To evaluate the sensitization to aeroallergens determined by skin prick test (SPT) in Brazilian adolescents, and to correlate its positivity with the diagnosis of asthma and/or rhinitis based on the written questionnaire (WQ) of ISAAC phase III study.
Patients and MethodsA total of 996 adolescents (387 boys) were selected by systematic samples. A standard allergen extracts panel (positive/negative control, D pteronyssinus [Dpt], P americana [Pa], B germanica [Bg], dog, cat, fungal and grass mix) was used and its positivity compared with positive responses to asthma, rhinitis or both.
ResultsPositive SPT to at least one allergen was observed in 466 adolescents (46.8 %), with sensitization to Dpt in 79.1 %. Positivity to more than one allergen occurred in 232 students (49.8 %). The frequency of positive SPTs was significantly higher among adolescents with asthma (OR=2.16), rhinitis (OR=1.69), and asthma and rhinitis (OR=2.03). Positive SPT to four or more allergens were higher among asthmatics (OR = 2.6) and among adolescents with asthma and rhinitis (OR=3).
ConclusionsA high sensitisation rate to aeroallergens was observed, significantly higher among those with asthma, rhinitis or a combination of both, especially in multiple sensitisations.
The prevalence of IgE-mediated diseases such as asthma and rhinitis has been markedly increasing in industrialized countries over the last decades. Skin prick test (SPT) have been a valuable tool in the determination of sensitisation to environmental allergens in patients with a suspicion of respiratory allergies. Children attending public schools in large urban centres are exposed to allergens at home and at school, with few data being available regarding sensitisation of adolescents with symptoms of asthma and/or rhinitis to the most common allergens, especially cockroach allergens1.
The confirmation of a possible allergic aetiology of these respiratory diseases is important and will permit a better therapeutic approach. Although controversial, a reduction in the exposure to environmental aeroallergens to which the patients are sensitive has been the therapeutic management defended by most physicians who care for these patients2.
The objective of the present study was to evaluate and compare the frequency of sensitisation to aeroallergens determined by the SPT among adolescents attending public schools in the western region of the city of Sao Paulo and in the town of Nova Iguacu, municipality of Rio de Janeiro, and to determine its correlation with the diagnosis of asthma and/or rhinitis established, based on the written questionnaire (WQ) of the International Study of Asthma and Allergies in Children (ISAAC phase III).
SUBJECTS AND METHODSA total of 1014 adolescents (532 from the western region of the city of Sao Paulo, and 482 from the town of Nova Iguacu, Rio de Janeiro) participated in the study, 621 girls and 393 boys, ranging in age from 12 to 16years (mean = 13.8years and median = 14years). All students participated in ISAAC phase III and were regularly enrolled in the public education network of the two municipalities. The students were randomly and probabilistically selected among those who correctly responded to the ISAAC WQ and who agreed to perform the SPT. In Sao Paulo, the schools studied were municipal and belonged to peripheral urban regions with good public sanitation, although the students were from an underprivileged socioeconomic class, living in shanty towns or precarious dwellings. The municipality of Nova Iguacu is characterized by urban areas, but the Integrated Centers of Public Education (CIEP) are present in regions without asphalt and with poor sanitary conditions, resembling typically rural areas.
The ISAAC phase III WQ was answered by 3181 adolescents (13 and 14years old) from the western region of the city of Sao Paulo and by 3185 adolescents from the municipality of Nova Iguacu, and was concluded in 2002. The ISAAC WQ for 13–14year olds was standardised and validated for the Brazilian culture, and the questions regarding asthma, rhinitis and eczema are mainly related to the symptoms of each of these diseases experienced especially over the past 12 months3–5.
In the western region of Sao Paulo, 21.9 % of the adolescents responded positively to question 2 regarding asthma and 30.1 % responded positively to the question regarding rhinitis, whereas in Nova Iguacu the positive responses were 11.8 and 17.4 % for asthma and rhinitis, respectively.
The SPTs were performed using allergen extracts of the standard battery: positive (10mg/ml histamine) and negative control (0.5 % phenol solution and glycerin solution), Dermatophagoides pteronyssinus [Dpt], Periplaneta americana [Pa], Blattella germanica [Bg], dog and cat epithelia, and a fungal and grass mix. The extracts were provided by Diater (distributed by ALC -Alergia Clínica Laboratorial e Comércio Ltda) and their composition was analysed by ELISA at the Laboratory of the Faculty of Medicine of Ribeirao Preto, Sao Paulo. The presence of Der p 1, Der f 1, Der p 2, Blot 6, Bla g 1, Bla g 2, Fel d 1 and Can f 1 at satisfactory levels was confirmed: Dpt = 2mg/ml; dog epithelium = 5mg/ml; cat epithelium = 5mg/ml; Bg = 2.5mg/ml, and Pa = 2.5mg/ml. The levels of Alternaria (5mg/ml) and Aspergillus (5mg/ml) fungal allergens, pool of airborne fungi (5mg/ml) and wild grass pollen (containing Lolium perenne, 2.8mg/ml) were not quantified.
The SPT was performed by an experienced allergologist using a modification of the Pepys technique6–8, at the school of the selected students after explanation of the exam and previous consent. Disposable individual lancets (Alko do Brasil) were used for each extract, being positioned at a 90° angle to allow each drop to penetrate only 0.1 to 0.2mm into the skin. A positive response was defined as a wheal size equal to or greater than 3mm above the negative control. Those patients who showed no wheal formation in response to the positive control and to none of the allergens tested, or who presented whealing in response to all allergens (dermographism) were excluded from the study.
The data regarding positive responses to the asthma and rhinitis modules of the ISAAC WQ, as well as the mean wheal diameter obtained for each allergen tested, were entered into the database module of the statistic software SPSS (SPSS Inc, Chicago, IL). Differences between proportions were evaluated by the Chi-square test and by Fisher's exact test, when necessary. The Mantel-Haenszel test was used to calculate the odds ratio (OR) and 95 % confidence interval (95 %CI) between the SPT and gender and the presence of asthma, rhinitis or a combination of both. A p value < 0.05 was considered to be significant.
The projects were approved by the Research Ethics Committees of the University Hospital, Sao Paulo University School of Medicine, and Clemente Filho University Hospital, Federal University of Rio de Janeiro. The parents of the students or responsible persons, together with the adolescents, signed a free informed consent form to be included in the study.
RESULTSEighteen adolescents were excluded from the study (8 due to the presence of dermographism and 10 because of a negative test result with the positive control), corresponding to a loss of 1.7 %, and the final sample consisted of 996 students (387 boys). The SPT was well tolerated by all adolescents.
On the basis of question 2 of the questionnaire regarding asthma (Have you had wheezing in the past 12months?), the students were randomly divided into two groups: asthmatics – students who responded positively to this question (n = 291) and non-asthmatics – students who responded negatively (n = 705). The same procedure was used to classify the students with positive responses regarding rhinitis (n = 338), no rhinitis (n = 658), asthma + rhinitis (n = 470), and no asthma and no rhinitis (n = 526).
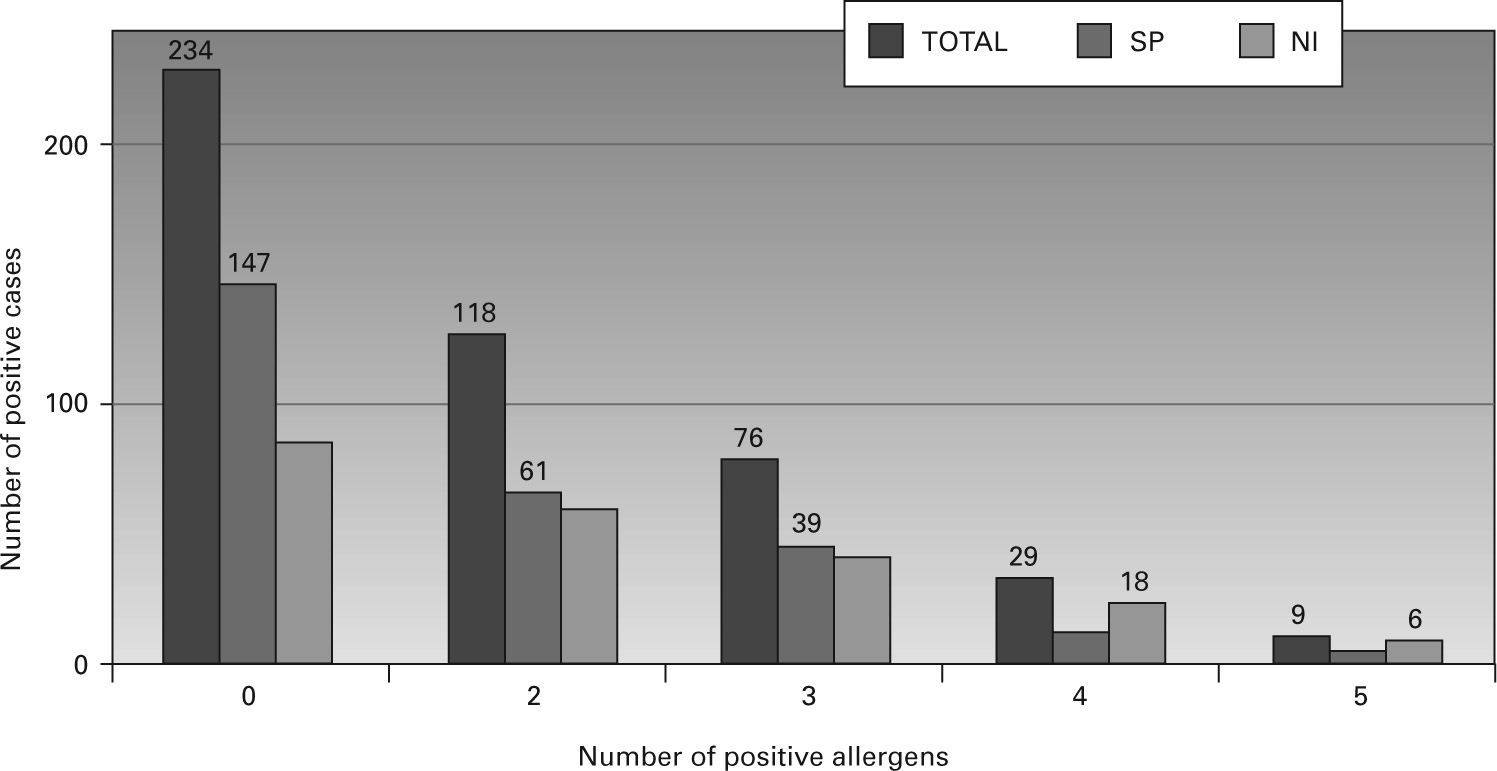
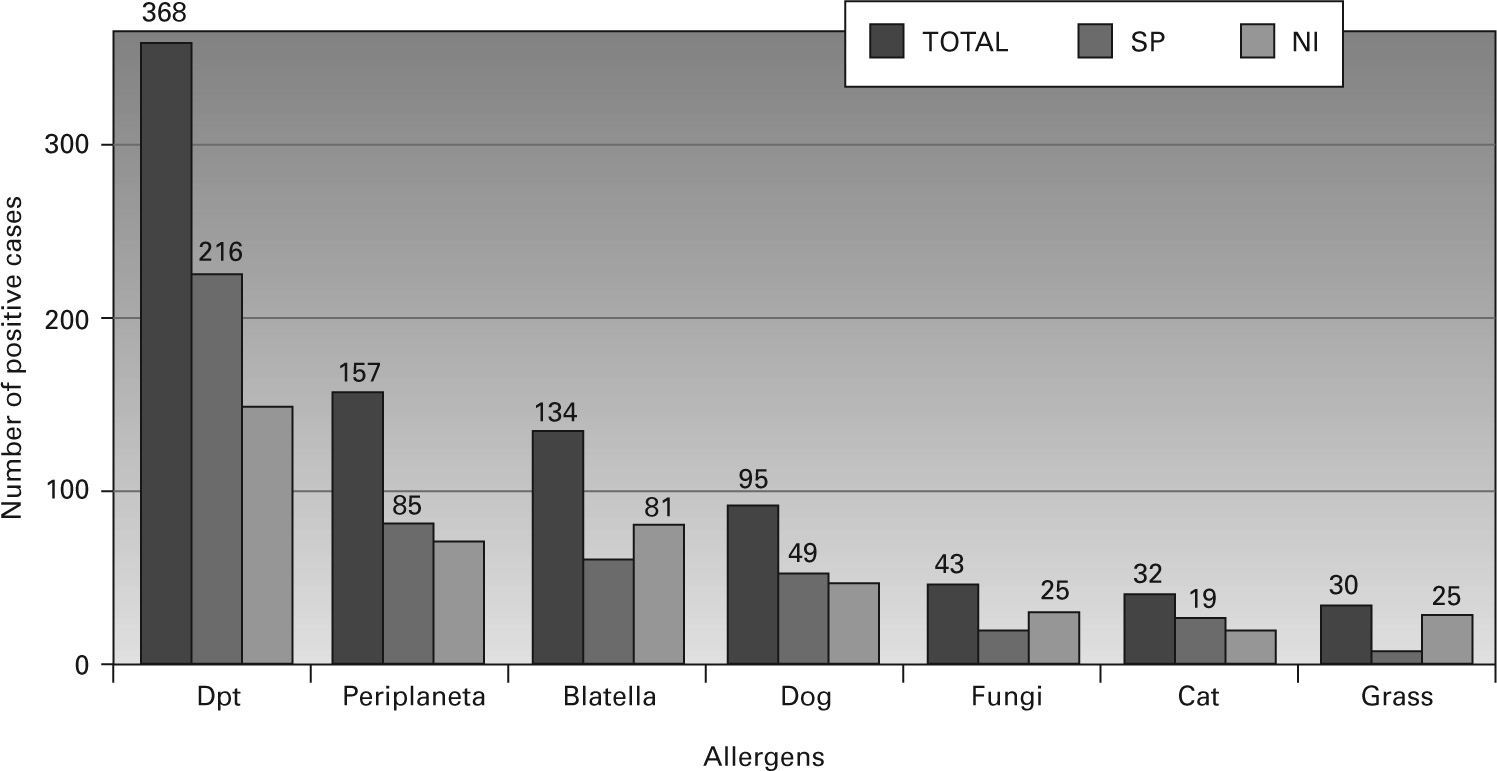
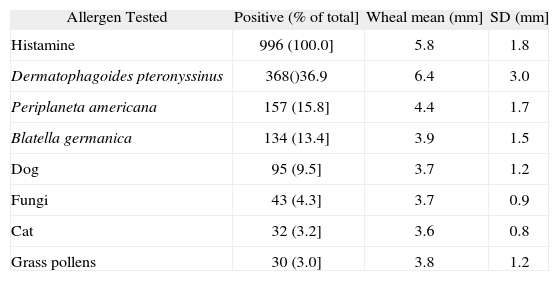
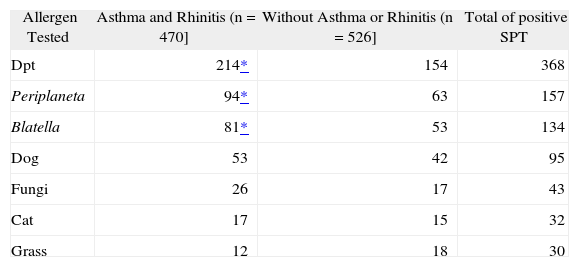
A positive reaction to at least one allergen was observed in 466 adolescents (46.8 %). The distribution of positive skin tests in each centre and for the total sample is shown in figure 1. No significant difference in gender was observed between students with a positive SPT to at least one allergen: 41.2 % boys (192/466) and 58.6 % girls (273/466) (OR = 1.21, 95 %CI = 0.94-1.56, p = 0.16). The distribution of SPT positivity to the different allergens tested is shown in figure 2, with 79.1 % of all positive tests showing sensitisation to Dpt, 33.7 % to Pa, and 28.8 % to Bg. The distribution of the mean wheal diameter and standard deviation obtained for the different allergens and histamine are shown in table I.
Positivity of Skin Prick Tests (SPT) in 996 adolescents – Wheal mean and standard deviation (SD)
| Allergen Tested | Positive (% of total] | Wheal mean (mm] | SD (mm] |
| Histamine | 996 (100.0] | 5.8 | 1.8 |
| Dermatophagoides pteronyssinus | 368()36.9 | 6.4 | 3.0 |
| Periplaneta americana | 157 (15.8] | 4.4 | 1.7 |
| Blatella germanica | 134 (13.4] | 3.9 | 1.5 |
| Dog | 95 (9.5] | 3.7 | 1.2 |
| Fungi | 43 (4.3] | 3.7 | 0.9 |
| Cat | 32 (3.2] | 3.6 | 0.8 |
| Grass pollens | 30 (3.0] | 3.8 | 1.2 |
Among the 466 patients with a positive SPT, 232 (49.8 %) reacted to more than one allergen (114 in Sao Paulo and 118 in Nova Iguacu), with the most frequent concomitant positivity being observed for
Dpt + Pa (40 cases) and Dpt + Pa + Bg (38 cases), followed by Dpt + Bg (24 cases) and Dpt + dog epithelium (20 cases).
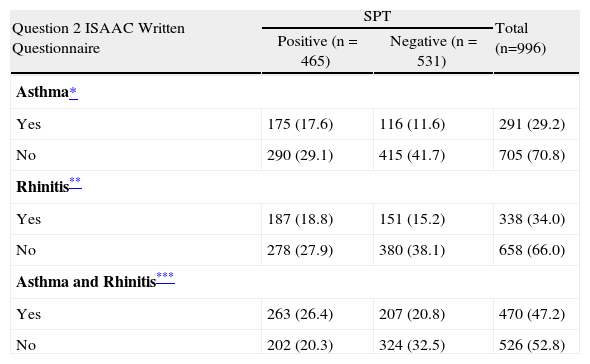
The frequency of positive SPTs was significantly higher among asthmatics (60.1 %) compared to nonasthmatics (41.1 %) (OR = 2.16, 95 %CI = 1.63-2.85, p < 0.0001). The same was observed for patients with rhinitis (53 %) compared to non-rhinitis subjects (42.4 %) (OR = 1.69, 95 %CI = 1.29-2.20, p < 0.0001) (table II). In addition, a higher prevalence of sensitisation was observed among students with asthma and rhinitis (56 %) compared to patients without asthma and without rhinitis (38.4 %) (OR = 2.03, 95 %CI = 1.58-2.62, p < 0.0001) (table II). An association between asthma and rhinitis was observed in Sao Paulo (OR = 4.25, 95 %CI = 2.83-6.4, p < 0.0001) and in Nova Iguacu (OR = 3.35, 95 %CI = 2.19-5.12, p < 0.0001).
Distribution Skin Prick Tests (SPT) positivity according to allergens tested and presence of asthma and/or rhinitis
The association between the presence of asthma and SPT positivity was significant for the following allergens tested: Dpt (OR = 1.98, 95 %CI = 1.34-2.9, p < 0.001), Pa (OR = 1.85, 95 %CI = 1.13-3.01, p = 0.013) and dog epithelium (OR = 2.04, 95 %CI = 1.12-3.74, p = 0.019) in Sao Paulo, and for Dpt (OR = 2.16, 95 %CI = 1.45-3.25, p < 0.0001), Bg (OR = 2.47, 95 %CI = 1.52-4.02, p < 0.0001) and Pa (OR = 1.84, 95 %CI = 1.11-3.06, p = 0.017) in Nova Iguacu. However, with respect to rhinitis, the association was only significant for Dpt both in Sao Paulo (OR = 1.76, 95 %CI = 1.24-2.5, p = 0.002) and in Nova Iguagu (OR = 1.65, 95 %CI = 1.08-2.49, p = 0.018).
Table III shows the association between positivity to each allergen tested and the presence of asthma and rhinitis, with emphasis on the following allergens: Dpt (OR = 2.02, 95 %CI = 1.55-2.62, p < 0.0001), Bg (OR = 1.86, 95 %CI = 1.29-2.69, p = 0.001), and Pa (OR = 1.84, 95 %CI = 1.3-2.6, p = 0.001). This relationship was similar for students from Sao Paulo and Nova Iguacu, except for a significant association with dog epithelium (OR = 2.6, 95 %CI = 1.38-4.9, p = 0.002) which was only observed for students from the western region of Sao Paulo.
Distribution of Skin Prick Tests (SPT) according to asthma, rhinitis or association asthma and rhinitis. Odds ratio (OR) values and 95 %CI
| Question 2 ISAAC Written Questionnaire | SPT | Total (n=996) | |
| Positive (n = 465) | Negative (n = 531) | ||
| Asthma* | |||
| Yes | 175 (17.6) | 116 (11.6) | 291 (29.2) |
| No | 290 (29.1) | 415 (41.7) | 705 (70.8) |
| Rhinitis** | |||
| Yes | 187 (18.8) | 151 (15.2) | 338 (34.0) |
| No | 278 (27.9) | 380 (38.1) | 658 (66.0) |
| Asthma and Rhinitis*** | |||
| Yes | 263 (26.4) | 207 (20.8) | 470 (47.2) |
| No | 202 (20.3) | 324 (32.5) | 526 (52.8) |
The positive (PPV) and negative predictive values (NPV) of the SPT for the presence of asthma were 60 % (95 %CI = 54 to 65 %) and 59 % (95 %CI = 55 to 62 %), respectively. Regarding the presence of rhinitis, the PPV and NPV were 55% (95 %CI = 49 to 60 %) and 57 % (95 %CI = 53 to 61 %), respectively. For the concomitant presence of asthma and rhinitis, the PPV and NPV were 56 % (95 %CI = 51 to 60 %) and 61 % (95 %CI = 57 to 65 %), respectively.
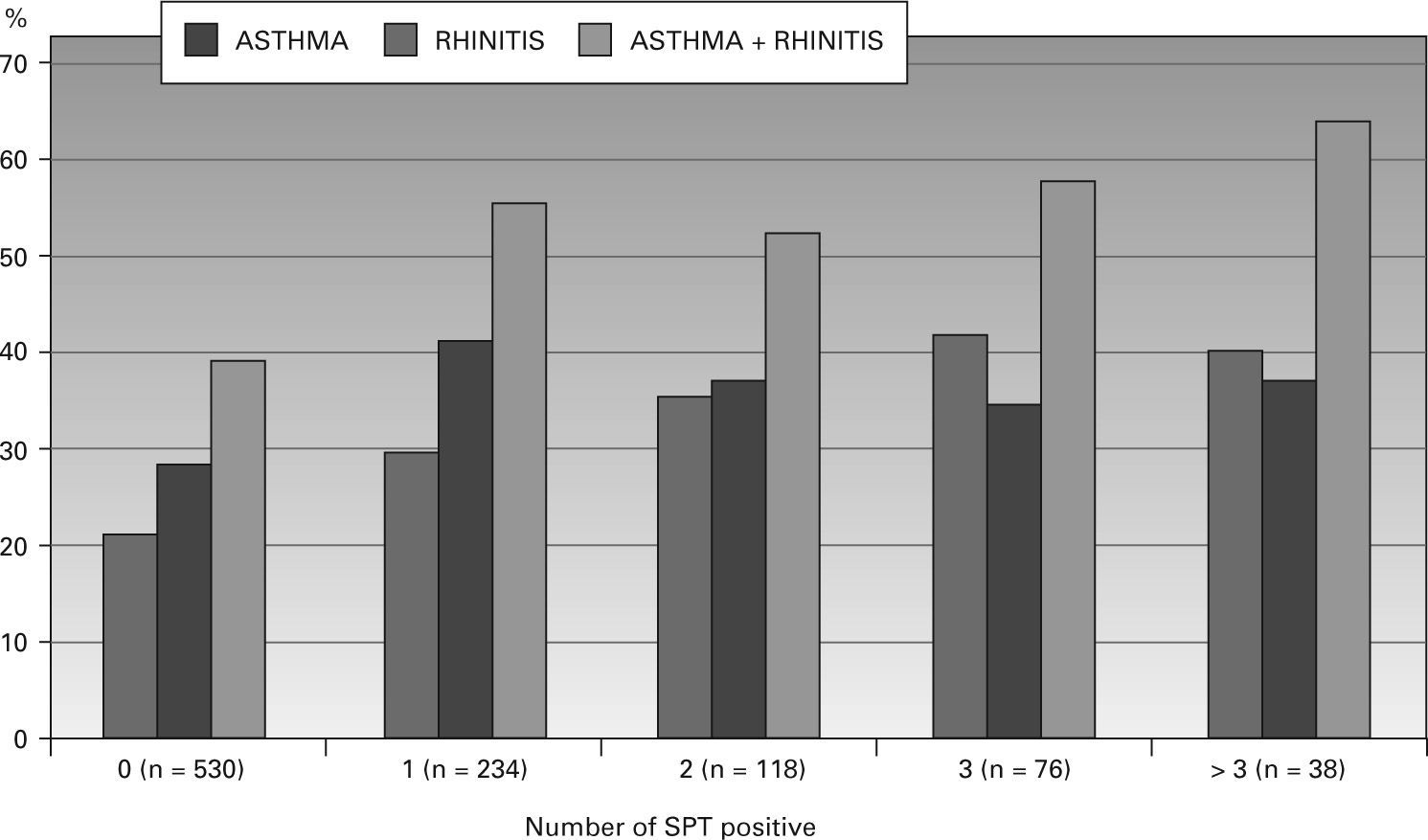
When comparing the number of positive SPTs and the presence of asthma or the combination of asthma and rhinitis, the finding of four or more positive tests (multiple sensitisation) demonstrated a risk 2.6 times higher (OR = 2.6, 95 %CI = 1.32-5.10, p = 0.0085) for having asthma (PPV = 42 %, NPV = 78 %) and a risk 3 times higher (OR = 3.0, 95 % CI = 1.5-5.9, p = 0.0018) for having both asthma and rhinitis (PPV = 66 %, NPV = 61 %). The number of positive SPTs did not increase the risk for rhinitis, as shown in figure 3.
Wheal size in relation to the presence of asthma was analysed individually for the main allergens found in our population (Dpt, Pa and Bg), with a mean wheal diameter of 6mm or more showing the best PPV and NPV. For Dpt, a wheal diameter of 6mm or more presented an OR of 2.37 for patients with asthma (PPV = 43 %, NPV = 76 %; p < 0.0001). The OR was 2.58 for the combination of asthma and rhinitis (PPV = 62 %, NPV = 61 %; p < 0.0001) and 2.2 for rhinitis alone (PPV = 46%, NPV = 71 %; p < 0.0001). With respect to cockroaches (Pa), a wheal diameter of 6mm or more showed an OR of 2.55 for the presence of asthma (PPV = 41 %, NPV = 78 %; p < 0.042), of 4.42 for the combination of asthma and rhinitis (PPV = 73 %, NPV = 61 %; p < 0.001), and no significance for rhinitis. For Bg, a wheal diameter of 6mm or more presented an OR of 5.25 for the presence of asthma (PPV = 60 %, NPV = 78 %; p < 0.0019) and of 4.29 for the combination of asthma and rhinitis (PPV = 73 %, NPV = 61 %; p < 0.0133), while no significance was observed for rhinitis.
DISCUSSIONThe prevalence of atopic diseases has been increasing in both developed and developing countries, and it is not possible to explain this increase only based on changes in the genetic characteristics of the population. The influence of exposure to environmental allergens on sensitisation and the induction of symptoms have been extensively studied. The process of sensitisation may or may not be associated with the onset of clinical symptoms, but several investigations have shown the risk of exposure to aeroallergens for both sensitisation and clinical manifestations of asthma and other atopies9–12. Longitudinal studies have demonstrated that this risk is directly related to early exposure and to the intensity of exposure to household allergens, especially house dust mites13,14.
In a meta-analysis, Peat & Li15 evaluated the effects of various environmental factors on the incidence and severity of asthma and concluded that exposure to household allergens is the main risk factor of asthma manifestations. More recently, cohort studies regarding early exposure to household allergens, sensitisation and the occurrence of increased bronchial responsiveness and asthma have reported conflicting results16. Especially concerning the exposure to cat allergens, various investigations have demonstrated that indoor exposure to elevated levels of Fel d 1 might induce the production of specific IgG and IgG4 in the absence of sensitisation or a risk for asthma17,18. Environmental control measures used as primary prophylaxis and analysed throughout childhood proved to be ineffective, but the reduction in allergen exposure continues to be important in secondary prevention19.
Most studies report domestic exposure to aeroallergens as determinant for sensitisation and the occurrence of symptoms; however, little emphasis is placed on exposure to the same allergens at schools and day-care centres19,20. A recent study document-ed the exposure of nursing infants, preschool children and schoolchildren to elevated levels of cockroach allergens at day-care centres and schools in the city of Sao Paulo1. This fact might explain the high degree of sensitisation to these allergens reported in previous studies involving children of the same socioeconomic level21. The adolescents studied here were from underprivileged socioeconomic classes, living in shanty towns or precarious dwellings which often surrounded the schools. The typically rural environment of the schools in Nova Iguacu might explain the differences in the sensitisation to grass pollen and fungi in these students when compared to those from the western region of the municipality of Sao Paulo.
The SPT has been used in the identification of possible atopy-causing allergens for more than six decades. The use of a standard technique by trained personnel, and especially employing standardized material in terms of the composition of the allergens tested and the lancets used, has caused this method to be safe, rapid, low-cost and a method of choice for establishing the allergic basis of patient symptoms. The selection of allergens to be tested in different populations or even individually should take into account the prevalence of allergens to which the population is exposed22,23.
The criterion of atopy adopted in the present study was a positive reaction to at least one of the allergens tested, a criterion used in different cohort and case–control studies; however, one should remember that the results need to be interpreted within the context of the history and symptoms of each patient. Population studies have identified asymptomatic individuals with a positive SPT, with some reports showing a relationship between positivity and the future onset of rhinitis or asthma symptoms in 20 to 60 % of skin sensitisation patients during variable follow-up periods of 2 to 20 years24.
Reports of positive SPTs in asymptomatic patients are rare in the Brazilian and international literature, but have been described in up to 30 % of individuals without a history of any type of allergy when tested against a set of aeroallergens to which the particular population is exposed24,25. A population study conducted on 3271 schoolchildren (13 to 14years old) in the city of Curitiba, Brazil, in 1999, which determined the frequency of sensitisation to Dpt in the general population, detected 31.3 % of positive SPTs to this mite25. In the present study, we observed an elevated degree of sensitisation (positive SPT to at least one allergen) in 41.1 % of adolescents without symptoms of asthma, in 42.4 % without symptoms of rhinitis, and in 38.4 % without symptoms of asthma and rhinitis. These results permit us to infer that low socioeconomic and environmental conditions may facilitate sensitisation in these populations which, although asymptomatic, may in the future present allergic symptoms and therefore require periodic follow-up. Another noteworthy aspect is the development and implementation of secondary prevention programmes in order to reduce exposure to these aeroallergens in an attempt to minimize progression to symptomatic disease.
In Brazil, the main inhalant allergens are represented by mite species (Dpt, Dermatophagoides farinae and Blomia tropicalis [Bt]) present in house dust. Our results clearly show a higher frequency of sensitisation to Dpt in adolescents reporting symptoms of asthma, rhinitis or both, as well as in asymptomatic cases. The finding of 41.8 % of positive skin tests to Dpt in students without symptoms of asthma and rhinitis is higher than that reported in 1999 for the general population of the same age in the city of Curitiba. The Curitiba schoolchildren attended public and private schools concentrated in the central region of the city, located in the southern region of our country, in contrast to the students evaluated here which belonged to an underprivileged socioeconomic class and lived in more peripheral areas of the cities of Sao Paulo and Nova Iguacu, a fact that might explain the higher frequency of sensitisation.
With respect to cockroach allergens, 15.8 and 13.4 % of all SPTs were positive for Pa and Bg, respectively. Since the adolescents studied here were of a low socioeconomic condition and lived in very poor dwellings, a higher prevalence of sensitisation to cockroaches in general was expected, as also reported by some investigators for asthmatic children26–28. Analysis of students with and without asthma showed a significantly higher positivity to Pa and Bg in asthmatic patients (22 and 19.9 %, respectively). The same was observed for patients with asthma and rhinitis (20 and 17.2 % for Pa and Bg, respectively), while the difference was not significant for adolescents with rhinitis only. Our findings are in contrast to those reported in other Brazilian studies which demonstrated positivity to cockroach allergens reaching values of up to 55 %, and are similar to the lower rates reported in American studies involving asthmatics of low income (23 to 60 % rate of cockroach sensitisation)28–30. Although we observed a discrete predominance of sensitisation to Pa antigens, the rate did not differ from that reported in other studies and further investigations analysing the two species separately would be important even though there is a 40 to 50 % correlation between their allergens31,32.
The PPV and NPV of a positive SPT in relation to the data of the ISAAC questionnaire obtained in the present study indicate that the test detects only up to 65 % of cases with positive responses regarding asthma, rhinitis or both. These low values might be explained by the high sensitisation of the populations studied or by an eventual failure to fill out the self-administered questionnaires in the ISAAC study. It should be emphasized that a positive response to the question regarding wheezing in the past 12months (active asthma) used in the ISAAC protocol shows a high sensitivity and specificity as confirmed by construct validation when compared to bronchial reactivity evaluated by methacholine provocation in a Brazilian study33.
The increase in the prevalence of asthma does not seem to be related only to the degree of sensitisation to the most common household allergens (mites and cockroaches), since an increase in the prevalence of asthma has also been reported for countries were the levels of these allergens are negligible. The hygiene hypothesis for underprivileged populations such as those studied here also does not explain the high percentages of patients with asthma symptoms (21.9 % in Sao Paulo and 11.8 % in Nova Iguacu), which are close to those of countries considered to have a high prevalence of asthma in the ISAAC study. In the present series, sensitisation to multiple allergens was associated with a higher and increasing risk for asthma and the combination of asthma and rhinitis, in agreement with Arshad et al34, but with lower percentages for asthma than for asthma and rhinitis and no significance for rhinitis alone. Asrhad et al34 also documented sensitisation to pollen in 31.7 % of their patients studied. These allergens are not the most common in the Brazilian regions included in this study, a fact that might explain the lower relationship with rhinitis. Other investigators also reported a number of positive SPTs higher than 3 to be a risk for the presence of asthma35,36. The same association was observed for wheals measuring 6mm or more. We emphasize the higher risk for asthma and the combination of asthma and rhinitis detected in the present adolescents when analyzing sensitisation to cockroach allergens. On the other hand, the number of positive tests or mean wheal diameter did not increase the chance for a diagnosis of rhinitis.
Recently, attempts have been made to explain the development or not of asthma in genetically predisposed populations based on the combination of several factors, such as sensitisation to allergens, presence of endotoxins in the environment, particulate pollutants, lower rates of infections, as well as a reduction in physical activity, changes in dietary habits and development of obesity. Irritating factors or even factors triggering symptoms of asthma such as viral infections, active or passive smoking, environmental allergens, physical exercise and cold air are also part of the mechanisms involved in the changes necessary for the development of airway inflammation37.
Even considering all aspects of the role of primary prevention in the development of allergies, the importance of obtaining information regarding possible risk factors for allergic diseases lies in its utilization in public health interventions. Guidance regarding more adequate environments, especially for children with a genetic predisposition and for those already sensitized, has proved to be useful in the secondary prevention of allergic diseases38.
We thank: Renata Tambelini, Andréia R. Penha, Fabiana Hashimoto, Kelly A Furuta (Sao Paulo), Mara M.R. Félix, Ana Lúcia P.M. Rego, Adriana M. Raymundo, Gabriela C.T.P. Sepúlveda (Nova Iguacu, Rio de Janeiro) for their help in performing the skin prick tests.