Influenza is an infectious disease, dangerous for all people, especially for some risk groups such as patients with chronic diseases and health care workers. But most of the people under the risk of influenza, including health care workers are not immunised because of misinformation. In this study, we aimed to determine the knowledge, beliefs and attitudes of patients with allergic rhinitis and asthma and parents of such children related to influenza vaccination. Attitudes and beliefs of physicians treating these patients about influenza vaccination were also investigated.
MethodsTwo different questionnaires consisting of various items related to influenza vaccine were distributed to physicians and patients and parents of children with asthma and allergic disease.
ResultsThe physicians group consisted of 189 physicians from various branches. About one third of physicians from various branches reported that they did not believe the vaccine's effectiveness. Most of the participating physicians did not immunise themselves with influenza vaccination despite the fact that any patient of theirs had died due to influenza infection.
Although nearly half of the 183 patients had been vaccinated with influenza vaccine, only 27% of adults and 11.7% of children had been vaccinated annually.
ConclusionsAsthmatic patients are not immunised regularly with influenza vaccine due to misperceptions about vaccine effectiveness and fear of adverse effects. Another important reason of this is that most the physicians caring for these patients neither immunise themselves nor recommend the vaccine to their patients.
Influenza (flu) is an infectious disease caused by an influenza virus and yearly outbreaks lead to three to five million cases of severe illness and about 250,000–500,000 deaths.1 Therefore, influenza vaccination is the most effective strategy for prevention of influenza virus infection and its complications, such as pneumonia. The World Health Organisation (WHO) recommends annual vaccination for nearly all people over the age of six months-especially pregnant women, children between six months and five years of age, those with chronic diseases and healthcare workers.2 Despite these facts, anti-vaccination movements lead to the fear of people from the vaccines due to misinformation.3 Unfortunately, some doctors and health care workers are also affected by this negative propaganda and neither immunise themselves nor recommend it to their patients.
In this study, we aimed to determine the knowledge, beliefs and attitudes of patients with allergic rhinitis and asthma and parents of such children related to influenza vaccination. Attitudes and beliefs of physicians treating these patients about influenza vaccination were also investigated.
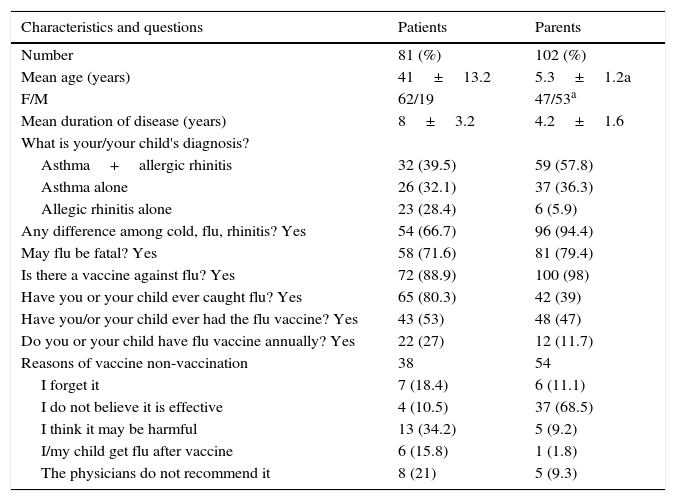
Materials and methodsIn the first part of the study, a questionnaire was distributed to various physicians who take care of allergic and asthmatic patients in their daily practice. The questionnaire consisted of 12 items regarding the physicians’ demographic characteristics, personal qualifications, influenza vaccination recommendations and beliefs and attitudes towards effectiveness and side effects of influenza vaccine. In the second part of the study another questionnaire containing 12 items regarding their (and their children's) clinical diagnoses and knowledge and attitudes related to influenza vaccine were distributed to patients and parents of patients (Table 2). All of the questionnaires were to be filled out on sight.
The study protocol was approved by the Ethics Committee of Sisli Etfal Teaching and Research Hospital, Istanbul.
Statistical analysisWe first performed descriptive analysis of the demographic and health variables potentially affecting the influenza vaccination rate. We used chi-square test to compare categorical variables and z-test for independent proportions to compare the proportions. A P value less than 0.05 was considered statistically significant.
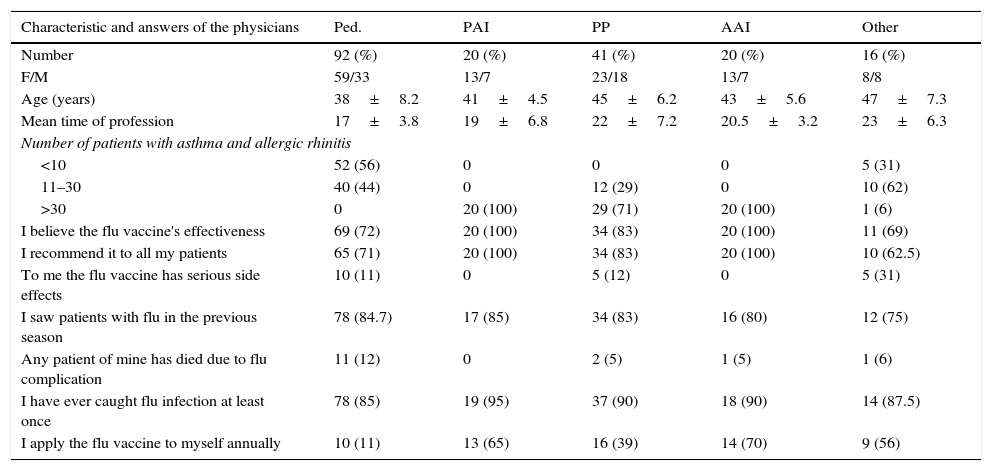
ResultsThe physicians group consisted of 189 physicians from various branches most of whom were paediatricians and pulmonary physicians (Table 1). Nearly all the physicians who specialised in allergy and asthma care believe in the effectiveness of flu vaccine, but 30% of general paediatricians and physicians from other branches did not believe in the vaccine's effectiveness. Most of participating physicians did not immunise themselves with influenza vaccination, despite the fact that no patient of theirs had died due to influenza infection (Table 1). Although a significant portion of respondents from physicians group said they had seen patients with influenza in the previous influenza season, some of them recommended the influenza vaccine only to those patients with serious diseases (Table 1).
Demographic and professional characteristics and answers to the questions of physicians from various branches related to influenza vaccination.
| Characteristic and answers of the physicians | Ped. | PAI | PP | AAI | Other |
|---|---|---|---|---|---|
| Number | 92 (%) | 20 (%) | 41 (%) | 20 (%) | 16 (%) |
| F/M | 59/33 | 13/7 | 23/18 | 13/7 | 8/8 |
| Age (years) | 38±8.2 | 41±4.5 | 45±6.2 | 43±5.6 | 47±7.3 |
| Mean time of profession | 17±3.8 | 19±6.8 | 22±7.2 | 20.5±3.2 | 23±6.3 |
| Number of patients with asthma and allergic rhinitis | |||||
| <10 | 52 (56) | 0 | 0 | 0 | 5 (31) |
| 11–30 | 40 (44) | 0 | 12 (29) | 0 | 10 (62) |
| >30 | 0 | 20 (100) | 29 (71) | 20 (100) | 1 (6) |
| I believe the flu vaccine's effectiveness | 69 (72) | 20 (100) | 34 (83) | 20 (100) | 11 (69) |
| I recommend it to all my patients | 65 (71) | 20 (100) | 34 (83) | 20 (100) | 10 (62.5) |
| To me the flu vaccine has serious side effects | 10 (11) | 0 | 5 (12) | 0 | 5 (31) |
| I saw patients with flu in the previous season | 78 (84.7) | 17 (85) | 34 (83) | 16 (80) | 12 (75) |
| Any patient of mine has died due to flu complication | 11 (12) | 0 | 2 (5) | 1 (5) | 1 (6) |
| I have ever caught flu infection at least once | 78 (85) | 19 (95) | 37 (90) | 18 (90) | 14 (87.5) |
| I apply the flu vaccine to myself annually | 10 (11) | 13 (65) | 16 (39) | 14 (70) | 9 (56) |
Ped, paediatrician.
PAI, paediatric allergist/immunologist.
PP, pulmonary physician.
AAI, adulthood allergist/immunologist.
Other, physicians from other branches.
The second part of the study consisted of 81 adults and parents of 102 children (Table 2). Most of the patients from both groups had both asthma and allergic rhinitis. Although nearly half of the patients had been vaccinated with influenza vaccine, only 27% of adults and 11.7% of children had been vaccinated every year. The reasons for not being vaccinated were fear of side effects and scepticism about efficacy (Table 2).
Answers to the questions of patients or parents related to influenza vaccination.
| Characteristics and questions | Patients | Parents | |
|---|---|---|---|
| Number | 81 (%) | 102 (%) | |
| Mean age (years) | 41±13.2 | 5.3±1.2a | |
| F/M | 62/19 | 47/53a | |
| Mean duration of disease (years) | 8±3.2 | 4.2±1.6 | |
| What is your/your child's diagnosis? | |||
| Asthma+allergic rhinitis | 32 (39.5) | 59 (57.8) | |
| Asthma alone | 26 (32.1) | 37 (36.3) | |
| Allegic rhinitis alone | 23 (28.4) | 6 (5.9) | |
| Any difference among cold, flu, rhinitis? Yes | 54 (66.7) | 96 (94.4) | |
| May flu be fatal? Yes | 58 (71.6) | 81 (79.4) | |
| Is there a vaccine against flu? Yes | 72 (88.9) | 100 (98) | |
| Have you or your child ever caught flu? Yes | 65 (80.3) | 42 (39) | |
| Have you/or your child ever had the flu vaccine? Yes | 43 (53) | 48 (47) | |
| Do you or your child have flu vaccine annually? Yes | 22 (27) | 12 (11.7) | |
| Reasons of vaccine non-vaccination | 38 | 54 | |
| I forget it | 7 (18.4) | 6 (11.1) | |
| I do not believe it is effective | 4 (10.5) | 37 (68.5) | |
| I think it may be harmful | 13 (34.2) | 5 (9.2) | |
| I/my child get flu after vaccine | 6 (15.8) | 1 (1.8) | |
| The physicians do not recommend it | 8 (21) | 5 (9.3) | |
Despite extraordinary successes, such as the eradication of smallpox, some people still have doubts about the benefits of vaccines and worry over their safety. Ironically, doubts about the vaccines and anti-vaccine attitudes are more common in developed countries and among the high socio-economic groups of these countries.3 The Advisory Committee on Immunisation Practices recommends that all health care personnel (HCP) be vaccinated annually against influenza.1 There are two important reasons for this: First, vaccination protects the health care workers against influenza,4 and the second is that influenza vaccination of health care workers reduces illness and mortality among patients.5 However, the coverage of influenza vaccination among HCP is about 42% even in countries with aggressive immunisation programs.6 In Srinagar, India only 4.4% of HCP had ever received influenza vaccination, although they believed that influenza poses adverse potential consequences for themselves or their contacts due to similar reasons in our physician study group.7
Although the infection rate of influenza viruses is high in all age groups, the frequency of isolation of influenza viruses and the burden of infection is highest in young children.8 Influenza and pneumonia result in 20,000 deaths each year in the United States and paediatric mortality from influenza is typically higher in the first year of life than older ages.9 Children with chronic pulmonary (including asthma), cardiovascular, renal, hepatic, haematological, or metabolic disorders are under higher risk for influenza complications. Some studies of children with asthma have demonstrated that up to 63–80% of exacerbations of wheezing or asthma in children are caused by viral infection10,11 and it is estimated that 8% of asthma exacerbations are caused by influenza.12 So, annual influenza immunisation is widely recommended for children with asthma.1 Despite the fact that paediatricians are the physicians who most commonly encounter influenza-infected patients, only 11% of paediatricians from our study group immunise themselves with influenza vaccine and 71% recommend it to the patients. In contrast, all of the paediatric and adult allergy-immunology specialists recommend the influenza vaccine. The rates of recommendation of the vaccine to patients and application to themselves are higher among pulmonary physicians (83%, 39%, respectively) than other specialists such as internists. We think this may be due to the fact that, although they accept the effectiveness of the influenza vaccine, they do not consider themselves under the risk of severe influenza infection. In Turkey, most of the asthmatic adults are diagnosed and treated by pulmonary physicians and adult allergy and immunology specialists.
Unfortunately, in recent years some vaccines, such as the influenza vaccine are perceived as unsafe and unnecessary by a growing number of persons13 and anti-vaccination ideas have spread over the time with the contribution of misleading Internet sites and television programmes. For example, concerns regarding the safety and usefulness of influenza vaccine have increased with contribution of TV programmes during the swine and avian virus outbreaks a few years ago.
Overall vaccination coverage is very high for routine vaccines in Turkey and the incidences of vaccine preventable diseases have declined dramatically in recent decades. In our country, like other developing and developed countries, asthma is a common disease and nearly 5% of adults and 8% of children suffer from it.14,15 Despite the asthmatic patients or parents of asthmatic children knowing that influenza is a serious disease and may be fatal, only 27% of adults and 12% of asthmatic children are vaccinated annually. In our study group, the leading reasons for vaccine refusal are concern about the safety and effectiveness of the vaccine. Another reason is that they think they might get the flu infection from the influenza vaccine. Some rare and mild side effects of influenza vaccine (such as headache, fever, nausea) are being attributed to the vaccine. An interesting finding in our study was that fewer parents think the vaccine to be harmful than the adult patients themselves. This may be due to persuasion of the parents on the benefits of the influenza vaccine and recently applied routine childhood vaccines remembered as “non-harmful” by the parents. Another important reason for non-vaccination of the patients is that their physicians do not recommend the vaccine.16 This may partly be due to excessive patient numbers in the outpatient departments of our hospitals. In spite of their heavy workload, the physicians should spare some time for their patients and explain the risks and benefits of the influenza vaccine at least once in the vaccination season.17 Unfortunately, some physicians underestimate the importance of vaccination for various reasons. Trust of patients and parents to the physicians is also very important to decrease the concerns of the people about the vaccines.18
In conclusion, in spite of recommendations for annual influenza vaccination, asthmatic patients are not vaccinated sufficiently due to misperceptions of influenza and its risks. In addition many physicians neither immunise themselves nor recommend the vaccine to their patients. Therefore, both physicians and asthmatic patients and parents of such children should be trained on the advantages of influenza vaccine, to increase vaccination rates.
Ethical disclosuresConfidentiality of dataThe authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Protection of human subjects and animals in researchThe authors declare that no experiments were performed on humans or animals for this investigation.
Conflict of interestThe authors have no conflict of interest to declare.