Hyper-IgE syndrome (HIES), also called Job's syndrome, [Online Mendelian Inheritance in Man (OMIM) #147060 and #243700] is a rare primary immunodeficiency disease, with an incidence lower than 1/106,1 not gender related, transmitted as an autosomal dominant or recessive trait with variable expressivity and of unknown etiology.1–3
HIES has been defined as a multisystem disease characterised by: 1) extremely high total serum Immunoglobulin E (IgE) levels; 2) recurrent bacterial infections — mainly respiratory and cutaneous; and 3) pneumonia with pneumatocele formation and other characteristics: eosinophilia, rough facial features (prominent forehead, broad nasal bridge and facial asymmetry), chronic eczematous dermatitis, retained primary teeth, recurrent pathological fractures from minor traumas, hyper-extensibility and scoliosis.2–4
HIES has been diagnosed by its clinical spectrum which is quite variable and in some patients, clinical signs start soon after birth.5,6 Although extremely high levels of total serum IgE (higher than 2,000IU/ml) have been pointed out as a major characteristic of HIES, misdiagnosis during the first months of life is common due to the characteristics of the immune system at this age.5–7
To date there is no explanation for the high production of IgE8–10and even with high levels of total IgE, the association between HIES and allergies is not common.11
HIES patients have recurrent infections mainly from Staphylococcus aureus presenting in the lungs, as hepatic abscesses, adenitis, cellulitis, and osteomyelitis.7,12 Infections by Candida albicans and other fungi have been increasingly reported.13–15 In some patients, the eczematoid cutaneous rash is extensive and spreads to the face similar to atopic dermatitis.5
In this study we report an exclusively breast-fed infant who presents features of HIES and developed atopic dermatitis due to food allergy.
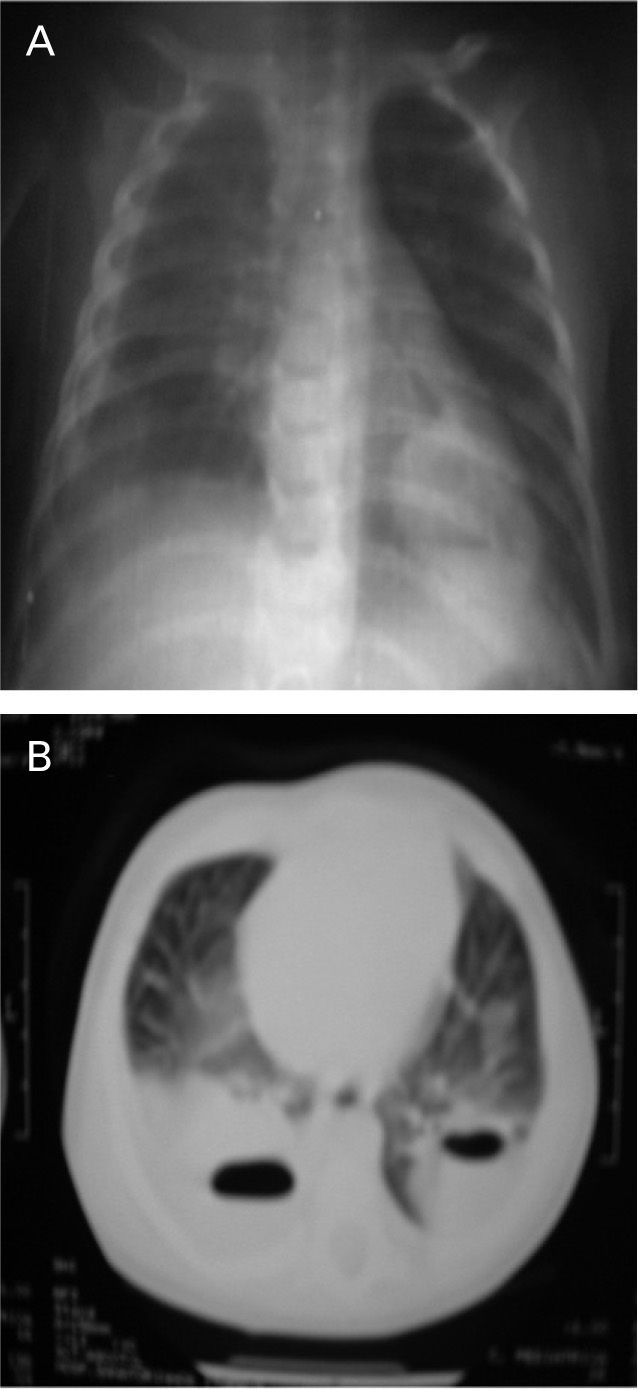
CASE REPORTCJS, 6month-old male, was born by normal delivery (weight = 3.59kg, height = 49cm), was exclusively breast-fed until he was 3months old when he presented a severe bilateral pneumonia complicated by pneumatocele in both lungs (Fig. 1), perineal candidiasis and an infected itching eczema. Eczema was characterized by disseminated and exudative-papule crusted erythematous lesions, mainly on the face and scalp, with excoriations and bleeding secondary to scratching due to the intense pruritus. These lesions did not occur in the nasogenian furrow (Fig. 2).
Patient is the fourth child of non-consanguineous parents and has an older brother who suffers from allergic rhinitis and mild atopic dermatitis.
On admission (aged 3months old), his lab evaluation showed: intense peripheral eosinophilia (17% or 16,000 eosinophils/mm3), total serum IgE = 1,830IU/ml, normal levels of IgA, IgM, and IgG, and normal CD4+ and CD8+ T lymphocyte numbers. Blood culture was positive for S. aureus. When he was 6months old, serum specific IgE (Immuno-CAP®) to whole cow's milk and to egg white were highly positive (class 5). Skin prick test (IPI-ASAC, Brazil®) was positive to whole cow's milk (3mm), beta-lactoglobulin (3mm), egg white (3mm) and soya (3mm).
Despite recommended treatment for atopic dermatitis (hygiene, skin hidratation, and antihistamines) the lesions did not improve. As the child was exclusively breast-fed, food for which he showed positive tests was removed from the mother's diet which resulted in an improvement of the cutaneous lesions. At this time, his diet was supplemented with an amino-acid formula (Neocate®). During his follow-up, when his mother twice broke her diet, the malar eczematous lesions worsened and improved when the diet was restarted. Today he is 12months old and is doing well. Patient did not present any severe infections after treatment with sulphamethoxazole/ trimethoprim.
DISCUSSIONDiagnosis of HIES in infants is difficult. The absence of a specific test makes this diagnosis a puzzle, requiring an accumulation of symptoms that develop over years of follow-up.1 The HIES group of the National Institute of Health elaborated a clinical score based on 19 characteristics in order to make HIES diagnosis simpler. A total score of at least 15 is extremely suggestive of HIES.3 According to these criteria our patient had a score of 33 (high levels of total serum IgE = 1,830IU/ml [8 points]; pneumatocele [8 points], peripheral eosinophils = 16,000/mm3 [6 points], severe eczema [4 points]; young-age correction [7 points]).
The typical HIES cranium-facial features and dental changes are impossible to observe in the first years of life and as they become evident as the child grows up, a periodic reassessment of these criteria is required to confirm diagnosis. Despite the high susceptibility to infections, the exact immune defect remains undetermined. Individuals tend to have frequent staphylococcal abscesses and pneumonias early in life, often developing pneumatocoeles that predispose them to later fungal and Gram-negative bacterial infections.16 Although different aspects of the syndrome were studied and impairment in both innate and adaptive immune response were shown.10,17,18 There is not a specific lab test to confirm diagnosis.
The incident that led us to suspect HIES was the fact that the patient was exclusively breast-fed and did not present any risk factor for developing a severe pulmonary infection. The presence of pneumatoceles suggests Staphylococcus aureus as the etiologic agent which was isolated in his blood culture. It is well known that breastfeeding is related to a reduction of infection in infants.
Atopic dermatitis generally appears after 2months of life in patients with a positive family history of atopy, skin colonisation by S. aureus is common and usually if infected, is not severe.19 In contrast, infections in HIES patients are frequently severe, caused by gram-positive and negative organisms as well as fungi.7,20 Cutaneous rashes start early on and resemble classic atopic dermatitis but they may have distinctive features.6,11,20–22
In the neonatal period, a vesiculo-pustular skin eruption is present in around 80 % of hyper-IgE-syndrome patients, often starting on the face, which may be confused with neonatal acne.23 After the neonatal period, skin findings include retro auricular fissures, external otitis, infected dermatitis of the axillae and groin, folliculitis of the upper back and shoulders, cutaneous abscesses, mucocutaneous candidiasis, and in some patients pitted scarring of the face.6 On occasions, a skin biopsy is necessary to help in differentiating them from each other.21,24
When our patient was diagnosed as having food allergy, his mother's diet was controlled, this procedure allied to antibiotics promoted a significant improvement of his eczema. It has been reported that up to 30 % of atopic dermatitis patients have clinical manifestation related to food allergies and could benefit from the exclusion of these foods from their diet. However, the gold standard for food allergy diagnosis is careful history taking, screening by skin prick allergy test, and/or serum specific IgE to food, followed by the double-blind, placebo-controlled food challenge (DBPCFC).19
Our patient was not submitted to this classical test but it happened indirectly when his mother twice broke her diet which worsened his eczema and was followed by an improvement when the mother again restarted dietary restriction. An interesting point is that the patient was exclusively breast-fed and we could speculate that sensitisation to cow's milk, egg whites and soya occurred from the human milk. It is well known that even small amounts of food eliminated through human breast milk can sensitise high risk subjects.25,26
The frequency of allergic diseases, mainly cow's milk allergy, among HIES patients is unknown.11 Distinguishing between food allergy and HIES in infants is often difficult. Hernandez-Trujillo et al. reported a HIES patient with growth retardation due to cow's milk allergy diagnosed by the identification of serum specific IgE to cow's milk and confirmed by double-blind placebo-controlled cow's milk challenge. There was a substantial improvement in this patient after cow's milk was eliminated from his diet and an extensively hydrolysed formula was initiated.11
In patients with a diagnosis of HIES and severe atopic dermatitis with poor response to the usual treatment, investigation of food allergies is mandatory, even in those exclusively breast-fed.