Reflex epilepsy is characterized by seizures triggered by a specific stimulus. Photosensitive epilepsy (PSE) has seizures provoked by photic stimuli. PSE is the most common form of reflex epilepsy and affects 2–5% of patients with epilepsy. The main feature is photosensitivity, which is an abnormal paroxysmal electrical reaction in the brain induced by strobe lights. The photoparoxysmal response (PPR) is the appearance of epileptiform activity induced by intermittent photic stimulation (IPS).1,2
Capovilla G et al, have demonstrated that Z1-filter, was more effective than four other colored types of lenses in reducing the response to IPS in PSE patients.3 These results were confirmed in a multicenter study, the use of Z1 filters abolished PPR in 75.9% and a 17.9% of PPR attenuation, evaluated by increased latency between the stimulus and the appearance of PPR, reduced duration of PPR, disappearance of clinical manifestations, or change to a less severe type according to Waltz's classification in17.9% from patients.4,5
It has been previously described that 30% of patients with epilepsy have no control of their seizures, despite the use of 2 or more correctly used AEDs, considering this condition as Drug Resistant Epilepsy (DRE). Valproic acid can control photosensitivity in about 40% of cases. There are no studies focusing on patients with PSE who are refractory to Valproic Acid. We selected from our database, those patients who had PSE, and continued with seizures despite the use of Valproic Acid in doses of at least 1500mg/day or higher and a new AED.6–9 Most of patients (n:9), have shown plasma levels of Valproic Acid were within the therapeutic range. Nevertheless, in the rest of patients (n:6) these levels could not be obtained. In all of studied population, Valproic Acid dosis was tolerated without toxic effects. The correlation between plasma levels of Valproic Acid and PPR wasn’t studied. None of the patients received AEDs or other drugs that were hepatic inducers.
The aim of this study was to assess whether the use of Z1 filters can reduce PPR in patients with drug-resistant PSE.
Prospective study to analyze the role of Z1 filters in the PPR from patients with drug-resistant PSE was performed. It was approved by the Ethics Committee of the Hospital Britanico. All patients signed an informed consent form. Patients with PSE, who had seizures despite being medicated with valproic acid at a minimum dose of 1500mg and at least one of the following AEDs (levetiracetam: 1000–3000mg/day, lacosamide 200–400mg/day and topiramate 200–400mg/day). For each patient, the maximum tolerated dose without adverse effects was used.were included.
Before performing the EEG, a complete ophthalmological examination was performed on all patients. An EEG was performed in a twilight room with 32-channel equipment (Neurovirtual®). Longitudinal, transversal and reference assemblies were used, according to the International 10/20 System. After 20min of recording, the IPS was performed with a photo-stimulator placed 30cm from the patient's face. Each stimulation lasted 1ms for 5s at 30-s intervals. Frequencies between 3 and 50Hz were used.3 EEG recording with Intermittent Photic Stimulation.
Identical IPS protocol was implemented after the application of the Z.1 filter (Zeiss™) in front of the patient's eyes. PPR was evaluated using the Scale described by Waltz patients,10 which gives a score from 1 to 4 according to the severity of the response to IPS.
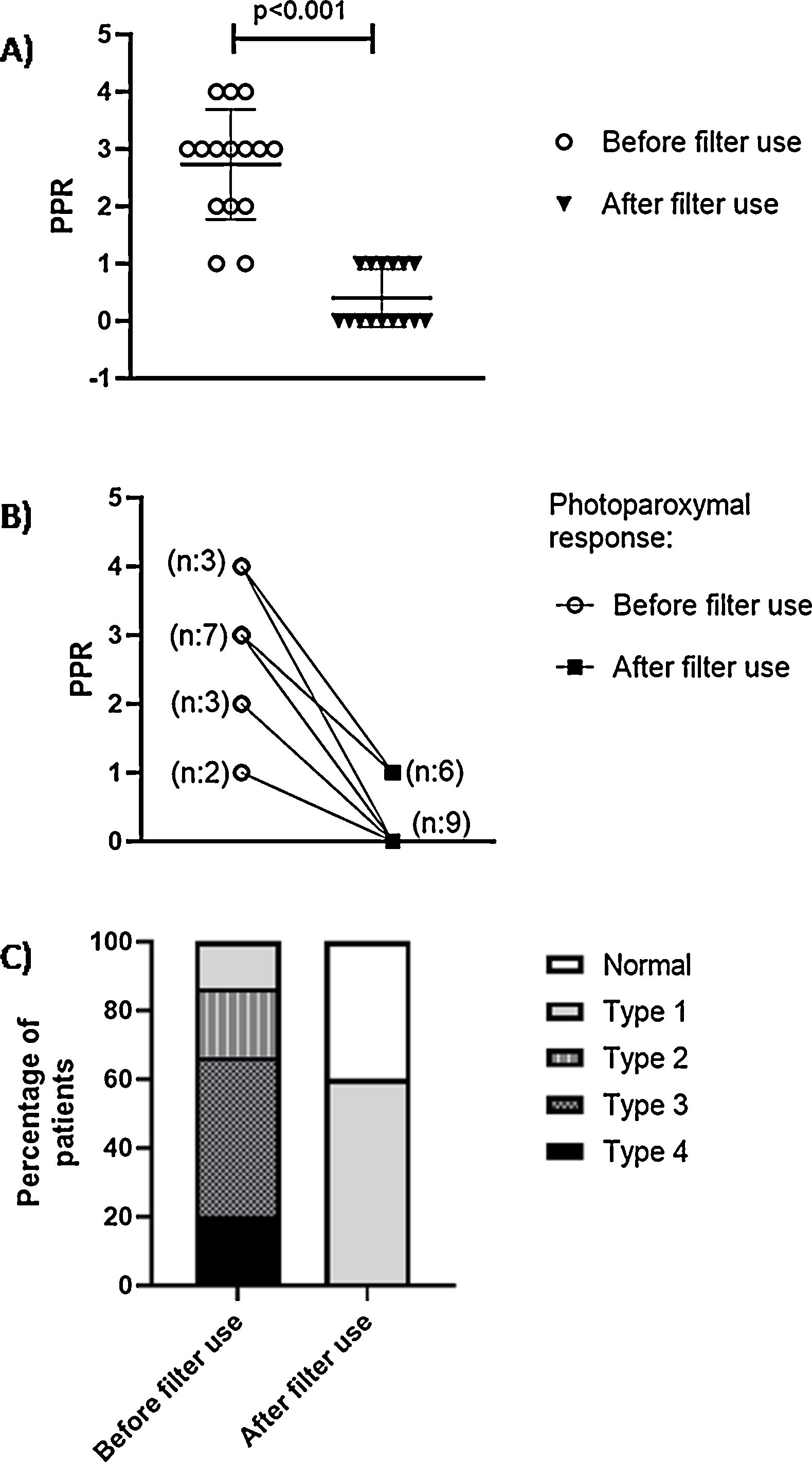
We included 15 patients with PSE. Mean age was 30.3±12.8 years. 53.4% were female. PPR without the use of Z.1 filter showed that the population in this study presented PPR in the following distribution: Type 4: 20% (n: 3); Type 3: 46.6% (n: 7); Type 2: 20% (n: 3); Type 1: 13.4% (n: 2); Type 1 (Fig. 1A). Our findings showed a significant decrease in PPR severity after the use of Filters Zeiss F.1 filters (0.4±0.2 vs. 2.7±0.9; p<0.001) (Fig. 1B). With the use of Zeiss F.1 filters, in more than half of the patients (60%) PPR was abolished (Fig. 1C). Type 1 were 6 patients and with PPR Abolition, 9 patients.
In our study the Z1 Filters were effective in reducing photosensitivity in PSE patients treated with valproic acid and second or third generation AED.
To our knowledge, there are no studies on the reduction of PPR with the use of Z1 filters only in patients with valproic acid associated with a third generation AED.
To avoid photosensitivity, different strategies can be adopted.11 For example, avoiding places where this type of light stimuli are more frequent, treatment with AEDs or the use of special filters.5 We agree that the Z1 filters are effective, even in patients receiving pharmacological treatment with 2 AEDs.