Poor sleep hygiene and the hour of changing shifts are among the most important factors which affect the quality of services in the intensive care unit. The present study aimed to investigate the demographic properties of patients who died in the intensive care unit and their association with their death hour.
Materials and methodsAs a cross-sectional study, this study was performed by referring to the Statistics Center of Hazrat Rasool Akram Hospital and collecting the demographic information of dead patients at 12 intensive care units in this hospital. This information includes age, sex, the cause of death, and the exact time of death of these patients.
ResultsIn this study, the rate of mortality in intensive care units was assessed as follows; from 12 pm to 2 am (14.48%), from 2 am to 4 (5.49%), from 4 to 6 am (8.99%), from 6 to 8 am (11.32%), from 8 to 10 am (6.79%), from 10 am to 12 noon (8.03%), from 12 to 14 (6.04%), from 14 to 16 (6.93%), from 16 to 18 (7.41%), from 18 to 20 (9.47%), from 20 to 22 (8.1%), and from 22 to 24 hours (6.93%). The highest rate of mortality was between 12–2 AM and then 6–8 AM. In this study, a significant rate of deaths occurred during the night and the lowest rate was during normal work hours and in fact during the morning hours of visiting patients.
ConclusionSince the highest rate of mortality was during night hours, during the hours of changing shifts, and at the beginning of midnight, the mortality rate could be decreased with the decrement in staff's working hours and paying more attention to patients during these hours, the overall mortality rate of patients could be decreased in ICU units.
La mala higiene del sueño y el horario de cambio de turno se encuentran entre los factores más importantes que afectan la calidad de los servicios en la unidad de cuidados intensivos. El presente estudio tuvo como objetivo investigar las propiedades demográficas de los pacientes que fallecieron en la unidad de cuidados intensivos y su asociación con la hora de su muerte.
Materiales y MétodosComo estudio transversal, este estudio se realizó remitiendo al Centro de Estadísticas del Hospital Hazrat Rasool Akram y recopilando la información demográfica de los pacientes fallecidos en 12 unidades de cuidados intensivos de este hospital. Esta información incluye la edad, el sexo, la causa de la muerte y la hora exacta de la muerte de estos pacientes.
ResultadosEn este estudio, la tasa de mortalidad en las unidades de cuidados intensivos se evaluó de la siguiente manera; de 12 a 2 am (14,48%), de 2 a 4 am (5,49%), de 4 a 6 am (8,99%), de 6 a 8 am (11,32%), de 8 a 10 am (6,79%), de 10 a 12 horas (8,03%), de 12 a 14 (6,04%), de 14 a 16 (6,93%), de 16 a 18 (7,41%), de 18 a 20 (9,47%), de 20 a 22 (8,1%), y de 22 a 24 horas (6,93%). La tasa más alta de mortalidad fue entre las 12 y las 2 de la mañana y luego entre las 6 y las 8 de la mañana. En este estudio, una tasa significativa de muertes ocurrió durante la noche y la tasa más baja fue durante las horas normales de trabajo y, de hecho, durante las horas de la mañana de visita a los pacientes.
ConclusiónÉtant donné que le taux de mortalité le plus élevé était pendant les heures de nuit, pendant les heures de changement de poste et au début de minuit, le taux de mortalité pourrait être diminué avec la diminution des heures de travail du personnel et en accordant plus d'attention aux patients pendant ces heures, l'ensemble le taux de mortalité des patients pourrait être diminué dans les unités de soins intensifs.
In hospitals, some special wards are considered for precise control and instant monitoring to reduce mortality in critically ill patients.1 The intensive care unit (ICU) is one of the specialized departments in hospitals that provide special care and treatment services. This department is also called ICU, coronary care unit (CCU), and intensive therapy unit (ITU).2 In this department, patients are monitored momentarily and around the clock, and the therapies are performed in both invasive and semi-invasive procedures.3 The most frequently prescribed drugs were intensive care medications given to patients. The cardiopulmonary care unit (CPU) is also located inside the ICU department.4 The ICU departments inside the hospitals are usually divided into several types including Pediatric Intensive Care Unit (PICU), Mobile Intensive Care Unit (MICU), Surgical Intensive Care Unit (SICU), and cardiopulmonary unit (CPU).5 Generally, ICU is a department with the most specialized staff and physicians in which critically ill patients are held under the best possible conditions with the latest available equipment.6 This department requires advanced equipment and skilled doctors and nurses who are trained and prepared specially for this department.7
Generally, based on the care requirements patients are divided into five groups which include critically ill patients, patients with moderate care requirements, self-reliant patients, patients with chronic conditions, and outpatients.8 A reduction in the care given to the patients in this department could cause irreparable consequences. Among the things which could decrease the quality of care services provided by the personnel of this department are fatigue, the time for changing work shifts, inexperienced medical staff, lack of knowledge about the duties of each staff, and ect.9 Based on the data from previous studies, the mortality rate of ICU patients between 12–18 PM was 30%, and in NON-ICU patients was 38% between 6:00–12:00 PM.10 Moreover, the mortality rate of patients in the surgical Intensive Care Unit (SICU) was higher on holidays compared to the other days (16.3% on holidays and 15.3% on normal days).10
While other studies did not show any differences between holidays and non-holidays.11 Another study with the same issue revealed that the mortality rate in patients who are admitted to the ICU at night is higher compared to the patients who are admitted to the ICU during the day.12 Other studies reported an increased rate of mortality on weekends compared to other days of the week.4 Another study revealed that there was no significant difference between the mortality rate of patients in the ICU and the normal department of the hospital during the month or daily. However, this difference would become significant over more than three years.13 Based on the data from another study, in patients treated with ST-elevation myocardial infarction (STEMI) diagnosis, a significant difference between the mortality rate during working and non-working hours was observed.14 Due to the importance of this subject, the present study was performed to determine the effect of different hours of the day on the mortality rate of patients admitted to the ICUs of Rasoul Akram Hospital in 2021.
MethodsThe present study is an analytical cross-sectional descriptive survey conducted on 1457 dead people in the ICU department of Rasoul Akram Hospital in 2021. The exclusion criteria were patients with incomplete records were excluded from the survey. All the data of the patients who died in the ICU department of Rasool Akram Hospital were collected including the exact time of death, age, sex, the leading cause of death, and the relevant department. The study was started after obtaining the required approval to carry out the project from the ethics committee of the Iran University of Medical Sciences and also the ethics code (IR.IUMS.FMD.REC.1400.531). After referring to the data center of Hazrat Rasool Akram Hospital, the documents, and data of patients who died in the ICU department in 2021 were surveyed. All collected data were kept confidential, then stored and analyzed, and finally published without mentioning the name.
At first, the data about the demographic properties of the patients were recorded on a checklist. The demographic information includes age, gender, the leading cause of death, the exact time of death, and the department in which patients died. This information was obtained by reviewing the data of patients who died in the ICU department of the data center of Rasoul Akram Hospital.
Data analysisFinally, after data collection, all data was entered into SPSS Statistics Version 24, and then statistical analysis was performed. For qualitative variables, frequency and the percentage of the frequency were evaluated, and for quantitative variables mean and standard deviation was evaluated. A T-test was used to evaluate the differences between quantitative variables. When the distribution of data was abnormal, Mann–Whitney U test was used to analyze data. Moreover, an analysis of qualitative variables was also done using the Chi-square test. Survival analysis of data was used using regression analysis. SPSS Statistics Version 24 was used for analyzing the data of the present study. The significance level was considered less than 0.05.
Ethical considerationsAt first, the consent of the ethics committee was obtained and then a particular code of ethics was received for the project. After that, the collected data were kept confidential and then analyzed without even a specific name. Before starting the work, a complete explanation of the research objectives and its method was provided to all the staff and research units in written and oral form. All data and documents of patients were used after obtaining permission. The data of patients remained confidential and was not disclosed to any natural or legal person and was only reported in groups. Participation in the study had no financial burden on the participants. This research does not have any contradictions to religious and cultural norms and society.
ResultsIn the present study, the data of 1457 patients who died in the ICU units of Rasoul Akram Hospital in Tehran in 2021 were surveyed. In general, Hazrat Rasool Akram Hospital has twelve ICU units that provide medical services to patients. Based on the data, 147 patients (85 men and 62 women with a mean age of 73 years) died in the ICU unit.
Since the ICU unit was among the special hospital departments which provided services to non-Covid patients during the pandemic, the main reason for the death of all 147 patients in this unit was non-Covid causes. Based on the data achieved from the analysis of the death rate per hour of the day, 34% of patients died between 12 and 7 AM. The highest rate of death was at 12 noon and also between 6–8 AM at which the hospital staff changed their shifts.
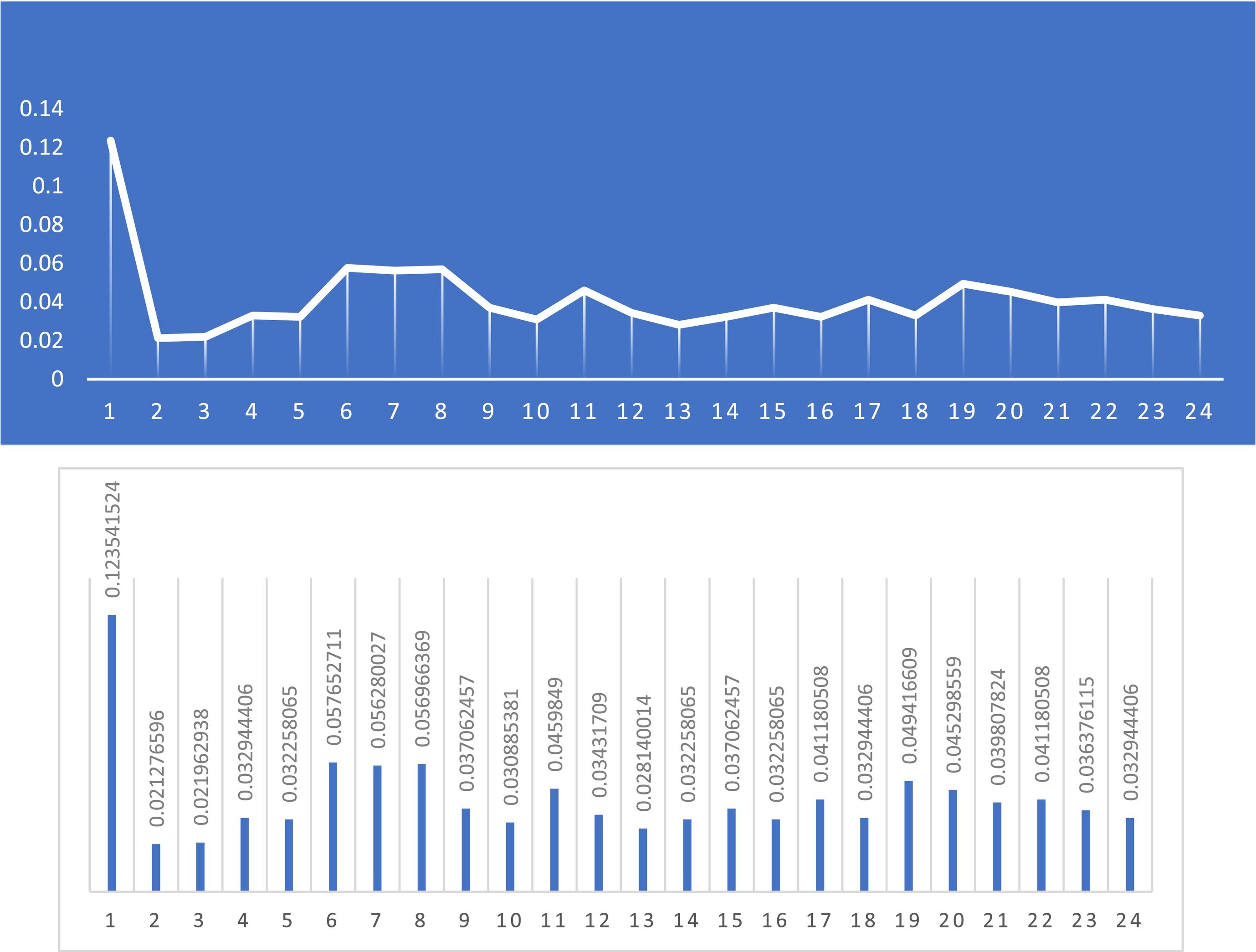
The difference between the death rate and the hour of death was significant (p-value <0.0001). Due to the higher rate of death at night, it could be concluded that night care has a significant effect on the death rate in this unit. Table 1 represents the data for other units. As can be seen from the following table, the difference between the death rate of men and women is significant. This difference raises a question about the main reason for this difference and why the death rate of men is higher compared to that of women. Moreover, in both genders, the higher rate of death is between 60 and 70 years (age has a significant association with the death rate in the 60s and 90s). Investigation around the reason for death revealed that 711 (49%) died of corona and 746 (51%) died of other factors. The results of the investigation of the exact time of death are represented in Fig. 1 and Table 2.
The demographic survey and exact death time of patients in ICU units.
| Time of death(Percentage %) | Average age | Women | Men | The number of dead people(Percentage %) | Unit |
|---|---|---|---|---|---|
| 8–12 (34) | 73 | 62 | 85 | 147 (10.1) | Emergency ICU |
| 6–12 (34) | 66 | 11 | 107 | 178 (12.2) | MICU |
| 12–1 (41) | 60 | 28 | 71 | 99 (4.9) | SICU |
| 6–8 (51) | 67 | 87 | 130 | 217 (14.9) | Neurosurgical ICU |
| 6–8 and 12–1 (42) | 67 | 80 | 97 | 177 (21.1) | Neurointensive care unit |
| 12–8 | 44 | 3 | 21 | 24 (1.6) | ICU OPU |
| 12–1 | 68 | 20 | 135 | 155 (10.6) | ICU Royal |
| 17–18 and 12–1 | 64 | 40 | 52 | 92 (6.3) | Orange ICU |
| 6–8 and 12–1 (39) | 65 | 137 | 167 | 304 (20.9) | ICU 4 |
| 21–22 and 1–2 (43) | - | 6 | 8 | 14 (1) | NICU |
| 3–6 (41) | 6 | 22 | 32 | 54 (3.7) | PICU |
| 23–1 (38) | 59 | 4 | 20 | 24 (1.6) | CCU |
| Night hours and the hours of changing shifts, 12–8 (40) | 63 | 607 | 850 | 1457 (100) | Total |
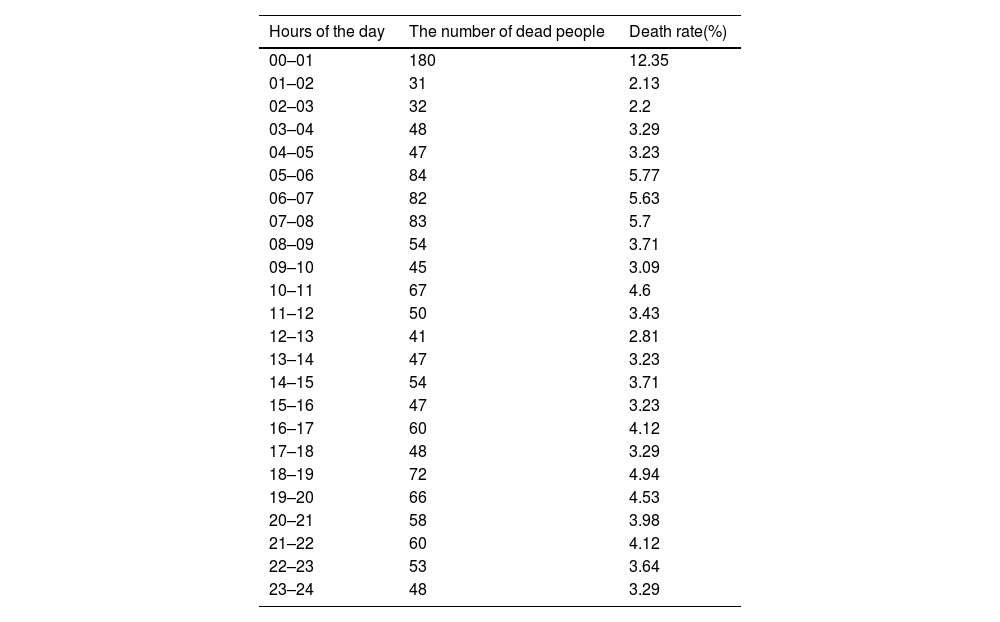
The death rate of patients admitted to ICU units based on the hours of the day.
| Hours of the day | The number of dead people | Death rate(%) |
|---|---|---|
| 00–01 | 180 | 12.35 |
| 01–02 | 31 | 2.13 |
| 02–03 | 32 | 2.2 |
| 03–04 | 48 | 3.29 |
| 04–05 | 47 | 3.23 |
| 05–06 | 84 | 5.77 |
| 06–07 | 82 | 5.63 |
| 07–08 | 83 | 5.7 |
| 08–09 | 54 | 3.71 |
| 09–10 | 45 | 3.09 |
| 10–11 | 67 | 4.6 |
| 11–12 | 50 | 3.43 |
| 12–13 | 41 | 2.81 |
| 13–14 | 47 | 3.23 |
| 14–15 | 54 | 3.71 |
| 15–16 | 47 | 3.23 |
| 16–17 | 60 | 4.12 |
| 17–18 | 48 | 3.29 |
| 18–19 | 72 | 4.94 |
| 19–20 | 66 | 4.53 |
| 20–21 | 58 | 3.98 |
| 21–22 | 60 | 4.12 |
| 22–23 | 53 | 3.64 |
| 23–24 | 48 | 3.29 |
In the present study, the highest rate of death was in the early hours of the night and then between 5–8 AM. As expected, the highest rate of deaths happened during the night shift. If the day is divided into three parts, the lowest rate of death occurred during normal working hours (during the patients' morning visits), and the highest rate of death occurred during the night hours, as shown in Fig. 2.
1: Night (12–8 AM); 2: Morning (8–4 PM); 3: Evening (16–24 PM)
Investigating the association of death rate with the hours per day, revealed a significant difference in terms of days' hours (P-value<0.000). This association is due to that mortality peaked between 00:00 and 2:00 AM. Moreover, it was revealed that the mortality rate increases significantly during the night hours.
DiscussionICU units in hospitals are among the most crucial departments. However, due to their role in providing services to critically ill patients, has a higher mortality rate in comparison with the other departments. It should be noted that increasing the quality of services in this department decreases the rate of death and improves health indicators in the community. In our study, 1457 death were surveyed in 12 different ICU units. The frequency of mortality based on the hours of the day was as follows; 00:00 to 2 AM (14.48%), 2 to 4 AM (5.49%), 4 to 6 AM (8.99%), 6 to 8 AM (11.32%), 8 to 10 AM (6.79%), 10 AM to 12 noon (8.03%), 12 to 14 (6.04%), 14 to 16 (6.93%), 16 to 18 (7.41%), 18 to 20 (9.47%), 20 to 22 (8.1%) and between 22 to 24 (6.93%). In a study by Cordiero10 who examined 700 dead people, 21% of deaths happened between 00:00 and 6:00 AM, which was the lowest mortality in their study. In their study, Vicent15 surveyed 500 dead people. Based on their study, 27.9% of death happened between 00:00 and 6:00 AM, which was as same as the results of our study. However, in their study, the peak down of death was between 00:00 and 6:00 AM which is contrary to our study, because the peak death rate of our study is 28.96٪ in the mentioned time period.
In a study by Cordeiro,10 the rate of mortality between 6:00 AM to 12:00 noon was 21% which was the lowest recorded mortality rate during these hours, while in our study it was 26.15%. A study by Vicent15 reported a total mortality rate of 36.02% between 12:00 PM to 18:00. Another study by Cordeiro10 reported a mortality rate of 30% in this time period as the highest mortality rate which contradicts our study because based on our data the highest mortality rate in these hours was about 20.38%. However, this percentage is the lowest mortality rate in 6-hour intervals in our study. In a study by Cordeiro,10 the rate of mortality between 6:00 AM to 12:00 noon was 21% which was the lowest recorded mortality rate during these hours, while in our study it was 26.15%. A study by Vicent15 reported a total mortality rate of 36.02% between 12:00 PM to 18:00. Another study by Cordeiro10 reported a mortality rate of 30% in this time period as the highest mortality rate which contradicts our study because based on our data the highest mortality rate in these hours was about 20.38%. However, this percentage is the lowest mortality rate in 6-hour intervals in our study.
In their study, Corderio10 reported a mortality rate of 24% between 18:00 and 24:00, while in Vicent's15 studies, the rate of mortality in that time period was 38%. Both of mentioned rates were in contrast with our study in which a mortality rate of 24.5% is reported for the mentioned time period. As aforementioned, the quality of patient care significantly affects the mortality rate. The most well-known factors as ones that reduce the quality of services are fatigue, drowsiness, and the hours of changing working shifts. In Hazrat Rasool Akram Hospital the hours of changing working shifts are different in various departments and generally are between 6:30 PM to 7:30 PM and 6:30 AM to 7:30 AM. Another study by Park13 investigated 3198 dead people, based on which 14:00 and 16:00, and 20:00 to 22:00 were reported as the peak time of death. Lowan12 studied 149894 dead cases, which is the peak frequency of deaths reported between 5:00 AM and 6:00 AM. Based on our data the peak time of death was reported to be between 5:00 AM and 6:00 AM. While three other time periods of 00:00 and 2:00 AM and 6:00 AM to 8:00 AM and 18:00 to 20:00 were also introduced as the peak time. A similar study by Artz16 investigated 700 dead people who had heart diseases and introduced two time peaks which were 6:00 AM and the time between 4:00 PM and 7:00 PM.
In the ICU units of hospitals, patients are usually visited daily by doctors in the morning. In Hazrat Rasool Akram Hospital, patients are visited by specialists while concentrating on patient tests and clinical courses based on the reason for patients' diseases. Based on a study by IOWAN,12 it was observed that the mortality of patients during the time interval of 8:00 AM and 2:00 PM (common working hours) based on the patient's admission to the hospital is less compared to the other working hours which is in line with the data of our study.
By dividing the day into three parts, the lowest mortality rate was recorded from 8:00 AM to 16:00 (27.8%), and the highest mortality rate was at night (00:00 to 08:00 AM) with a rate of 40%. It's while Pienaar11 reported that 767 patients died during the day and 469 patients died at night which doesn't match the results of our study.
ConclusionIn our study, the highest mortality rate was in the early hours of midnight and during the hours in which the staff change their shift. In this regard, with the decrement in staff working hours and paying more attention to patients during these hours, the overall mortality rate of patients could be decreased in ICU units.