A 43-year-old woman with a past medical history of renal microlithiasis was admitted to the Emergency Department with sudden onset of haemoptysis, dyspnoea and the need for oxygen therapy to maintain oxygen saturation above 90%.
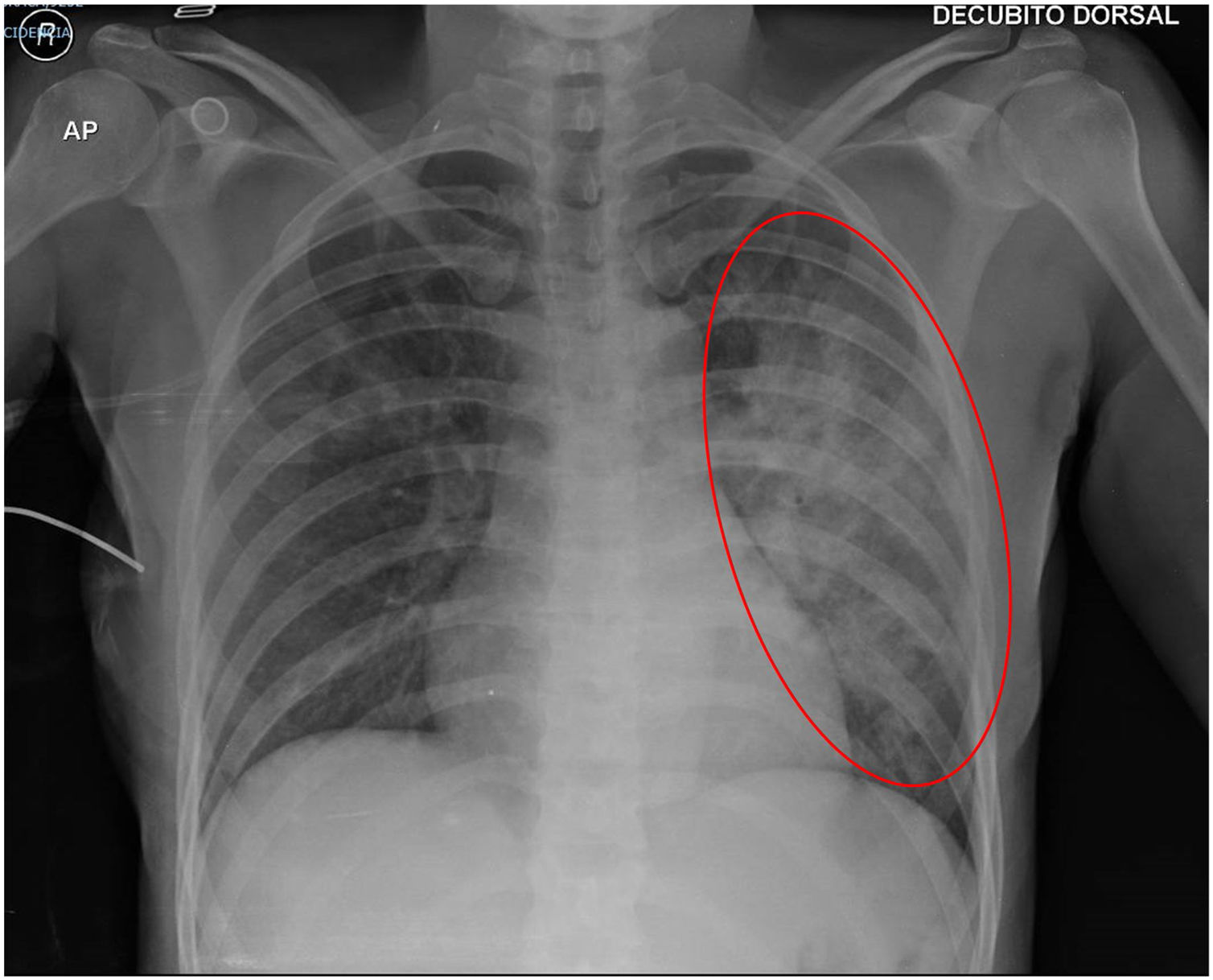
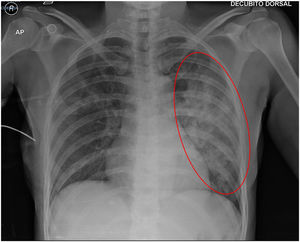
The chest X-ray showed diffuse infiltrates in the left haemithorax (Fig. 1) and a chest CT documented densification of the bilateral pulmonary interstitium, especially on the left hand side (Fig. 2), compatible with Alveolar Haemorrhage. She was admitted to the Intermediate Care Unit for haemodynamic surveillance and required red blood cell transfusion. Koch's bacillus screening was negative.
A bronchofibroscopy revealed haematic traces throughout the left bronchial tree. A urinalysis showed microscopic haematuria and proteinuria. Vasculitis was suspected, therefore specific laboratory studies were requested and the patient was started on a methylprednisolone cycle (1000mg) during 5 days, followed by oral corticosteroid therapy.
The laboratory studies results came back positive for anti-proteinase 3 anti-neutrophil cytoplasmic antibodies, giving the diagnosis of granulomatosis with polyangiitis.
The patient was discharge on oral corticosteroid therapy and given a progressive tapering plan.
Granulomatosis with polyangiitis is a type of small vessel vasculitis, characterized by necrotizing granulomatous inflammation1,2 and most often affects the respiratory tract and kidneys. Alveolar haemorrhage occurs up to 10% of cases.2