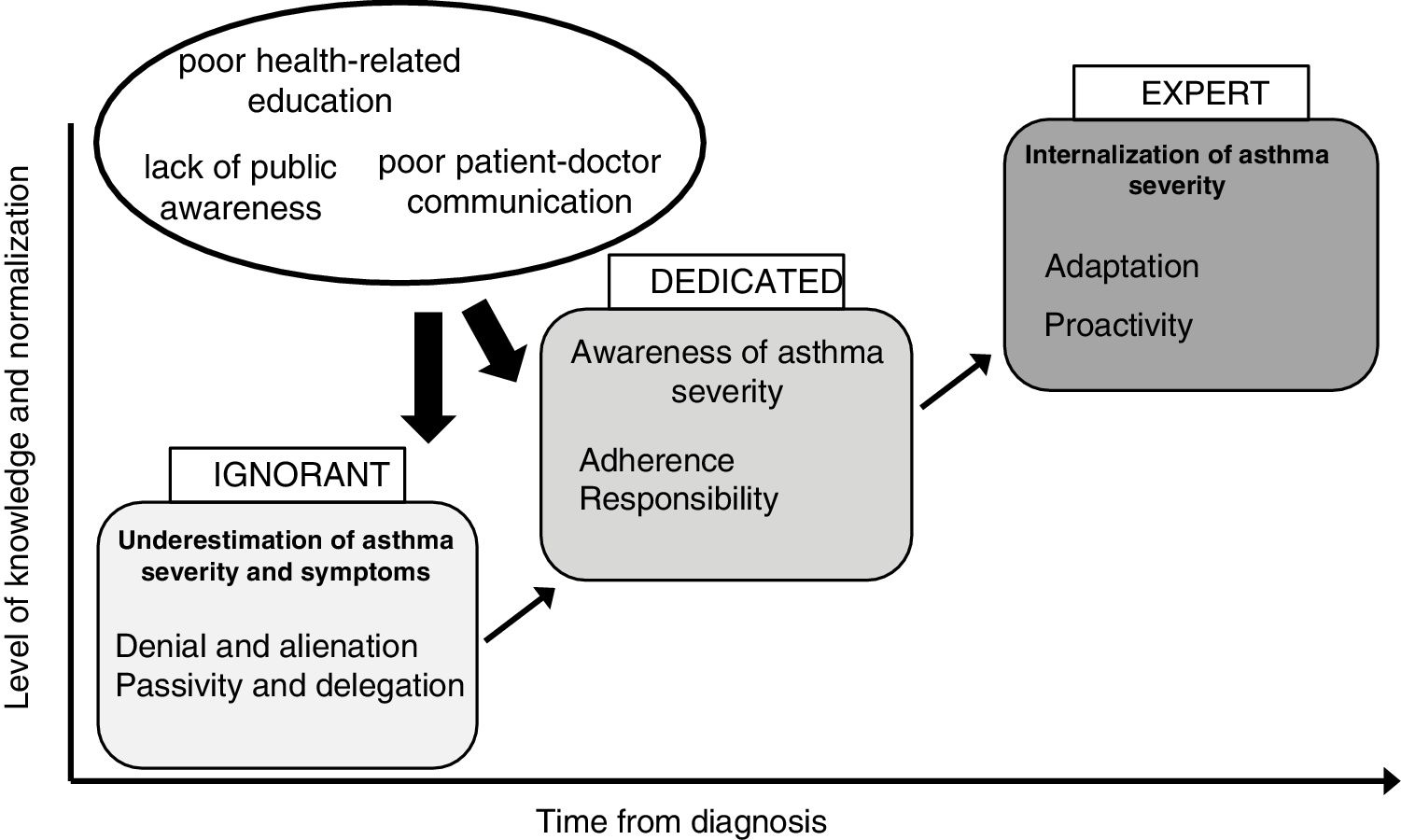
Attitudinal profiles of the SA patientsAttitudes of patients with SA have also evolved throughout three profiles—“ignorant”, “dedicated”, and “expert”—as patients accrued more life experiences and disease knowledge (Table 3). During the initial phases of the disease, most patients fell into the “ignorant” profile, which is characterized by passivity towards their asthma. In addition to being alienated from the disease, these patients were confused by the presence of asthma in their lives and attributed any possible cure or improvement exclusively to their doctor and the prescribed medication; yet their adherence to treatment was incomplete. After some time, patients in the “ignorant” profile evolved into the “dedicated” profile, marked by disease awareness. These patients acknowledged their asthma and were aware that obtaining disease-related knowledge was important to gain control and achieve a cure. Patients with the longest time since diagnosis fell into the “expert” profile, characterized by adaptation to chronicity, and used positive strategies to cope with the disease by reorganizing their lifestyles to be able to lead a “normal” life with asthma.
Attitudinal profiles of patients with severe asthma.
| Main features | Quotes |
|---|---|
| Ignorant profile (passive)Low level of normalization and knowledge: Delegation | |
| • Lack of understanding• Avoidance of asthma interiorization• The specialist is the person responsible for the disease and its management• Unconscious of their personal responsibility in their health status or disease control | “The doctors say I have asthma.” 36, BCN“I feel that taking care of my asthma is the doctor's responsibility.” 22, MAD“If I suspect I have asthma, I take Ventolin, but the doctor tells me I’m abusing it.” 38, SVL“I’m worried about having to take drugs every single day.” 22, MAD“My doctor told me to visit her in case of any problem, no matter how small.” 36, BCN |
| Dedicated profile (aware)Medium level of normalization and knowledge: Adherence | |
| • Responsible for their disease• Continuous search for education to learn to live with asthma• Need to integrate asthma in daily life• Adherent to treatment and doctor's indications• Constantly alert to detect symptoms | “To get better, it is necessary to learn to live with asthma.” 32, SVL“I see asthma as a disease to control.” 43, BCN“I get nervous before an exam, so I need to be careful.” 32, SVL“I don’t know anyone with severe asthma…. Sometimes I worry about having lung cancer.” 38, BCN“Doctors always give you hope; you have to be patient that things will get better.” 32, SVL |
| Expert profile (adapted)High level of normalization and knowledge: Proactivity | |
| • Perception of asthma as a “way of life”• Interiorization of asthma as part of daily life• Ability to recognize symptoms and anticipate their evolution• Willingness to help other patients and become a reference | “I am and will be a chronic asthmatic.” 61, MAD“Asthma is another part of my lifestyle experience.” 44, MAD“Being asthmatic is like having to wear smaller shoes. You need to receive proper treatment to ensure that it fits your needs.” 64, BCN“It is very annoying to see asmathic characters in movies that are always sick and at risk of dying.” 44, MAD |
The life experiences of patients with SA and their association with different attitudinal profiles (i.e., confusion, denial of their chronic condition, and non-recognition of asthma as a disease) have been reported in previous qualitative studies.10,24 However, our analysis went one step further and suggested an evolving pattern throughout well-defined attitudinal profiles. Moreover, the analysis of these profiles revealed their association with patients’ ability to manage their disease and control their symptoms: starting with limited self-management ability (i.e., ignorant profile), through constant search for disease information and self-management (i.e., dedicated profile), to adapting their lifestyle to be able to live with asthma (i.e., expert profile). Altogether, the results from the attitudinal profiles of patients with SA showed that awareness of disease severity increased as patients accepted and internalized the chronicity of asthma years after diagnosis. This association of severity and chronicity might explain the prominent underestimation of asthma identified in patients during the first phases of their journey. Similar to these findings from the expert profile, previous studies concluded that acquiring knowledge, making informed decisions, and accepting the disease are essential to learn to live with a long-term condition.25
Needs of patients with severe asthma regarding disease knowledge and perceptionPatients with SA conveyed several unmet needs, classified in the five main topics summarized in Table 4, mostly related to their level of knowledge about the disease. They complained about the limited information received after diagnosis, and how this fact restricted their ability to interiorize the chronicity of asthma, confidently self-manage their disease, and trust doctors’ decisions regarding treatment. On the other hand, patients felt that the general public and healthcare professionals, in particular those attending to them in the emergency room, considered the disease unimportant and felt that asthma received less attention compared to other chronic conditions.
Needs of patients with severe asthma regarding disease knowledge and perception.
| Main subtopics | Quotes |
|---|---|
| Topic 1: To have a comprehensive understanding of the disease from the beginning. | |
| • To be informed about:∘ Disease phases, their evolution, and steps to take∘ The severity that SA may have in the future• To interiorize from the beginning that:∘ Asthma has no cure∘ Finding the right treatment may require trying several• To understand relationships between future symptoms (i.e., allergy and panic) | “I think the doctor knew what was going to happen to me, but he didn’t tell me.” 36, BCN“I searched the Internet for information about SA and I almost went crazy. I found completely different descriptions, from a soft disease to a life-threatening one.” 38, BCN |
| Topic 2: To feel that my current status is not a consequence of my previous unconcern. | |
| • To avoid feeling guilty for worsening of my asthma after delaying a visit to the ER• To be reassured in my decisions about my asthma in spite of not strictly complying with the treatment and doctor's indications• To forget about the disease for short periods of time without consequences• To be reassured about the safety of the medication in case of pregnancy | “During my first pregnancy, I was fine, but I was very worried with my second one. Mind you, everything went well.” 44, MAD“When the doctors stopped my treatment, I suffered a crisis again.”43, BCN |
| Topic 3: To feel that I have control over my disease. | |
| • To feel that asthma limits my life but does not govern it• To adapt my activities without having to stop doing them• To foresee environmental conditions causing attacks or instability and be aware of its potential effects• To feel that I have tools to avoid or delay asthma attacks to have time to go to the ER | “The grass allergy season is a few months away; I can’t stop thinking about it, I have the toughest time.” 38, SVL“I had to eat breakfast in the locker room because everyone was smoking in the cafeteria and it was impossible to eat.” 61, MAD |
| Topic 4: To balance my perception of disease with that of my environment. | |
| • To feel that my doctor understands my emotions and considers the disease important• To feel that healthcare professionals understand my situation and therefore, I am given priority during my visits to the ER• To feel social support and awareness, at the same level that other chronic conditions | “They keep me waiting for a long time and then they just want to run tests; I only want to put on the mask as soon as possible.” 36, BCN“I don’t know how to explain to my doctor what is happening to me.” 22, MAD |
| Topic 5: To be sure I am prescribed the best possible treatment. | |
| • To trust the specialist in case of worsening• To be sure that any improvement is due to the expert knowledge of the doctor• To be sure that any improvement will last for a long time• To be sure that there are not any novel treatments• To be updated by the doctor about any novel treatment | “With every change in medication you think, “This is it,” and at the same time you know it won’t last.”, 64, BCN |
Previous studies conducted in different countries have typically identified a demand for non-technical disease information among asthma patients, suggesting the need for educational interventions, which should also be addressed to the general public to raise awareness.2,24 Similarly, participants in this study wished they had received comprehensive disease-related information from the beginning. This finding, together with the underestimation of the disease and attitudinal profiles identified in this study, raise the possibility that insufficient asthma-related education after diagnosis influenced disease perception and delayed their interiorization of asthma as a chronic disease.
Patients’ relationship and communication with doctors and healthcare providersFour main topics, summarized in Table 5, describe the relationship between patients and healthcare providers. Participants considered their primary doctor to be insufficiently prepared to treat SA and remarkably, perceived that general practitioners tended to underestimate their health status, delaying referral to a specialist. While allergists, and specially pulmonologists, were considered to have the best expertise in SA, their relationship and communication were hampered by the use of technical language, their frequent rotation, and the short time scheduled for visits.
Patients’ relationship and communication with doctors and healthcare providers.
| Main subtopics | Quotes |
|---|---|
| Topic 1: The patient does not perceive his/her doctor as a great specialist in SA treatment. | |
| • The doctor uses asthma chronicity as an excuse to stop looking for novel treatments and choose conservative treatments.• The doctor gives incomplete information, occasionally on purpose.• The doctor gives incomplete and random explanations about the causes of the crisis.• The doctor blames the patient's disease self-management when his/her status worsens. | “He/she normalizes everything by talking about my disease's chronicity; no matter how bad I am, he/she always thinks it is normal.” 64, BCN“My doctor has been very conservative since the beginning. He has always gone from less to more. I would have tried something stronger.” 38, BCN |
| Topic 2: Follow-up visits do not meet the patient's expectations. | |
| • Unsatisfactory frequency and duration, hampering empathy and closeness• Frequent change in specialist: difficulty to establish a relationship; prevents follow-up | “I know that the doctors don’t have enough time for me, so I avoid some questions.” 38, SVL“Since my diagnosis, I have visited several doctors with different points of views about my condition.” 36, BCN |
| Topic 3: The pulmonologist and allergist are perceived as two clearly differentiated approaches. | |
| • The pulmonologist is considered to have the best expertise, although a holistic approach to the patient's needs is missing.• The specialist uses technical language, distant from their life experiences, which intimidates them to raise any doubts• Positive perception of the allergist's efforts to explain the relationship between severe asthma, panic attacks, and allergy. | “My pulmonologist is very cold, he/she is not much concerned about my life, many times he/she just reads, reads, and reads.” 44, MAD “At first I was told I had asthma because of the allergy, then that the allergy was due to asthma, but they never explained to me the relationship between them.” 38, BCN |
| Topic 4: The patient believes that his/her primary care physician lacks training to treat SA. | |
| • The primare care physician lacks specific knowledge about asthma, resulting in persistent confusion.• The primary care physician lacks sufficient resources and the necessary motivation.• The primare care physician delays diagnosis and referral to the specialist as a result of underestimating the disease.• The primare care physician generates high expectations in the specialist's care, and these are not fulfilled. | “I have the feeling that my doctor is experimenting with me, without quite knowing what he/she is doing, until he runs out of options and can’t go any further.” 64, BCN“My primary care physician tells me he/she can’t give me any more options, that the pulmonologist should do it, but he/she cannot give me a solution either…” 61, MAD |
Previous studies have reported a suboptimal relationship and communication between SA patients and the general practitioner and/or specialist, and have acknowledged the patients’ unmet need to receive clear, understandable information. These deficiencies may impact patients’ health literacy and subsequent health-related behaviours.13,18,26 In this regard, the proposed discussion and preparation of personalized asthma plans, together with life plan counselling, may constitute useful strategies to improve the doctor-patient communication.7,27
Conclusions, usefulness and limitationsResults from this study, summarized in Fig. 1 and detailed in the context of the complete patient journey in Fig. S1, show that the lack of general awareness of SA as a differentiated disease determines the underestimation of its severity and symptoms by newly diagnosed patients, resulting in an initial attitude of denial and alienation towards the disease. Patients’ life experiences and attitudinal profiles towards doctors and treatments tend to evolve over time from disease diagnosis; the chronicity of asthma is usually internalized years after diagnosis, thus delaying the adaptation of patients’ lifestyle. Furthermore, our study detected that poor disease-related education and communication with healthcare providers likely contributes to the patients’ delayed understanding and ability to control and self-manage their condition.
The current patient-centred attention model for chronic diseases is based on providing patients with sufficient tools (i.e. disease-related knowledge) and establishing a relationship with their doctors for disease self-management and shared decision-making.1 In this regard, the results of this study concerning disease perception and internalization of asthma as a chronic disease identified novel gaps in SA patient care. Furthermore, the demand for more disease-related information and improved doctor-patient relationship and communication, underscored the accepted need of an effective communication of health-related information. The identification of these gaps may be useful for healthcare professionals and policymakers to design interventions addressed to the patients with SA and the general population, and meet the demands of SA patients with the overarching goal of improving their quality of life.
Ethnographic research should be understood in the context of the general limitations of this methodology regarding the generalizability of results and sample size, which may have restricted our findings. In spite of their limited number, the participants included in this study were representative of different demographic and clinical characteristics and, consequently, life experiences. This study used a generative methodology to achieve a general understanding of the life experiences of patients with SA over time rather than describing all possible experiences. In this respect, this study succeeded in describing the evolution of disease perception, disease internalization and patient attitudinal profiles, helping to identify needs and gaps in SA patient care. The relevance and usefulness of the findings presented here should promote future qualitative studies including both patients and healthcare providers to address the suitability of potential interventions to improve SA patient care.
FundingThis study was funded by AstraZeneca Farmacéutica Spain, S.A.
Conflicts of interestIU has nothing to disclose. GR is an employee of AstraZeneca Farmacéutica S.A, Spain.
The authors would like to thank i2e3 for providing medical writing support.