Asthma may have a detrimental effect on school attendance and achievement. Friend relations, attendance to school activities, quality of life (QOL) of asthmatic children may be negatively affected. The aim of this study was to evaluate factors influencing school functioning for asthmatic school-age children.
Materials and MethodsFrom January to May 2019, parents and school-age children who were followed by a diagnosis of asthma for more than one year, from seven pediatric allergy centers, were given a standard questionnaire including questions about child’s disease, school performance, absenteeism, home-family-school conditions. A pediatric QOL questionnaire was filled out by children. For evaluating control in the previous year, children who had more than two exacerbations and/or had any exacerbations needing systemic corticosteroids in the previous year were defined as inadequate control. School absence over nine days was taken into account as this has been shown to bring a risk for successful school life.
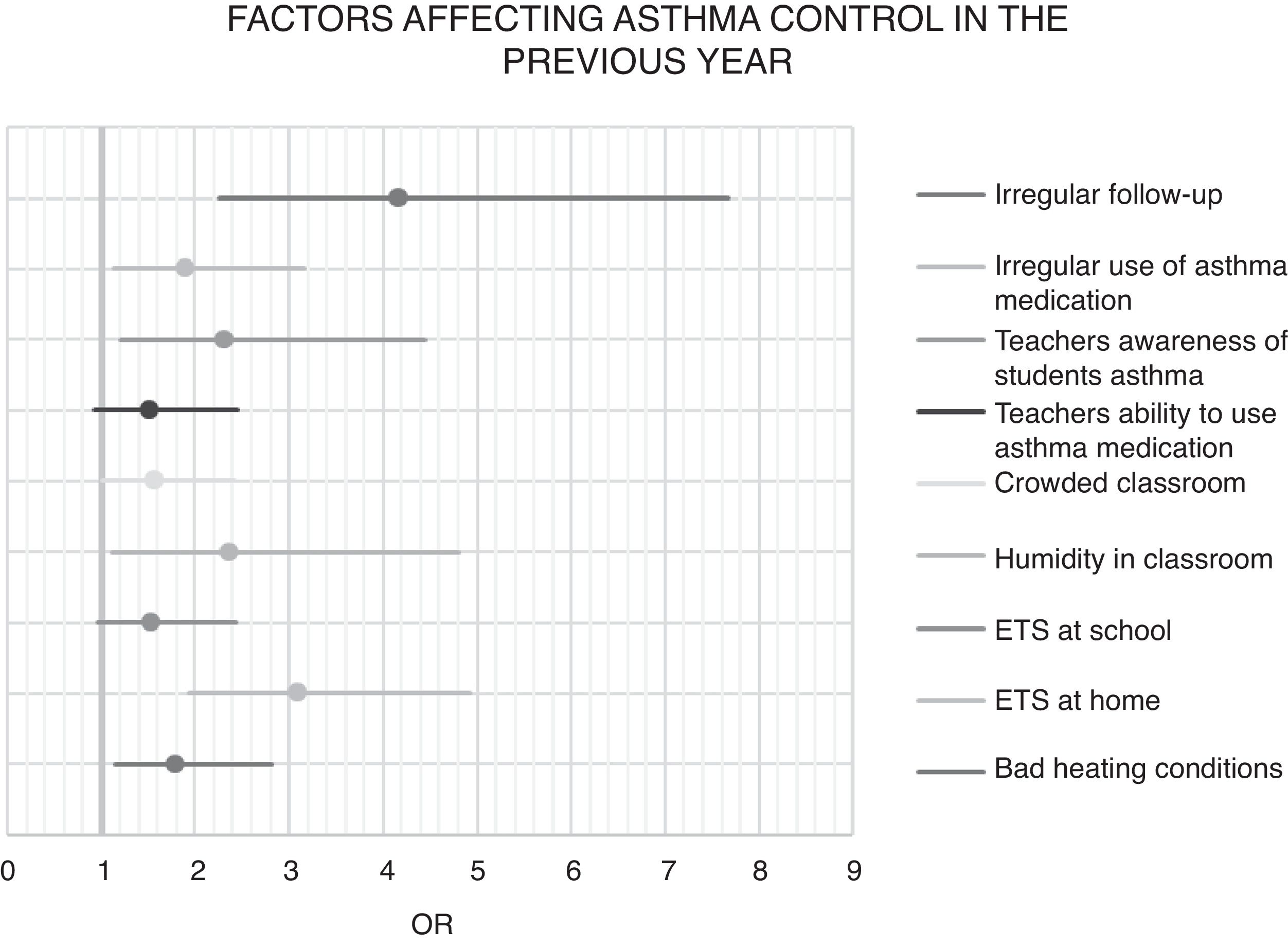
Results507 patients were included. Asthma control status was found to be effective on school absence (p < 0.001), on school success (especially math scores) (p < 0.001), on friend relations (p = 0.033), QOL (p < 0.001), attendance to school activities (p < 0.001). Regular follow-up (p < 0.001), regular use of asthma medication (p = 0.014), tobacco smoke exposure (p < 0.001), heating with stove at home (p = 0.01) affected asthma control. School conditions such as crowdedness (p = 0.044), humidity of the class (p = 0.025), knowledge of teacher about child’s asthma (p = 0.012) were effective on asthma control independent of home conditions and asthma treatment parameters.
ConclusionSchool interventions are important to improve asthma management.
Asthma is one of the most common chronic diseases of childhood. Global prevalence is between 11–14% for school-age children.1 The disease causes a burden on physical health of the children but also lowers the quality of life for both children and their families.2 Psychosocial problems may also be involved and need attention3. In this context, asthmatic children at school age needs special consideration. Their asthma does not only affect their physical health and life at home, it also causes negative conditions about school life.
Studies have shown that school absenteeism is more frequent among asthmatic children and this seems to have a detrimental effect on their school performance.4 Studies were generally concerned with all types of school absence, not only absence due to asthma. Furthermore, absence was considered as any absence and the number of days was not classified according to their possible effect on school life. It is accepted that missing 5% of the school year for any reason is associated with a higher risk for developing future chronic absenteeism, as well as lower proficiency in educational outcomes in later grades.5 A recent study reported that absence due to asthma over nine days was significantly higher for younger children, lower-income families, children with greater asthma severity and poorer control.6
Whether academic achievement is lower among asthmatic school children than their peers, free from the effects of school absence, is not clear. Studies report contradictory results and in part this may be because they are conducted among populations from different cultures and socioeconomic classes and use different methods to define asthma and measure school success.4 According to recent reports, urban children and children with more severe disease may be worse effected in terms of school achievement.7,8
Besides academic achievement, another important part of school functioning is the child’s relation with friends and joining in physical and social activities in school. Asthma may interfere with this side of school life too. Overall, physical and psychosocial quality of life must also be considered when we evaluate the school functioning of asthmatic children.9
Although there are studies about the detrimental effects of asthma on school life, there is only little data about the factors changing this effect. Besides the state of the disease and home conditions, school conditions may influence the school functioning of asthmatic children. Learning about the relation between these three parameters and school life may help us to develop preventive measures and support asthmatic children better. The aim of this study is to evaluate the factors influencing the effect of their disease on school functioning for asthmatic school age children.
Materials and methodsSeven pediatric allergy centers from six cities participated in the study. From January 2019 to May 2019, children aged 6–18 years who were followed by a diagnosis of asthma for more than one year in the participating pediatric allergy clinics were included in the study. Informed consent was taken from study participants and the study was approved by the Institutional Ethics Committee of Ankara City Hospital.
Power analysis using school success and school absence could not be done because a statistical data on these variables was not present in our country. So we made a power analysis using the prevalence of asthma in our country, and taking the prevalence of the variable 50% and we reached 384 for 95% confidence interval.
Age, gender, and atopy status of the patients were recorded from the hospital records. Patients and parents were given a standard questionnaire and a pediatric quality-of-life questionnaire was filled out by children. They were also questioned for the number of days they were absent from school due to asthma in the previous year and their passing scores, math scores and Turkish lesson scores in the previous year. Scores are given from 0 to 5 during primary school and from 0 to 100 during secondary and high school in our country. In order to make the statistics possible for the whole study group, marks of children from secondary and high schools were recorded from 0 to 5 (85–100 as 5, 70–84 as 4, 55–69 as 3, 45–54 as 2 and 0–44 as 1). Grades lower or equal to 3 were considered as “low success” and grades 4 or higher were considered “good success”.
The standard questionnaire included questions about their disease, home and family conditions and school conditions. Parameters questioned about the disease were regular use of asthma drugs, regular follow-up visits, number of any asthma exacerbations and exacerbations needing systemic steroids. Patients were considered to have inadequate control for the previous year if they had more than two exacerbations and/or any exacerbation needing systemic steroids. Control of asthma at the time of attendance was determined according to Global Initiative for Asthma (GINA) criteria.10
Parameters questioned about family and home conditions were mother and father education, family income (lower or higher than 3000 Turkish lira), number of people living (crowded if >4), heating status (stove or central heating), exposure to tobacco smoke (ETS), presence of wool, humidity, animals, cockroach at home.
Parameters questioned about school conditions were ETS, environmental air pollution, number of students in the class (>30 was considered crowded class), cleanliness, airiness and presence of humidity in the class. Whether they thought their asthma effected their academic achievement, whether their asthma worsened during school time, and if so, what the condition worsening their asthma was noted. Whether their teachers knew about patients’ asthma and how to use their asthma medication was also questioned. Attendance status of the patients to activities during school time and activities outside school were recorded.
Pediatric quality of life inventoryThe Pediatric Quality of Life Inventory™ (PedsQL™) 4.0 is a quality of life (QOL) scale designed by Varni et al. in 1999.11 It is suitable for application both to healthy and sick children of different age groups, such as 2- to 4-year-olds, 5- to 7-year-olds, 8- to 12-year-olds, and 13- to 18-year-olds. It consists of a generic core questionnaire with 23 items in five subscales: physical (eight items), emotional (five items), social (five items), and school functioning. The response scale is a 5-point Likert scale. The items are reverse scored between 0 and 100, where the answer “0 = never a problem” scores 100 and “4 = almost always a problem” scores 0, so that the higher the total PedsQL™ 4.0 score, the better the health-related quality of life (HRQOL). The inventory is validated for Turkish.12,13 As there is not a well-defined cut-off for this inventory, we defined children having a score under median as having “lower quality of life”.
Statistical analysisAll analyses were performed using the SPSS Statistics for Windows, version 25.0 (IBM Corp, Armonk, NY, USA). Descriptive statistics were expressed as mean ± SD or median (minimum-maximum) for continuous variables and as case numbers and percentage for nominal variables. The values were presented as medians and interquartile ranges (IQR) for the data that do not show a normal distribution. Differences between the groups were compared by Student’s T test or Chi-square as appropriate. Logistic regression analyses were performed to determine the risk factors for school absence, school success, quality of life and asthma control status. Variables in the univariate analysis at a p value of <0.2 were included in the multivariate logistic regression models. A backward likelihood ratio modeling strategy was used. The size of the effect of each risk factor was given using the odds ratios (ORs) and 95% confidence intervals (CIs). All variables used in the models were added at the same level. A p-value of ≤0.05 was considered statistically significant
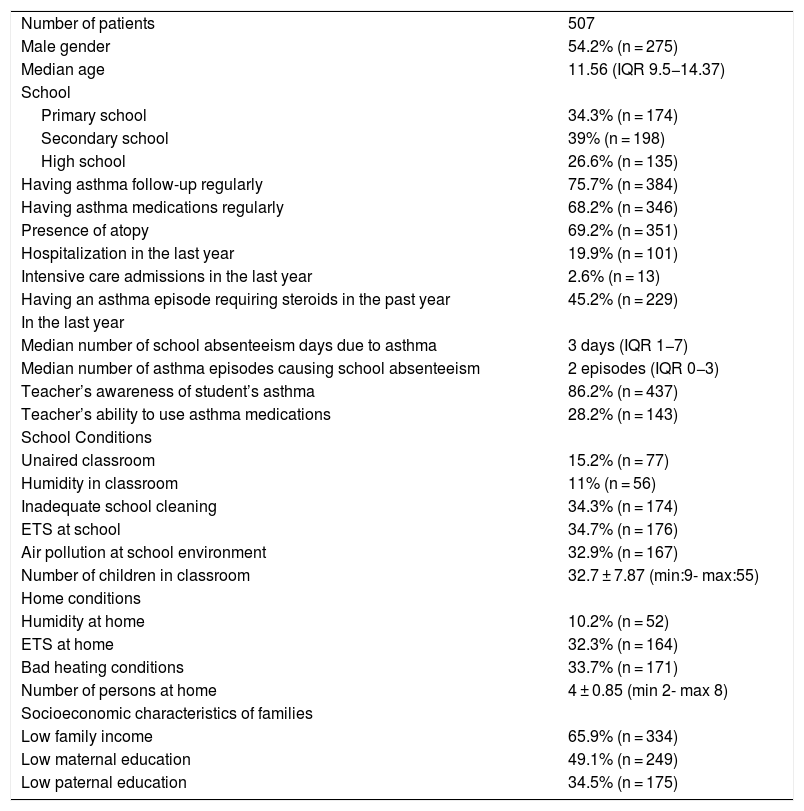
ResultsDuring the study period, 507 patients were included in the study. Median age was 11.56 years (IQR 9.5−14.37) and 54.2% were male. Of the children, 34.3% were educated in primary school, 39% were in secondary school and 26.6% were in high school. The characteristics of the patients are given in Table 1.
Characteristics of patients.
| Number of patients | 507 | |
| Male gender | 54.2% (n = 275) | |
| Median age | 11.56 (IQR 9.5−14.37) | |
| School | ||
| Primary school | 34.3% (n = 174) | |
| Secondary school | 39% (n = 198) | |
| High school | 26.6% (n = 135) | |
| Having asthma follow-up regularly | 75.7% (n = 384) | |
| Having asthma medications regularly | 68.2% (n = 346) | |
| Presence of atopy | 69.2% (n = 351) | |
| Hospitalization in the last year | 19.9% (n = 101) | |
| Intensive care admissions in the last year | 2.6% (n = 13) | |
| Having an asthma episode requiring steroids in the past year | 45.2% (n = 229) | |
| In the last year | ||
| Median number of school absenteeism days due to asthma | 3 days (IQR 1−7) | |
| Median number of asthma episodes causing school absenteeism | 2 episodes (IQR 0−3) | |
| Teacher’s awareness of student’s asthma | 86.2% (n = 437) | |
| Teacher’s ability to use asthma medications | 28.2% (n = 143) | |
| School Conditions | ||
| Unaired classroom | 15.2% (n = 77) | |
| Humidity in classroom | 11% (n = 56) | |
| Inadequate school cleaning | 34.3% (n = 174) | |
| ETS at school | 34.7% (n = 176) | |
| Air pollution at school environment | 32.9% (n = 167) | |
| Number of children in classroom | 32.7 ± 7.87 (min:9- max:55) | |
| Home conditions | ||
| Humidity at home | 10.2% (n = 52) | |
| ETS at home | 32.3% (n = 164) | |
| Bad heating conditions | 33.7% (n = 171) | |
| Number of persons at home | 4 ± 0.85 (min 2- max 8) | |
| Socioeconomic characteristics of families | ||
| Low family income | 65.9% (n = 334) | |
| Low maternal education | 49.1% (n = 249) | |
| Low paternal education | 34.5% (n = 175) | |
The median number of days absent from school due to asthma was three days (IQR 1−7), 20.6% had absence more than nine days. The median number of asthma exacerbations leading to absence was two (IQR 0−3). The mean pass mark was 4.18 ± 0.81, math score was 3.98 ± 0.95 and Turkish score was 4.29 ± 0.79; 22.9% had low success according to general pass mark, 15.4% had low success according to Turkish scores and 29.4% had low success according to math scores. Of the parents, 61.7% thought that asthma has a worsening effect on their child’s achievement.
Of the parents, 36.9% reported that their child’s asthma was worsened at school and 43.8% of the children reported that physical education lesson was the condition when their asthma worsened. Worsening of symptoms when they were prone to irritants such as chemicals and wood shavings during workshops were reported by 21.1%. In 34.3% of the cases, parents thought that the school cleaning was not adequate and 32.9% reported that there was air pollution in the school environment.
According to the questionnaires, 49.9% of the asthmatic children could not attend activities at school (46.2% sometimes and 3.7% never) and 48.8% could not attend outside activities (41.5 sometimes and 6.3% never). Children who could not attend outside activities were 38.6% and 57.5% in groups who had good control and inadequate control during the previous year (p < 0.001). Children who could not attend school activities were 36.5% and 61.3% in groups who had good control and inadequate control during the previous year (p < 0.001).
Mean PedsQL total scale score was 70.81 ± 17.8, physical health summary score was 68.1 ± 21.47 and psychosocial health summary score was 72.24 ± 18.1.
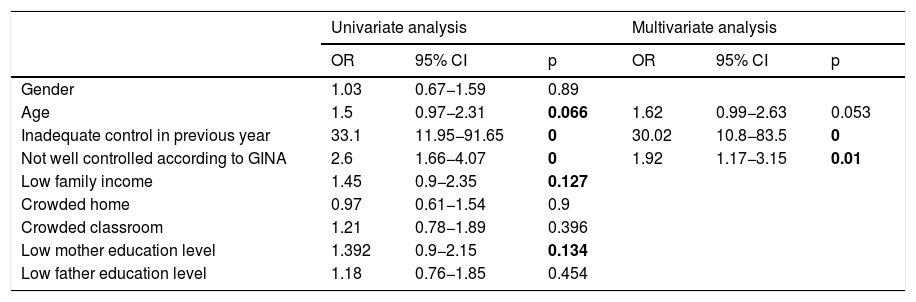
Absence due to asthmaWhen patients who have absences due to asthma for fewer than nine days and nine days and above were compared for age, asthma control in the previous year, asthma control according to GINA at the time of enrolment, low socioeconomic status and lower education of mother were significant in univariate logistic regression. Asthma control in the previous year, and asthma control according to GINA at the time of enrolment were significant in the multivariate logistic regression (Table 2). Inadequate asthma control in the previous year increased the risk of absence >9 days 30 times (OR 30.2 CI 10.8−83.5, p < 0.001)
Factors affecting school absence (>9 days).
| Univariate analysis | Multivariate analysis | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | |
| Gender | 1.03 | 0.67−1.59 | 0.89 | |||
| Age | 1.5 | 0.97−2.31 | 0.066 | 1.62 | 0.99−2.63 | 0.053 |
| Inadequate control in previous year | 33.1 | 11.95−91.65 | 0 | 30.02 | 10.8−83.5 | 0 |
| Not well controlled according to GINA | 2.6 | 1.66−4.07 | 0 | 1.92 | 1.17−3.15 | 0.01 |
| Low family income | 1.45 | 0.9−2.35 | 0.127 | |||
| Crowded home | 0.97 | 0.61−1.54 | 0.9 | |||
| Crowded classroom | 1.21 | 0.78−1.89 | 0.396 | |||
| Low mother education level | 1.392 | 0.9−2.15 | 0.134 | |||
| Low father education level | 1.18 | 0.76−1.85 | 0.454 | |||
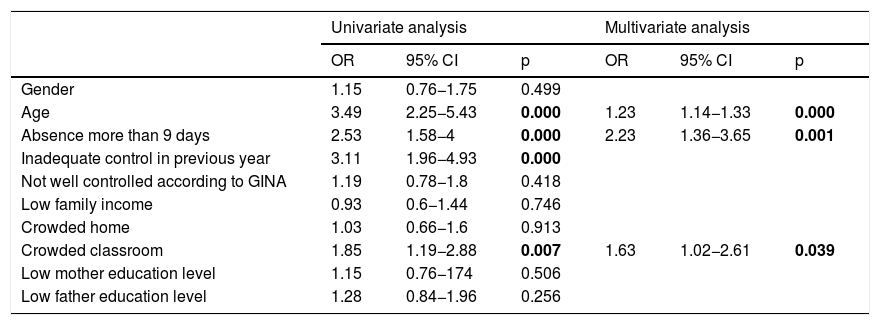
When patients who had low and good success according to pass marks were compared, higher age, having absence more than nine days, inadequate asthma control in the previous year and crowded classroom were significant in the univariate logistic regression. Higher age, having absence more than nine days, and crowded classroom were significant for multivariate logistic regression analysis (Table 3). When we compare math scores; 59.9% of those with inappropriate control in previous year and 83.3% of those with controlled asthma had good success (p < 0.001). Age, absence more than nine days, asthma control, inadequate asthma control in the previous year, not being well controlled according to GINA, crowded classroom, low mother and father education level were significant in the univariate analysis whereas only age (p < 0.001), inadequate control in previous year (p < 0.001) and father education (p = 0.001) were significant in the multivariate analysis. Turkish scores were not different between groups who had and did not have adequate asthma control during the previous year (p = 0.482).
Factors affecting school success.
| Univariate analysis | Multivariate analysis | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | |
| Gender | 1.15 | 0.76−1.75 | 0.499 | |||
| Age | 3.49 | 2.25−5.43 | 0.000 | 1.23 | 1.14−1.33 | 0.000 |
| Absence more than 9 days | 2.53 | 1.58−4 | 0.000 | 2.23 | 1.36−3.65 | 0.001 |
| Inadequate control in previous year | 3.11 | 1.96−4.93 | 0.000 | |||
| Not well controlled according to GINA | 1.19 | 0.78−1.8 | 0.418 | |||
| Low family income | 0.93 | 0.6−1.44 | 0.746 | |||
| Crowded home | 1.03 | 0.66−1.6 | 0.913 | |||
| Crowded classroom | 1.85 | 1.19−2.88 | 0.007 | 1.63 | 1.02−2.61 | 0.039 |
| Low mother education level | 1.15 | 0.76−174 | 0.506 | |||
| Low father education level | 1.28 | 0.84−1.96 | 0.256 | |||
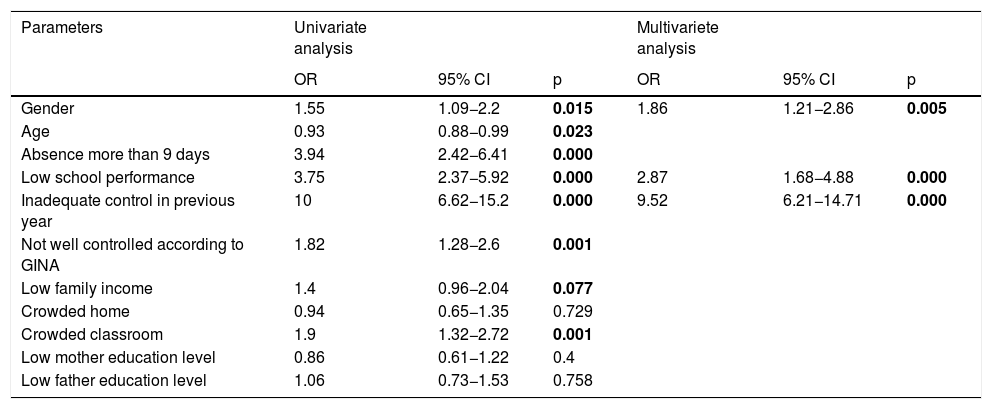
When children who had quality of life scores over and under the population median were compared; higher age, female gender, absence over nine days, lower success, inadequate asthma control in the previous year, lower family income, crowded class were significant in the univariate analysis. Of girls, 51.2% and of boys 48.8% had lower QOL (p = 0.015). In the multivariate analysis, female gender, lower success and inadequate asthma control in the previous year were still significant (Table 4).
Factors affecting quality of life.
| Parameters | Univariate analysis | Multivariete analysis | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | |
| Gender | 1.55 | 1.09−2.2 | 0.015 | 1.86 | 1.21−2.86 | 0.005 |
| Age | 0.93 | 0.88−0.99 | 0.023 | |||
| Absence more than 9 days | 3.94 | 2.42−6.41 | 0.000 | |||
| Low school performance | 3.75 | 2.37−5.92 | 0.000 | 2.87 | 1.68−4.88 | 0.000 |
| Inadequate control in previous year | 10 | 6.62−15.2 | 0.000 | 9.52 | 6.21−14.71 | 0.000 |
| Not well controlled according to GINA | 1.82 | 1.28−2.6 | 0.001 | |||
| Low family income | 1.4 | 0.96−2.04 | 0.077 | |||
| Crowded home | 0.94 | 0.65−1.35 | 0.729 | |||
| Crowded classroom | 1.9 | 1.32−2.72 | 0.001 | |||
| Low mother education level | 0.86 | 0.61−1.22 | 0.4 | |||
| Low father education level | 1.06 | 0.73−1.53 | 0.758 |
When questions of PedQL about relations with peers were evaluated, children who had inadequate control of asthma during previous year more frequently reported they had problems in getting on with peers (3% vs 7.3% p = 0.033) and they had problems in keeping in step with their peers (2.2% vs. 10.2% <0.001).
When questions of PedQL about school life were evaluated, children who had inadequate control of asthma during the previous year more frequently reported they had difficulty in concentrating in the class (9.1% vs. 25.2% <0.001), had difficulty in keeping up with their lessons (4.3% vs. 24.5% p < 0.001) and they forgot things (10.3% vs. 24.8% p < 0.001).
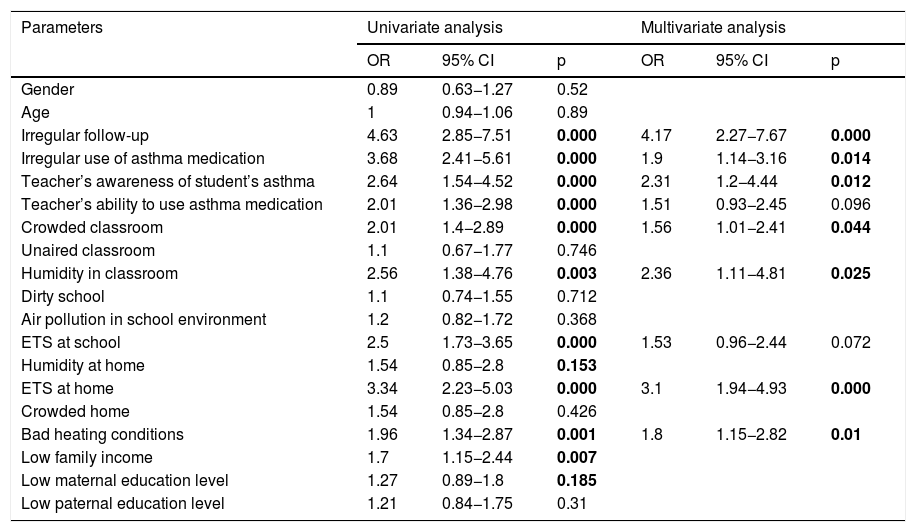
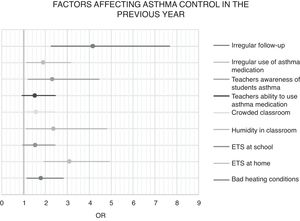
As control in the previous year was a predictive factor for absence, achievement, QOL, friend relations, attendance to school activities and outside activities, we looked for the factors that may have affected control in the previous year. In the univariate analysis, from criteria about the disease, irregular follow-up and irregular drug use were significant; from criteria about family and home conditions, low education level of mother, lower family income, heating with stove, ETS and humidity at home were significant; from criteria about school conditions, classroom more crowded than 30 children, humidity in classroom, tobacco smoke exposure at school and teachers not being informed about child’s asthma and not being capable of using asthma medication were significant. In the multivariate logistic regression, teachers not being capable of using asthma medication, ETS at school, lower income, low education level of mother and humidity at home lost significance and other parameters were still significant (Table 5) (Fig. 1).
Factors affecting control status in the previous year.
| Parameters | Univariate analysis | Multivariate analysis | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | |
| Gender | 0.89 | 0.63−1.27 | 0.52 | |||
| Age | 1 | 0.94−1.06 | 0.89 | |||
| Irregular follow-up | 4.63 | 2.85−7.51 | 0.000 | 4.17 | 2.27−7.67 | 0.000 |
| Irregular use of asthma medication | 3.68 | 2.41−5.61 | 0.000 | 1.9 | 1.14−3.16 | 0.014 |
| Teacher’s awareness of student’s asthma | 2.64 | 1.54−4.52 | 0.000 | 2.31 | 1.2−4.44 | 0.012 |
| Teacher’s ability to use asthma medication | 2.01 | 1.36−2.98 | 0.000 | 1.51 | 0.93−2.45 | 0.096 |
| Crowded classroom | 2.01 | 1.4−2.89 | 0.000 | 1.56 | 1.01−2.41 | 0.044 |
| Unaired classroom | 1.1 | 0.67−1.77 | 0.746 | |||
| Humidity in classroom | 2.56 | 1.38−4.76 | 0.003 | 2.36 | 1.11−4.81 | 0.025 |
| Dirty school | 1.1 | 0.74−1.55 | 0.712 | |||
| Air pollution in school environment | 1.2 | 0.82−1.72 | 0.368 | |||
| ETS at school | 2.5 | 1.73−3.65 | 0.000 | 1.53 | 0.96−2.44 | 0.072 |
| Humidity at home | 1.54 | 0.85−2.8 | 0.153 | |||
| ETS at home | 3.34 | 2.23−5.03 | 0.000 | 3.1 | 1.94−4.93 | 0.000 |
| Crowded home | 1.54 | 0.85−2.8 | 0.426 | |||
| Bad heating conditions | 1.96 | 1.34−2.87 | 0.001 | 1.8 | 1.15−2.82 | 0.01 |
| Low family income | 1.7 | 1.15−2.44 | 0.007 | |||
| Low maternal education level | 1.27 | 0.89−1.8 | 0.185 | |||
| Low paternal education level | 1.21 | 0.84−1.75 | 0.31 | |||
Previous studies about the effects of asthma on school functioning were generally focused on academic achievement and school absenteeism and compared children with asthma to healthy children. Only a few studies have evaluated the factors about asthma that are negatively affecting school functioning. We have settled our study for investigating these factors and added parameters such as quality of life, friend relations and attending to school activities as part of school functioning. This study has revealed that inadequate control of asthma may cause higher absenteeism and may interfere with academic achievement of asthmatic school children. Children with inadequate control also had lower quality of life, had problems in their relations with peers more frequently and could attend school activities less frequently. School conditions such as ETS, humidity in the classroom, crowded classes, and teacher’s awareness of the student’s asthma significantly affected the control of the disease.
Being away from school negatively affects both academic achievement and social interactions of school children. Previous studies have shown that asthmatic children were more frequently absent from school than their healthy peers.4 Most studies have used any absenteeism, not only absence due to asthma and only one defined the status of absenteeism according to its effect on school functioning. Absence over 5% of the school year is considered as a risk for detrimental effects 5 so we considered absence due to asthma of over nine days as “at risk”. Although greater frequency of absenteeism is well defined for asthmatic children, factors affecting the frequency of absence due to asthma are less studied. Asthma severity was defined as a risk factor in some studies but others did not find such a relation.4,7,8 The definition of severity varied widely among studies. We have used the frequency of asthma exacerbations and presence of exacerbations needing systemic steroids as a measure of asthma control during the previous year because control definition according to GINA gives a perspective of the previous month but we wanted to have an opinion about the whole school year. We have found that children who had inadequate control in the previous year more frequently experienced absence due to asthma longer than nine days; actually inadequate control increased the risk 30 times. Recently, Kim et al. also reported a nearly three-fold risk for school children with uncontrolled asthma to have absence of over nine days.6
Academic achievement of asthmatic school children was also studied yielding contradictory results. Definitions of achievement varied greatly among studies. Some studies used school grades whilst some performed standardized tests for reading and math.4 In some of the studies defining a lower achievement for asthmatic children, absence was considered as the real reason. In a very recent study conducted in 683,716 children, asthmatic children were reported to perform worse in school exams and they concluded that higher absenteeism only partially explained the poorer attainment.14 In our study we have used pass scores of children and found that children with inadequate control in the previous year had lower pass scores than their peers with controlled asthma. Although the effect of control was not significant in the multivariate analysis and this supports the effect of control by leading to absence, we have also found that inadequately controlled children more frequently had difficulty in concentrating in the class and more frequently had difficulty in keeping up with their lessons. Furthermore, math scores were affected by control independent of absence in the multivariate analysis. Providing better asthma control may help to decrease absence and improve academic achievement.
Chronicity and unpredictability of asthma causes a risk for lower quality of life for children with asthma. We have used PedsQL instead because it has a special domain about school life and it also questions relations with friends. When we have evaluated factors affecting quality of life, female gender, status of success and asthma control during the previous year they were found significant. Girls seem to have a lower quality of life and may need more attention. Better asthma control may help improving QOL.
Asthmatic children may have internalizing behavior problems more often than their peers and they also may experience problems in friend relations.3,15 They may have problems in physical activities and may not be able to attend other school activities inside and outside the school and this may lead to missed opportunities to engage with their peers. In our study asthmatic children infrequently had problems with their peers but they had problems more frequently if they had inadequately controlled asthma. Nearly half of the patients could not attend school activities, and attendance to activities at school and outside were also lower for children with inadequate control.
Besides the effect of asthma control on friend relations, friend relations may also affect asthma control in turn. Children may hesitate to take their medication when they are with their friends for fear of being alienated by their friends. It has been shown that fear of stigmatism is more effective than stigmatism itself.16 As was shown in our study, alienation is not frequent for asthmatic children and patients must be supported to take their medication when needed even if they are among friends. Increasing awareness for asthma among school children may help to solve the problem.
Although there are some studies evaluating the effect of asthma severity and control on absence and achievement, there are only a few mentions about the conditions affecting asthma control in studies about school functioning.4 As control of the disease was related to all aspects of school functioning (absence, achievement, friend relations, attendance to school activities and quality of life), we have evaluated the factors affecting control. Family and home conditions, school conditions and disease characteristics were studied. Besides irregular follow-up, irregular drug use and ETS exposure and stove use at home, humidity and being crowded in the classroom and teacher’s awareness of the patient’s disease were significantly effective in multivariate analysis.
Exposure to allergens in the school environment is important for asthmatic children. Previous studies have shown that schools may have considerable amounts of allergens.17 Humidity in the school is related to mold exposure and has been reported to worsen asthma18,19 Fungal spore levels in the classroom correlated with asthma symptoms and a relief of symptoms on weekends were reported.17 Besides their activity as allergens, mold exposure has immune modulator effects on asthma.19 Longitudinal studies have found improvement by repair of moisture damage.17 Thus it is important to take preventive measures to avoid dampness in the classroom. Moreover, irritants must also be taken into account, as 21% of our patients have reported worsening of asthma with irritants such as chemicals during workshops.
Teachers generally have inadequate information about asthma and do not feel prepared to assist in the management of asthmatic children.20 Teachers of children with inadequately controlled asthma more frequently were informed about their student’s disease in our study. Perhaps families felt a need for help more frequently if they had more problems with the control of the disease. However, teachers of children with good control in the previous year more frequently had the ability to use asthma medication. Our finding supports the idea that being able to get help for medical management at school may improve asthma control. As many children reported that their asthma worsened during physical education lessons, education of teachers of that lesson can be a priority.
Being in a crowded class may increase the transmission of airway infections which are leading triggers of asthma exacerbations. Furthermore, in a crowded class the teacher may have less time to deal with each student and this may have a detrimental effect on the support of the teacher for an asthmatic child.
There may have been students from the same school, and this may have caused an eventual bias and this is a limitation of our study. Further studies in collaboration with the schools may give more detailed information.
The relation between asthma and school is two-sided. School conditions affect asthma control and therefore children’s school functioning. Conditions of classrooms, taking part of the teacher in the management of asthma and awareness of students about asthma may help to improve school functioning. To achieve better asthma control, school children with asthma must be treated and supported with a cooperation of family, medical and school personnel. School conditions must be upgraded to achieve “asthma friendly schools” by the collaboration of medical, educational and governmental authorities.
Funding declarationThere is no funding for the research.
Conflict of interestThe authors have no conflict of interest to declare.