Apitherapy represents a certain form of complementary and alternative medicine that uses bee products in combination with other methods from this field. One of the basic concepts of this type of medicine is that all diseases can be treated using apitherapy. This study was performed to assess the recommendations from authors of books on apitherapy regarding the treatment of seasonal allergic rhinitis and compare them to findings from the scientific literature.
MethodsOne hundred and twenty-nine books on apitherapy were analysed regarding recommendations for allergic seasonal rhinitis. Scientific evidence regarding the efficacy of using various bee products was searched via PubMed and JUSTfind.
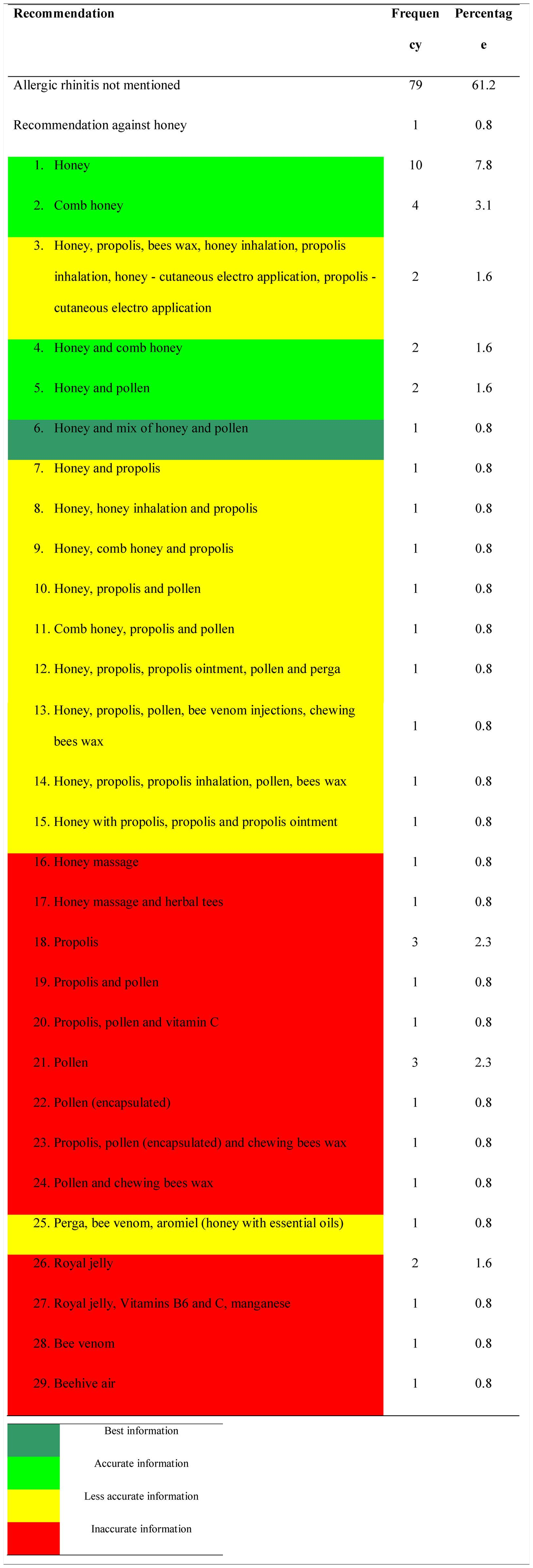
ResultsOnly 38.8% of the apitherapy books mentioned seasonal allergic rhinitis. Among these books, we found 29 different recommendations in favour of bee products and one against the use of honey. The most reasonable recommendation according to clinical studies on the subject, namely the use of a mix of honey and pollen, was only found once (0.8%).
ConclusionsThe large discrepancies and number of different recommendations demonstrate that apitherapy is not a consistent type of medicine. The recommendations regarding seasonal allergic rhinitis in the vast majority of apitherapy books cannot be considered adequate when compared to the scientific findings.
Seasonal allergic rhinitis (SAR) is defined as an immunoglobulin E (IgE)-mediated inflammatory type 1 response of the nasal mucous membranes after exposure to inhaled allergens. Its symptoms include rhinorrhoea, nasal obstruction and blockage, nasal itching and repetitive sneezing; it may be accompanied by allergic conjunctivitis, with symptoms that can include itchy, red, watery and/or swollen eyes.1 Unaffected people may sometimes perceive these symptoms as trivial; however, research on the topic indicates that these conditions have negative and far-reaching impacts on the life of affected people. Both SAR and allergic conjunctivitis have been shown to limit daily activities and functioning in affected individuals. These individuals frequently experience difficulties falling asleep, waking during the night, snoring and poorer sleep quality, all of which negatively impact physical and mental performance, as well as quality of life.1,2 These conditions affect between 10 and 30% of people in Western countries.3 In the United States of America, it is estimated that SAR generates $2–$5 billion in direct health expenditures and is responsible for as much as $2–$4 billion in lost productivity annually.4
With this background, it is clear that an efficient treatment for SAR is crucial in order to avoid the associated expenditures and the related loss in productivity. Treatment options include intranasal and oral formulations of antihistamines, decongestants, corticosteroids, intranasal cromolyn, intranasal anticholinergics and oral leukotriene receptor antagonists. There are general guidelines on what should be used for specific situations.5 Most recent recommendations suggest that patients at least 12 years of age should receive intranasal corticosteroid therapy only because it has been shown that combined intranasal corticosteroid and oral antihistamine therapy are not more beneficial compared to intranasal corticosteroid alone.6 According to an analysis from Spain, the perception of “controlled” rhinitis using these methods was 40%, data which indicate that the majority of cases are uncontrolled.7
Another treatment option is allergen immunotherapy. A recent meta-analysis demonstrated that this modality is effective in improving symptom, medication and combined symptom and medication scores in patients with allergic rhinoconjunctivitis. According to that meta-analysis, some evidence suggests that these benefits are maintained after therapy discontinuation.8
Apart from conventional medicine, a considerable number of patients use methods from the field of complementary, alternative or integrative medicine (CAM). The percentages of patients seem to vary substantially throughout the world – between 7 and 50%, with the highest percentages in Australia, Europe and the United States of America.7,9,10 Similar to other fields of medicine, the percentage of users has increased in recent years.9,10 There are many methods that are used, including dietary and nutritional supplements, herbal medicines, homoeopathy, phototherapy, behavioural and physical techniques and Traditional Chinese Medicine.9 According to the most recent review on the topic, tea therapy, acupuncture, Nigella sativa, cinnamon bark, Spanish needle, acerola, capsaicin (Capsicum annum), allergen-absorbing ointment and cellulose powder are frequently used.11 Again, the prevalence of these methods varies among countries. For example, in Italy, homoeopathy is the main form of CAM used, followed by herbal remedies.12 In Japan, the use of phytotherapy (Ten-Cha, Rubus suavissimus), foods that contain lactic acid bacteria (yogurt) and cedar pollen candy are the most utilised techniques.13
Although there is a multitude of methods that are applied, only a few are recommended. According to a clinical practice guideline, acupuncture may be offered to patients who are interested in non-pharmacologic therapy.4 This recommendation is based on high-quality randomised controlled trials that demonstrated efficacy and effectiveness for acupuncture in the treatment of both SAR and perennial allergic rhinitis.14 Additionally, endonasal phototherapy has proven efficacy.15 On the other hand, herbal therapy is explicitly not recommended, and studies on homoeopathy have a low or uncertain overall quality; thus, they do not allow any conclusions about intervention effects.4,16
Sublingual tablet immunotherapy represents another therapeutic option; current evidence supports the concept that it can be considered an alternative or add-on treatment to pharmacotherapy.17 Similar to sublingual tablet immunotherapy, treatment with honey is frequently suggested by protagonists of apitherapy, a field of complementary and alternative medicine that focuses on treatment options that use various products from the beehive, especially honey, pollen, propolis, royal jelly and bee venom. This review was performed to assess the recommendations of apitherapists with respect to pollen-induced SAR and compare them to evidence from clinical and preclinical studies.
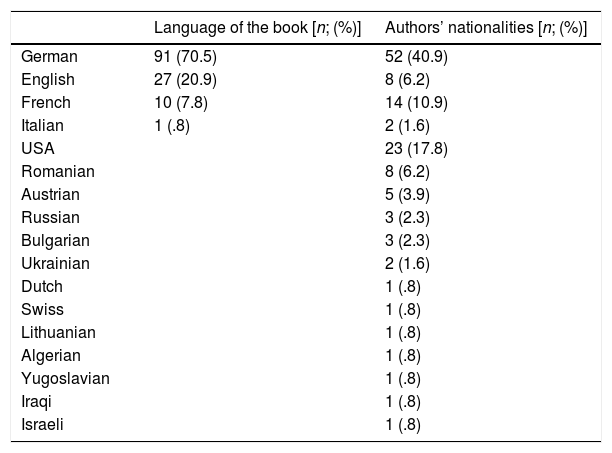
MethodsA systemic analysis of 129 books on apitherapy was performed in order to analyse the current state of apitherapy and determine which therapies are recommended. The analysed books are listed in alphabetical order and provided in a separate file. The languages in which they were published, and the countries of the authors’ origin are shown in Table 1.
Language of the various books and authors’ nationalities.
| Language of the book [n; (%)] | Authors’ nationalities [n; (%)] | |
|---|---|---|
| German | 91 (70.5) | 52 (40.9) |
| English | 27 (20.9) | 8 (6.2) |
| French | 10 (7.8) | 14 (10.9) |
| Italian | 1 (.8) | 2 (1.6) |
| USA | 23 (17.8) | |
| Romanian | 8 (6.2) | |
| Austrian | 5 (3.9) | |
| Russian | 3 (2.3) | |
| Bulgarian | 3 (2.3) | |
| Ukrainian | 2 (1.6) | |
| Dutch | 1 (.8) | |
| Swiss | 1 (.8) | |
| Lithuanian | 1 (.8) | |
| Algerian | 1 (.8) | |
| Yugoslavian | 1 (.8) | |
| Iraqi | 1 (.8) | |
| Israeli | 1 (.8) |
There were no selection criteria for the books. We included all books that we identified and obtained for detailed analyses. One major aspect was that the analysis would include books of all opinion leaders such as former and current presidents of the Apimondia Scientific Commission on Apitherapy and presidents of societies for apitherapy. For this reason, we included one in the Italian language because it was the only book from Dr. Mateescu, the current president of Apimondia's commission on apitherapy.
After analysing all the recommendations on SAR, the results were compared to the findings of scientific studies on bee products. These studies were identified using PubMed and JUSTfind (data search engine of the Justus-Liebig-University Gießen, Germany, which comprises 337 databases from the EBSCO Discovery Service) using the search terms “allergic seasonal rhinitis”, “allergic rhinitis”, “pollinosis” or “hay fever” combined with the names of various bee products. In the next step, the methods that were suggested by apitherapists were compared to results of the scientific literature analysis in order to evaluate the quality of the recommendations.
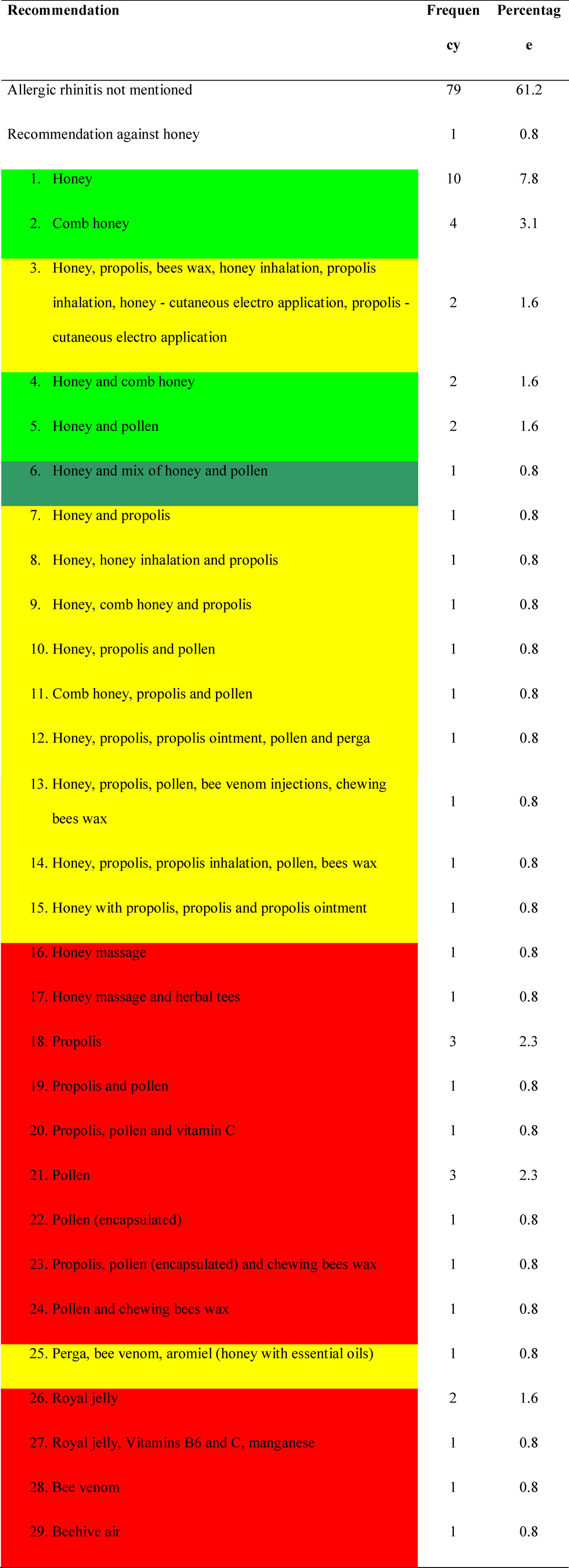
ResultsAnalyses from apitherapy booksTable 1 shows the number of published books, their languages and the country of origin for the various authors. Overall, 50 out of 129 books (38.8%) mention SAR. Among these books, we found 29 different recommendations in favour of bee products and one against the use of honey. Only one recommendation was found four times (administration of comb honey) and only two are supported thrice (administration of pollen). Four recommendations were found twice. The various recommendations are summarised in Table 2. Honey, pollen/perga and propolis represent the most important parts of the treatment because they are mentioned most: 31 times (honey) and 17 times (pollen and propolis). Interestingly, only six books (12%; 6/50) provide information on dosing of the bee products.
Information from the scientific literatureHoneyThe use of honey and pollen is recommended based on the concept of oral desensitisation. Studies have shown that there are common antigens between the pollen from entomophilous and anemophilous flowers.18,19 A case report presented a patient suffering from severe SAR, perennial sinusitis and antihistamine dependence whose symptoms were improved by nutritional supplements, herbal medicines, honey and a low-histamine diet.20 Regarding the efficacy of honey for SAR, six clinical studies proved the concept:
- •
A cohort study of 20 patients reported a response rate of 75%.21
- •
A study of 21 patients who consumed 10–20g of honey per day found a response rate of 76.2%.22
- •
A three-armed prospective randomised trial that comprised 36 patients compared local unprocessed honey (1) to commercial honey (2) and corn syrup (3) and found no evidence for the efficacy of honey.23 However, the conclusions of that study are questionable due to the low number of patients in each arm and the considerable drop-out rates during the trial.
- •
Another cohort study of 23 patients showed that after regular consumption of local honey 12 patients (52.2%) were free of complaints after treatment while in nine patients (39.1%) the situation improved considerably.24
- •
A two-armed randomised placebo-controlled trial compared 1g/kg body weight of honey daily to the same dose of honey-flavoured corn syrup as a placebo. After four weeks, all complaints improved significantly in the treatment group; this benefit persisted for one month after treatment cessation.25
- •
Allergic conjunctivitis, which is frequently associated with SAR, was reportedly improved due to the instillation of a 60% honey solution.26
- •
A study that comprised 353 children revealed that honey with added bee pollen led to a response rate of 69%; however, the treatment was more efficient in children younger than 11 years old.27
- •
Another prospective-randomised trial investigated honey with added birch pollen versus regular honey in 44 patients. All patients in that study were sensitive to birch pollen. Notably, birch pollen added to honey was significantly more efficient than regular honey.28 Thus, it might be advantageous if honey contains relevant antigens.
No study has tested bee-collected pollen for SAR.
Propolis and royal jellyRegarding propolis, we found evidence for treatment effects in animal experimental models.29–31 In one study, a combination of royal jelly and Brazilian green propolis was used.32 All studies presented positive results.
Bee venomBee venom was studied in animal experimental models and showed positive results.33,34 There was also a study indexed in PubMed on the treatment of allergic rhinosinusitis in children with bee venom.35 Unfortunately, we were unable to analyse that study because it was in Russian.
Other bee productsNo information on other bee products (bees wax, honey massage, aromiel, beehive air, etc.) in relation to SAR was found in the scientific literature.
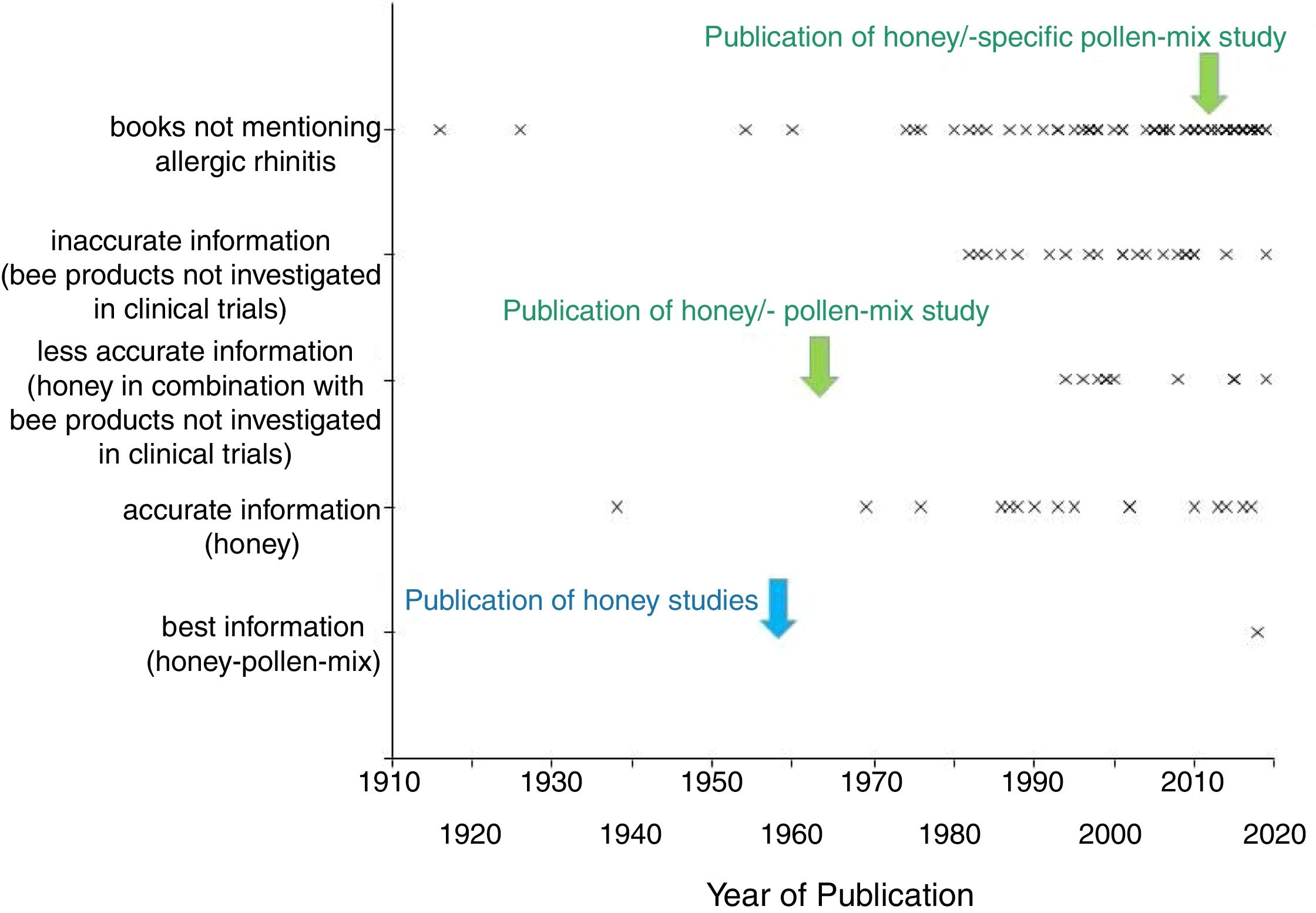
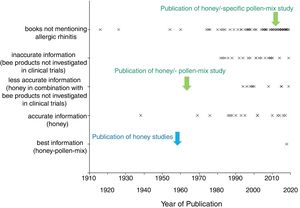
Do apitherapy books use the scientific literature?Fig. 1 depicts the various dates when the books were published based on whether they provide the best information (honey-pollen-mix), accurate information (honey), less accurate information (honey in combination with bee products not investigated in clinical trials), inaccurate information (bee products not investigated in clinical trials) or do not mention the topic. Overall, 39 out of 123 books (31.7%) cite studies from the scientific literature. Among books that refer to SAR, 17 cite scientific literature. However, only one book cites the scientific literature on SAR. The book by Fearnley (2001) refers to a study on propolis and hay fever by Chauvin (1980). The paper was published in a scientific beekeeping magazine (Apiacta). Notably, one book (0.8%) provided the most valid recommendation to use a mix of honey and pollen (based on clinical trials).
DiscussionOur analysis demonstrated that apitherapists present many different recommendations for the treatment of SAR. The fact that only a minority of the books mention the topic cannot be regarded as a problem because some books only focussed on bee products that the author might not have thought suitable for the treatment of SAR. Our comparison of the recommendations and scientific evidence revealed that many recommendations are not based on sufficient scientific evidence because the results of preclinical studies cannot be regarded as sufficient. Even considering recommendations that might rely on animal trials, there are recommendations that totally lack scientific evidence, e.g. honey massage and beehive air. Given that preclinical data from experimental animal models cannot be considered an adequate basis for any recommendation, only honey, pollen or the combination of honey and pollen can be considered an appropriate proposal for an alternative SAR therapy. Several bee products have considerable allergic potential (especially bee venom, royal jelly and propolis), and these substances should not be recommended or recommended only with caution in order to avoid unnecessary side effects.36–38 However, evidence regarding propolis and royal jelly is fairly new. Thus, only few books could have possibly considered the evidence from the animal studies on bee venom, royal jelly and propolis. In all, only 25 recommendations (50%) can be considered reasonable.
Overall, there are several questions associated with apitherapy for SAR:
- 1.
Is the current evidence sufficient to suggest honey and/or pollen for SAR?
- 2.
Can the percentage of adequate recommendations from apitherapists be considered adequate and acceptable?
- 3.
Should therapists consider other methods from the field of complementary and alternative medicine?
As shown, the clinical evidence for honey and/or pollen for SAR is based on only a few clinical studies which all have low patient numbers. However, the fact that the treatment-related response rates ranged from 60 to 75% makes it reasonable to consider further trials on the subject. If patients ask for such treatment, it was suggested that such a treatment should be started slowly and with very small doses in order to avoid allergic reactions.39 It also seems reasonable that in such cases the specific pollen should be added to honey in accordance with the research by Saarinen et al.28
The fact that only one book author justified his recommendations on the basis on a scientific study suggests that apitherapy protagonists do not seem to be interested in adjusting their recommendations to the current knowledge. For example, the two studies on honey and SAR should have been detected by the authors of apitherapy books because they had been published in the 1950s and 1960s and are easily accessible.21,27
This study is the first one that has analysed the topic of apitherapy and SAR. Apart from a review of the current scientific literature on bee products for SAR, the present study has also analysed the recommendations from apitherapy book authors. One limitation for this study is that there was no strategy in the selection of the books. We simply analysed all books that we could find after a careful search on bookseller platforms, multinational e-commerce corporations and the JUSTfind system. Unfortunately, there is no compilation of books on apitherapy, and thus it is impossible to assess whether we missed relevant publications. Another limitation is that we had to restrict this study to books in English, French and German. There may be significant contributions that were published in Spanish, Romanian, Russian and other languages. However, we do not believe that we missed relevant recommendations because much work from Russia, Romania and other countries has been translated into English, French and German. These works come from authors who are considered to be the founding fathers of apitherapy (e.g. Bodog F. Beck and Charles Mraz) or who are international opinion leaders in the field, which are included in our analysis as shown in Table 2.
Regarding whether honey and/or pollen should be used as a treatment option for SAR, other treatment options with better evidence should be considered. As indicated in the introduction, acupuncture and endonasal phototherapy can be considered safe and valid treatment options for patients with SAR.8,14,15 These methods are unlikely to have any risk of allergic reactions and thus both should be preferred over an apitherapeutic approach. Although very rare, there are reports of allergy to honey.39 As indicated by Choi et al., providers of honey therapy must be aware of the potential risk of severe allergic reactions upon ingestion of honey and bee pollen, especially in patients with a pollen allergy.40 However, further studies on honey and/or pollen seem to be justified.
Although there is some evidence that bee-derived honey and/or pollen can be considered efficient treatment options for SAR, further studies seem to be necessary to evaluate the different concepts, namely the use of honey only, pollen only, a combination of honey and unspecific pollen or a combination of honey and a specific pollen.
FundingNone declared.
Conflict of interestNone, except that both authors are hobby beekeepers.