At present, the use of palladium (Pd) is very common in nickel-free jewellery and since its introduction in 1973, the use of this metal has increased significantly1. Pd is also present in dental and electrical appliances, jewellery, chemical catalysts and as an automotive emission-control catalyst2.
The aim of our work is to evaluate the prevalence of sensitisation to Pd over a 5-year period and to study the clinical relevance of this sensitisation in a University Hospital in Spain.
PATIENTS AND METHODSFrom 1st January 2000 to 31st December 2005, a total of 1092 patients with a suspected diagnosis for contact dermatitis were patch-tested in the Cutaneous Allergy Unit of our Dermatology Department.
Patch tests were performed on all patients using an extended Spanish Research Group in Contact Dermatitis and Cutaneous Allergy (GEIDAC) baseline series that included Pd chloride 1 % in petrolatum (Trolab®Hermal, Reinbek, Germany). The ethical principles for biomedical investigations promulgated by the Helsinki declaration were observed. All patients were tested in an identical manner. The allergens were applied in adhesive strips of epicutaneous test (Curatest®-Lohmann-Rauscher) and fixed with adhesive tape (Omnifix®-Hartmann). Patch tests were applied to a dermatitis-free area of the upper back. Additional patch tests were performed according to the patient's history and personal or occupational exposure. Readings were made after D2 and D4 using the International Contact Dermatitis Research Group (ICDRG) criteria. The results were evaluated according to the standard scoring system recommended by ICDRG. Only allergic reactions were accepted as positive whereas patch test reactions suspicious of an irritant reaction were excluded from analysis. The relevance of positive patch tests was established in relation to the patient's clinical history. Atopic dermatitis was diagnosed according to the criteria of Hanifin and Rajka3.
Statistical analysis was with Pearson's chi-squared test for the table of contingency 2 × 2, with Yates's correction factor and, where necessary, Fisher's exact test. Statistical significance level was taken as P < 0.05, with the odds ratio (OR) and its corresponding confidence interval (CI) at 95 % being calculated where considered necessary. For analysis of age groups, the patients were subdivided into the following age groups: 1–9, 10–19, 20–29, 30–39, 40–49, 50–59, 60–69 and ≥ 70years.
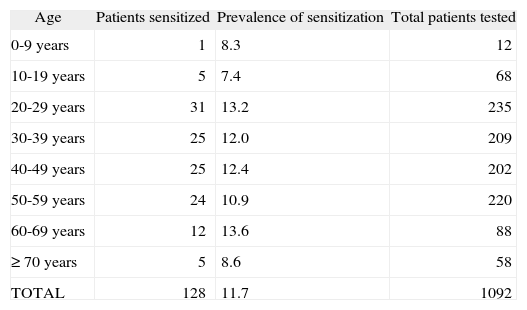
RESULTSDuring the 5-year period studied, we evaluated a total of 1092 patients, 673 (61.6 %) women and 419 (38.4 %) men, with the mean age of all patients being 41.4 ± 16.5years. A total of 128 patients had a positive patch tests to Pd, being 115 (89.8 %) women and 13 (10.2 %) men, with an average age of 40.8 ± 15.3years (range 7–90years). The overall prevalence of a contact allergy to Pd was 11.7 % (17.1 % in females and 3.1 % in males). Individuals sensitised to Pd were significantly more likely to be female (OR = 6.74; 95 % IC: 3.70-12.28; p < 0.000). The prevalence of sensitisation distributed by age groups is shown in Table I.
Distribution of the prevalence of sensitization to palladium grouped by age
| Age | Patients sensitized | Prevalence of sensitization | Total patients tested |
| 0-9years | 1 | 8.3 | 12 |
| 10-19years | 5 | 7.4 | 68 |
| 20-29years | 31 | 13.2 | 235 |
| 30-39years | 25 | 12.0 | 209 |
| 40-49years | 25 | 12.4 | 202 |
| 50-59years | 24 | 10.9 | 220 |
| 60-69years | 12 | 13.6 | 88 |
| ≥ 70years | 5 | 8.6 | 58 |
| TOTAL | 128 | 11.7 | 1092 |
The most frequent localizations of the dermatitis in the patients with a contact allergy to Pd were the hands (30 patients; 23.4 %) and the face (15 patients; 15.7 %). Housewife was the most prevalent occupation (44 patients; 34.4 %) followed by intellectuals (21 patients; 16.4 %) and health care professionals (12 patients; 9.4 %). As an occupational group, the electronics industry workers presented the highest prevalence of sensitisation to Pd (25 %), followed by housewives and health care professionals (22.2 %). 19 (18.8 %) patients and 5 (8.8 %) patients had a personal and a family history respectively for atopy. 96.9 % (124) of patients who were positive to Pd, were also positive to nickel sulphate and 2 (1.6 %) patients showed only a positive reaction to Pd, without a concomitant reaction to a transition metal. Positive tests to Pd were relevant in 96.1 % of the cases.
DISCUSSIONPd, a well-known sensitizer in humans, is a frequent transition metal. Its use has increased significantly in the past decade. When Pd chloride 1 % in pet. is part of the baseline series, the prevalence of sensitisation to Pd ranges between 8 % in Austria4, 9 % in Turkey5 and 13% in Israel6. Nevertheless, no data on Pd allergy were available previously for Spanish populations due to the fact that Pd is not included in the baseline series of GEIDAC7. The prevalence in our study (11.7 %) is similar to that found by other authors.
Due to the increase in the utilisation of Pd and the consequent exposure to this metal, the rates of sensitisation have risen8. The population may be exposed to Pd mainly through dental alloys and nickel-free jewellery. Pd has proved to be a suitable substitute in nickel-free products with the female population being more at risk. This agrees with the results obtained in the present study, where females were significantly more sensitised to Pd.
The relevance of a positive patch test reaction to Pd is likely to be compromised. This can be explained by the fact that a significant number of patients allergic to Pd also showed a positive patch test to nickel sulphate8,9. The evaluation of these subjects allows us to conclude that cosensitisation to nickel is frequent, as many authors have reported6,8. This justifies the high clinical relevance obtained in our study (96.1 %). The simultaneous positive reactions of nickel and Pd are explained by: a) sensitisation to both metals; b) contamination of the Pd patch test material with small traces of nickel, although several studies have not accepted this theory;2,10 and c) nickel and Pd present a similar chemistry with an equivalent electron arrangement, which might be responsible for a true cross-reactivity at the T-cell level9. All positive results in the electronic industry workers group were considered relevant, reflecting how widely distributed this transitional metal is in the electronics world.
Any baseline patch test series must be re-evaluated regularly in order to consider changes in its composition11. We considered that sensitisation to Pd must be studied in the future. In view of the high rates of Pd sensitisation in our area, we think that Pd should be included in the GEIDAC baseline series9.