A relationship between asthma and obesity has been documented in children and adolescents. An alternate day calorie restriction diet has been reported to improve asthma symptoms by decreasing levels of serum cholesterol and triglycerides, reducing markers of oxidative stress and increasing levels of the antioxidant uric acid. Therefore, to investigate the lipid profile in asthmatic children may be important in asthma control treatment.
Materials and methodsOne hundred and sixty newly diagnosed persistent asthmatic children were selected to participate in the study. They were divided into four groups based on their body mass index (BMI): Group I normal weight (BMI=20–24.9kg/m2, n=30); Group II under-weight (BMI<20kg/m2, n=30); Group III overweight (BMI=25–30kg/m2, n=25); and Group IV obese (BMI>30kg/m2, n=25). Fasting blood sugar, fasting insulin, and HbA1c were measured to exclude the possibility of pre-diabetes. Lipid profile measurements included total cholesterol, high-density lipoprotein (HDL), low-density lipoprotein (LDL), apo-A1, apo-B and triglycerides.
ResultsThere were no significant differences in the levels of apo-A1, apo-B, triglycerides, cholesterol and LDL in all four groups. Only the level of HDL was higher in GIV>GIII>GII>GI (75.84±13.95, 68.56±15.28, 64.17±13.93, 63.17±14.34mg/dl, respectively). There were no cases of pre-diabetes in any of the four groups.
ConclusionHypercholesterolaemia and hypertriglyceridaemia were not found in any of the persistent asthmatic children, and thus they are not high risk factors for asthma. Similarly, there were no differences in apo-A1 and apo-B between any of the BMI groups. No differences were found in LDL levels, however HDL levels were increased in all four groups, indicating that allergic sensitisation may have occurred. Controlling body weight and restricting calorie intake may be as important as appropriate pharmacological management in controlling asthma.
The global prevalence rates of current asthma in children aged 6–7 years and 13–14 years have been reported to be 11.7% and 14.1%, respectively.1 Increasing evidence suggests that obesity is a risk factor for asthma, and that weight loss can improve symptoms. Improved clinical findings have also been associated with decreased levels of serum cholesterol and triglycerides, striking reductions in markers of oxidative stress and increased levels of the antioxidant uric acid. The pro-inflammatory role of serum cholesterol in asthma has been studied with contradicting results. A modest but significant association between higher levels of serum cholesterol and asthma, independent of age, gender, body mass index (BMI), socio-economic status and serum high sensitivity C reactive protein has been reported.2 Moreover, hypercholesterolaemia and obesity have been reported to independently increase the risk of asthma.3 Compliance with an alternative day calorie restriction diet has been reported to be associated with improvements in symptoms and pulmonary function, and reductions in oxidative stress and inflammation.4 In addition, Buchowski showed that oxidative stress can be rapidly reduced and the reduction sustained through a modest reduction in caloric intake, suggesting potential health benefits for overweight and obese women.5 However, Ouyang reported that although adiposity is associated with asthma, a higher percentage of body fat, and lower high-density lipoprotein (HDL) and higher low-density lipoprotein (LDL) levels were associated with a greater risk of allergic sensitisation mostly in lean Chinese subjects.6 Thus, a genetic influence on these traits may exist. Ahmad reported that gender and ethnicity were significantly associated with asthma, and that obesity was positively associated with asthma in children aged 13–17 years.7 In addition, Fessler reported that cholesterol promotes Th2 immunity and allergic inflammation in rodents. Reports of both direct and inverse associations between serum cholesterol and atopy in different populations suggest that ethnicity or other demographic variables may modify these relationships.8 Asthma and obesity are associated disorders, however the mechanisms responsible for this relationship are unclear. The aim of this study was to examine the lipid profiles of mild to moderate asthmatic children and investigate the association between dyslipidaemia and asthma and the effect of asthma and obesity on hyperlipidaemia.
Material and methodsRenai and Mother & Child branches of Taipei City Hospital participated in this study, and the research protocol was approved by the Institutional Review Board of each branch. From January 1, 2013 to October 23, 2014, 160 persistent asthmatic patients (asthma symptoms ≥3 days per week or ≥3 nights per week) aged 6–17 years with asthma diagnosed by a doctor were asked to participate in this study. We excluded patients who had used systemic corticosteroids two weeks before the study. The participants were divided into four groups based on BMI: Group I normal weight (BMI=20–25kg/m2, n=30); Group II under-weight (BMI<20kg/m2, n=30); Group III overweight (BMI=25–30kg/m2, n=25); and Group IV obese (BMI>30kg/m2, n=25). Fasting blood sugar, fasting insulin, and HbA1c were measured to exclude the possibility of pre-diabetes. Lipid profiles including total cholesterol, HDL, LDL, apo-A1, apo-B and triglycerides were measured before breakfast. All parents/guardians of participants gave informed consent (as the legal age of consent in Taiwan is 20). SPSS software (version 1.2 for Windows; SPSS Inc., Chicago, IL, USA) was used for all analyses. A p-value of less than 0.05 was considered to be statistically significant.
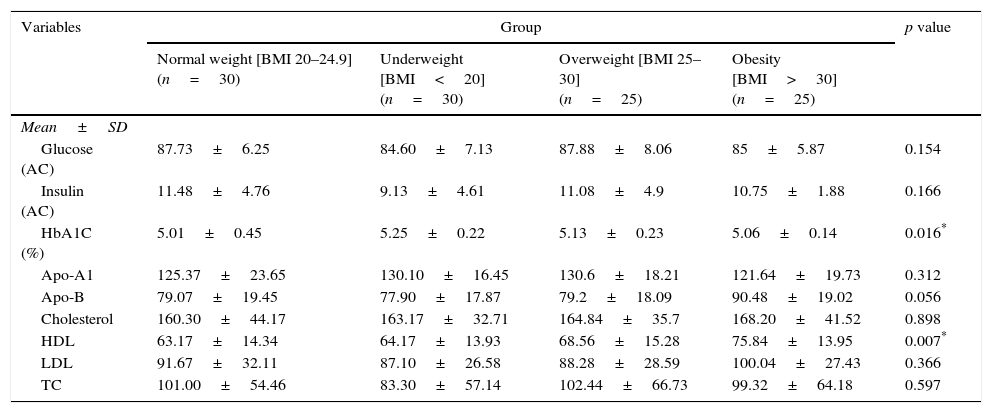
ResultsThe lipid profiles of the four groups showed that the level of HDL increased in the following order: obesity>overweight>underweight>normal weight (75.84±13.95, 68.56±15.28, 64.17±13.93, and 63.17±14.3mg/dl; respectively, p=0.007). There were no significant differences in cholesterol, triglyceride and LDL levels in all four groups (p>0.05). Levels of fasting blood sugar and fasting insulin were within normal limits in all of the four groups. There were no cases of pre-diabetes in any of the four groups (Table 1).
Lipid profiles in school children with persistent asthma (ANOVA).
| Variables | Group | p value | |||
|---|---|---|---|---|---|
| Normal weight [BMI 20–24.9] (n=30) | Underweight [BMI<20] (n=30) | Overweight [BMI 25–30] (n=25) | Obesity [BMI>30] (n=25) | ||
| Mean±SD | |||||
| Glucose (AC) | 87.73±6.25 | 84.60±7.13 | 87.88±8.06 | 85±5.87 | 0.154 |
| Insulin (AC) | 11.48±4.76 | 9.13±4.61 | 11.08±4.9 | 10.75±1.88 | 0.166 |
| HbA1C (%) | 5.01±0.45 | 5.25±0.22 | 5.13±0.23 | 5.06±0.14 | 0.016* |
| Apo-A1 | 125.37±23.65 | 130.10±16.45 | 130.6±18.21 | 121.64±19.73 | 0.312 |
| Apo-B | 79.07±19.45 | 77.90±17.87 | 79.2±18.09 | 90.48±19.02 | 0.056 |
| Cholesterol | 160.30±44.17 | 163.17±32.71 | 164.84±35.7 | 168.20±41.52 | 0.898 |
| HDL | 63.17±14.34 | 64.17±13.93 | 68.56±15.28 | 75.84±13.95 | 0.007* |
| LDL | 91.67±32.11 | 87.10±26.58 | 88.28±28.59 | 100.04±27.43 | 0.366 |
| TC | 101.00±54.46 | 83.30±57.14 | 102.44±66.73 | 99.32±64.18 | 0.597 |
Apo-A1, apolipoprotein A1; Apo B, apolipoprotein B; HDL, high density lipoprotein cholesterol; LDL, low density lipoprotein cholesterol; TC, triglyceride.
The association between hypercholesterolaemia and obesity with airway hyperresponsiveness has drawn increasing attention due to the potential role of cholesterol and lipid homeostasis in lung physiology and asthma.9 However, the mechanism responsible for this obesity-asthma association is unknown. A high-fat meal can lead to significant increases in nitric oxide (FeNO), total cholesterol, and especially triglycerides. This suggests that a high-fat diet may contribute to chronic inflammatory diseases of the airway and lungs.10 The disease burden of asthma appeared normal in normal weight and slightly overweight women rather than obese and markedly obese women suggests that the development of asthma may be a point on the trajectory of chronic obesity or that asthma and obesity are concurrent disorders.11 Asthma and obesity are associated disorders, however obesity in patients with difficult-to-treat asthma has been reported to be inversely related with sputum eosinophils and exhaled FeNO, and positively associated with the presence of co-morbid factors and reduced lung volume. In addition, a higher BMI has been reported to be associated with elevated FeNO. This suggests that factors other than airway inflammation alone may explain the relationship between obesity and severity of asthma.12,13 In addition, obese adolescent males with mild persistent asthma have been reported to have a significantly higher prevalence of metabolic syndrome than obese males without asthma.14 Thus, when studying the lipid profile of asthmatic patients, those with pre-diabetes should be excluded. Studies exploring the effect on obesity of eating fast food and watching television have reported that frequent and very frequent consumption of fast food was associated with a higher BMI in children,15,16 and that a higher number of hours of watching television was positively associated with BMI in both adolescents and children with an apparent dose response effect.17 Therefore, it seems that all risk factors for obesity are related to asthma and even asthma exacerbation.
Although cholesterol exerts complex effects on inflammation, the relationship between cholesterol and asthma/wheezing has been reported to be independent of BMI and C reactive protein and similar between atopic and non-atopic participants.18 Plasma secretory A2 (sPLA2) has been shown to have functions relevant to asthmatic inflammation, including eicosanoid synthesis and effects on dendritic cells and T cells, and also to provide a biological link between asthma, inflammation, increased BMI, lipid metabolism and antioxidants. Interactions among these factors may be pertinent to the pathophysiology and increasing prevalence of both asthma and obesity.19 El-Shaboury reported a significant increase in the incidence of endogenous hypertriglyceridaemia but not of hypercholesterolaemia in asthmatic patients.20 Another study established a critical role of ATP-binding cassette transporter A1 in reverse cholesterol and phospholipids transport in airway smooth muscle cells, suggesting that dysregulation of cholesterol homeostasis in these cells may be important in the pathogenesis of asthma.9
It has recently been shown that diet-induced dyslipidaemia alters trafficking of immune cells to the lung in a manner that may have important implications for the pathogenesis of acute lung injury, asthma, and pneumonia. Conversely, cholesterol-targeting pharmacological agents such as statins, apolipoprotein mimetic peptides, and liver X receptor agonists have shown early promise in the treatment of several lung disorders including asthma.21 Apolipoprotein A1 (apo-A1) is a key component of HDL that mediates reverse cholesterol transport from cells and reduces vascular inflammation. In an animal model, endogenous apo-A1 was found to negatively regulate OVA-induced neutrophilic airway inflammation, primarily via a G-CSF-dependent mechanism. This suggests that apo-A1 may play an important role in modulating the severity of neutrophilic airway inflammation in asthma.22 Apo-A1 mimetic peptides have been shown to attenuate airway inflammation, airway remodelling, and airway hyperreactivity in murine models of experimental asthma. Thus, site-directed delivery of apo-A1 mimetic peptides may represent a novel treatment approach for asthma.23–25 Cholesterol-lowering drugs (or statins) possess pleiotropic immunomodulatory properties, and this has opened a new area of research regarding the anti-inflammatory and anti-proliferative properties of statins. Thus, statins may modulate mevalonate-dependent and independent pathways, and the emerging area of cholesterol, sphingolipid, and lipid raft biology in lung diseases may lead to new therapeutic targets.26
The mean plasma lipid level after long-term slow-release theophylline treatment has been reported to be significantly higher than that before treatment.27 However, Allayee showed that serum levels of all lipids were significantly lower in patients taking montelukast and theophylline compared to a placebo, and thus asthma medication may have some beneficial effects for asthmatics with respect to the risk of cardiovascular disease.28 No significant changes in serum fasting triglyceride concentrations have been reported before and after inhaled corticosteroid therapy, and only high-dose inhaled corticosteroids have been reported to have a minor effect on lipid metabolism after long periods of use in asthmatic patients.29 Moreover, beta 2-adrenergic stimulation has been reported to have no effect on basal serum lipid levels.30
In the current study, the HDL concentration was obviously increased in the obese and overweight children and even in the normal weight and underweight group, however the cholesterol and triglyceride levels were within normal limits in all of the four study groups. This means that persistent asthma and even asthma exacerbations occurred independently of the lipid profit of the participants. Hypercholesterolaemia is a risk factor for asthma, independent of obesity, and serum total cholesterol and non-HDL have been reported to be inversely related to asthma.18 This is in contrast to Chen's study, in which asthma was associated with high LDL levels and this association was amplified in overweight and obese subjects.31 Moreover, our results are different from other studies which showed that high serum triglyceride and low serum HDL levels were associated with wheezing after adjusting for adiposity.32,33
In conclusion, understanding the relationship between lipid profiles and asthma does not completely clarify why the prevalence of asthma is higher in obese children. However, body weight control with a restricted calorie intake may become a therapeutic treatment for children with asthma.
Ethical disclosuresProtection of human subjects and animals in researchThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence is in possession of this document.
Conflicts of interestAll authors declare that there are no conflicts of interest that may be inherent in this submission.