Parastomal variceal bleeding (PVB) is a serious complication occurring in up to 27% of patients with an ostomy and concurrent cirrhosis and portal hypertension. The management of PVB is difficult and there are no clear guidelines on this matter. Transjugular intrahepatic portosystemic shunt (TIPS), sclerotherapy, and /or coil embolization are all therapies that have been shown to successfully manage PVB. We present a case series with five different patients who had a PVB at our institution. The aim of this case series is to report our experience on the management of this infrequently reported but serious condition. We also conducted a systemic literature review focusing on the treatment modalities of 163 patients with parastomal variceal bleeds. In our series, patient 1 had embolization and sclerotherapy without control of bleed and expired on the day of intervention due to hemorrhagic shock. Patient 2 had TIPS in conjunction with embolization and sclerotherapy and had no instance of rebleed 441 days after therapy. Patient 3 did not undergo any intervention due to high risk for morbidity and mortality, the bleed self-resolved and there was no further rebleed, this same patient died of sepsis 73 days later. Patient 4 had embolization and sclerotherapy and had no instance of rebleed 290 days after therapy. Patient 5 had TIPS procedure and was discharged five days post procedure without rebleed, patient has since been lost to follow-up.
Parastomal variceal bleeding (PVB) is a phenomenon first described in the literature in 1968 by Resnick, et al. as a late complication in cirrhotic patients who had not received a shunt between their portal and systemic vascular systems.1 It is well established that patients with portal hypertension are at an increased risk for esophageal, gastric, duodenal, and rectal varices and management for these is well described in the literature. The cause of varices is due to engorgement in the venous vasculature at a location where a low systemic pressure system and high portal pressure collide. Parastomal varices are more unique, in that, they are the result of a surgical creation in the form of a stoma, such as an end colostomy, diverting loop ileostomy, or end ileostomy. Although the most common cause of PVB is portal hypertension, as a result of cirrhosis, other potential etiologies for PVB include mesenteric venous thrombosis causing isolated pressure near the stoma.2 Saad, et al. classified varices and found that most PVBs are either type-1a or type-2a. Type-1a is a nonocclusive varix with porto-portal collaterals only, whereas type-2a is non-occlusive but has porto-portal collaterals and trace porto-systemic collaterals.3 It is estimated that PVB occurs in up to five percent of patients with a stoma but as high as fifty percent in patients with portal hypertension. Parastomal varices are usually first documented two years after ostomy placement but have been reported to appear as early as five months.4 The recognition and treatment of PVB has not been well established leading to the exploration of new treatment modalities.5
Material and MethodsThis case series was conducted by performing a retrospective study, approved by the Institutional Review Board, of patients between the years of 2013 and 2016 diagnosed with a PVB. The proper written informed consent was obtained for clinical management of patients including those who received TIPS placement, prior to procedures. The risks and benefits of TIPS as well as the limited data on utilizing TIPS for this particular presentation was discussed. Once patients were identified, we collected multiple variables including: patient demographics, model for end stage liver disease (MELD) scores, hematocrit (Hct), hemoglobin (Hb) and platelet (plt) count - prior to admission, at admission, before any PVB intervention, and after any PVB intervention. We also investigated INR level, indication for stoma, type of stoma, etiology of cirrhosis, mortality and bleeding free survival. Bleeding free survival was defined as the interval number of days between the first PVB intervention at our institution and last observation in the electronic medical record at our institution without a PVB.
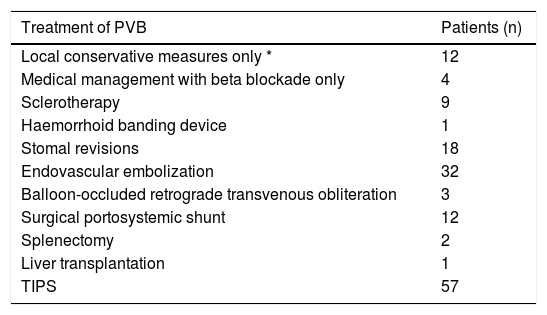
Literature reviewIn December of 2017 the US National Library of Medicine / National Institute of Health database was searched for relevant articles from MEDLINE, life science journals and online books (www.pubmed.gov). The following terms alone or in their combinations “bleed”, “bleeding”, “stoma”, “stomal”, “varices”, “portal hypertension” were used to generate search results. The review was performed by a single researcher. The search terms generated a total of 81 articles. 27 articles were excluded after title and/or abstract review. Exclusion criteria included abstracts and/or manuscripts not in the English language, titles without abstracts, stomal bleeds secondary to urologic procedures and portal hypertension secondary to biliary atresia. 54 articles encompassing 163 patients were included in our literature review.22-63Table 1 describes the reported treatment modalities of parastomal variceal bleed found in this search.
Reported treatment modalities of parastomal variceal bleed.
| Treatment of PVB | Patients (n) |
|---|---|
| Local conservative measures only * | 12 |
| Medical management with beta blockade only | 4 |
| Sclerotherapy | 9 |
| Haemorrhoid banding device | 1 |
| Stomal revisions | 18 |
| Endovascular embolization | 32 |
| Balloon-occluded retrograde transvenous obliteration | 3 |
| Surgical portosystemic shunt | 12 |
| Splenectomy | 2 |
| Liver transplantation | 1 |
| TIPS | 57 |
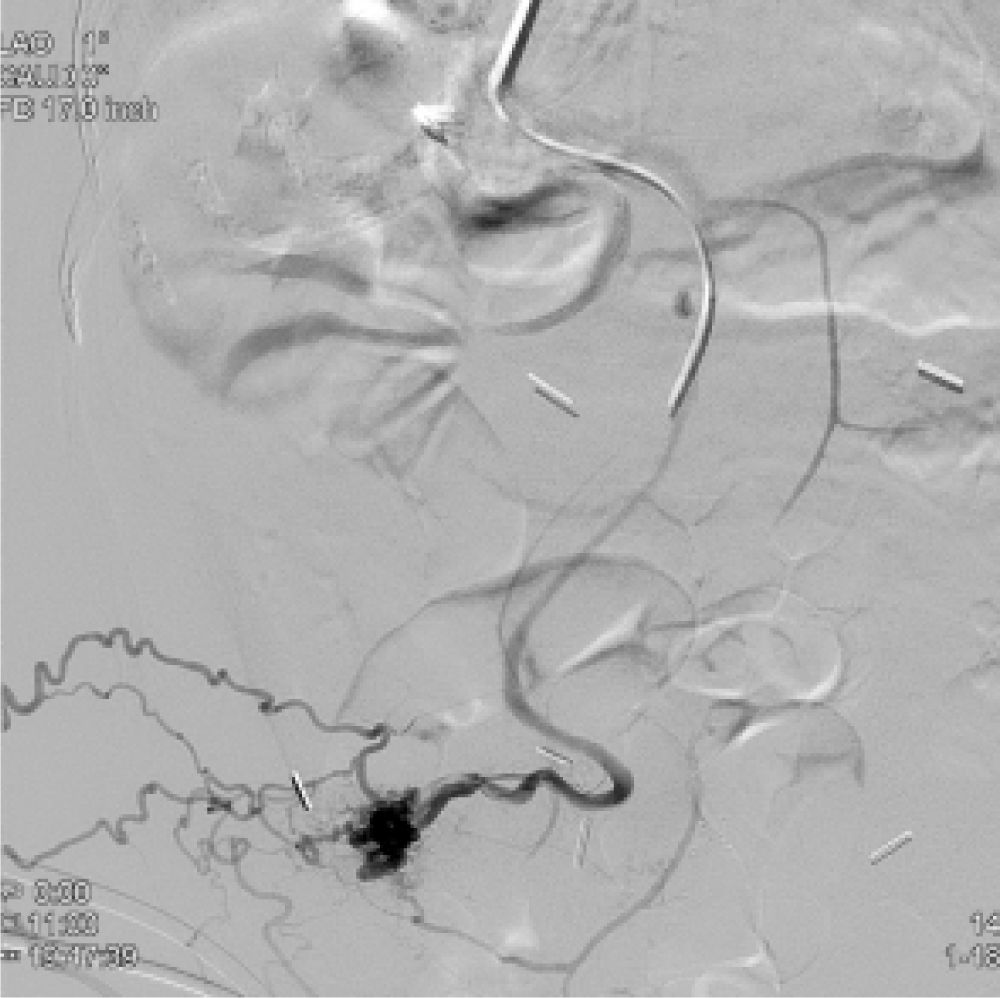
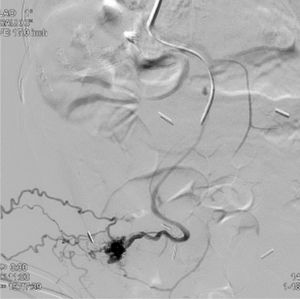
A 63-year-old white female with a past medical history (PMH) of fulminant clostridium difficile colitis status post total colectomy with end ileostomy and cryptogenic decompensated cirrhosis complicated by stomal varices and hepatic encephalopathy presented to the hospital with a chief complaint of stomal bleeding. The patient had her ostomy placed in 2008 with the first reported PVB two years later, followed by two subsequent bleeds eight and nine years after original ostomy placement. All of these aforementioned PVBs were managed conservatively with packed red blood cell (pRBC) transfusions. Upon presentation to our center the patient was initially hemodynamically stable, however she developed stomal rebleeding overnight resulting in hypotension with systolic blood pressures in the 60s. Patient was resuscitated and interventional radiology (IR) was consulted for TIPS. The portosystemic gradient pressure was found to be 8-9 mmHg and TIPS procedure was deferred. Thereafter, the patient underwent gelfoam and sclerosant embolization of a large peristomal variceal nidus from a branch of the superior mesenteric vein (Figure 1 and Figure 2). She again decompensated, this time during the procedure with hypotension and continued stomal bleed requiring the initiation of vasopressors and multiple packed red blood cell (pRBC) transfusions. Gastrointestinal (GI) surgery was consulted for bedside management and attempts were made to achieve hemostasis with ostomy packing and suture placement. Emergent ileoscopy was planned but the patient continued to decompensate and quickly expired. No attempts at resuscitation were made as the patient’s code status was do not resuscitate. Within hours of these interventions, patient expired with the cause of death being hemorrhagic shock.
A 40-year-old white female with a PMH of ulcerative colitis (UC) on adalimumab status post total colectomy and end ileostomy with decompensated cirrhosis secondary to primary sclerosing cholangitis (PSC) complicated by esophageal and stomal varices presented to the hospital for TIPS evaluation. Patient had an ostomy placed in 2013 and had first reported stomal bleed two years after placement. Two months prior to admission at our center the patient had first reported stomal bleed which required a total of 14 units of pRBC transfusions at an outside hospital. The patient additionally had stomal variceal stitching without success. Upon arrival to the hospital she had continued brisk bleeding from her stomal site leading to a decrease in hematocrit by 50 percent within 6 h. The following day she underwent TIPS procedure with sclerosant embolization of enlarged femoral varices with an enlarged stomal nidus. Mean portosystemic gradient was reduced from 17 to 5 mmHg. The patient remained hemodynamically stable, required no further transfusion, and was discharged two days post TIPS. She reported to follow up one month after discharge and denied any further bleeding but expressed worsening jaundice and encephalopathy. Labs at that time displayed a hematocrit of 30. She later underwent successful orthotopic liver transplantation nine months after the aforementioned admission. Post-operative course was complicated by a biliary stricture requiring endoscopic retrograde cholangiopancreatography but the patient had no further stomal bleeding events.
Patient 3A 73-year-old white female with a PMH of Crohn’s disease status post diversion with loop colostomy complicated by high ostomy output, chronic kidney disease (CKD) stage IV presented to the hospital with a chief complaint of encephalopathy. Patient had her ostomy placed in January of 2015. She was found to have an acute kidney injury on CKD and urosepsis. Shortly after admission the patient progressed to end stage renal disease (ESRD) requiring permcath placement for initiation of intermittent hemodialysis. Following permcath placement the patient was noted to have blood oozing from her ostomy site GI surgery was consulted for stomal evaluation - on exam there was no evidence of bleeding and thus no intervention. Subsequent computed tomography (CT) abdominal imagining displayed cirrhotic configuration of the liver which raised concerns for parastomal varices. The pathogenesis of cirrhosis was determined to be secondary to hepatitis C virus (HCV). Her bleed initially resolved but overnight there was an additional bleed from her ostomy site. Further history from her family revealed multiple episodes of PVB over the past 90 days which put her first reported bleed to be eight months after original ostomy placement. CT angiogram displayed abdominal wall varices coursing from the superior mesenteric artery through the peristomal region. Patient was evaluated by IR for possible intervention with TIPS and/or embolization. IR decided against either as there was no appreciable target for embolization and a high morbidity and mortality for TIPS procedure secondary to elevated pulmonary artery pressure and ESRD. During the hospitalization patient had no further bleeding events, hematocrit remained stable and no further transfusions were required. The patient received two separate paracentesis due to worsening ascites and completed treatment for her urinary tract infection. She was discharged without incident. After discharge the patient had several subsequent admissions for sepsis. Four months following her initial parastomal bleed at hospital patient was put on hospice and expired two days later.
Patient 4A 73-year-old white male with PMH of UC status post colectomy with end-ileostomy and nonalcoholic steato-hepatitis (NASH) cirrhosis complicated by esophageal variceal bleed presented from an outside hospital (OSH) for the management of a bleed from his ostomy site. Patient had his ostomy placed in 1960 at the age of 18. History was consistent with intermittent bleeding from the ostomy site in the past, with first major bleed reported in 2014, 54 years after ostomy placement. Patient presented to the OSH with new onset bleed which was managed with an anticoagulant applied to the ostomy site leading to temporary cessation of bleeding and the patient was discharged. The following day the patient represented with brisk bleed that required two units of pRBC transfusions, patient was again discharged with a quick re admission due to further bleed, he then left against medical advice and reported to our center. Upon presentation patient was found to be in septic shock from a right hip septic joint. He was treated with broad spectrum antibiotics and hip incision and drainage. Patient had no further ostomy bleeding episodes until 13 days after admission at our center, when patient was found to have a moderate bleed from his ostomy. Patient was started on octreotide and silver nitrate was applied to the site. Bleeding ceased and no transfusion was required. Two days later a bleed reoccurred and GI surgery was consulted to place stomal sutures which lead to interval improvement. Patient then had an additional bleed. IR was consulted for intervention. Patient underwent successful coil embolization and sclerotherapy of two draining peristomal varices off of the right common femoral vein. Patent had no further stomal bleeding post IR embolization and was discharged from hospital 12 days after his procedure. Patient was last seen in clinic six months following discharge without any further stomal variceal bleed.
Patient 5A 59-year-old white female with PMH of Crohn’s disease status post colectomy with end ileostomy and NASH cirrhosis presented to the hospital for management of a stomal bleed. Patient had her ostomy placed in 1998. Patient was previously seen at the hospital 10 days prior to admission for bleeding from her ostomy site. This was the first reported bleed which was 14 years after ostomy placement. She underwent evaluation with double balloon enterscopy which revealed small bowel arteriovenous malformations (AVM). Patient underwent AVM ablation and received nine units of pRBC transfusions and was subsequently discharged. Patient represented to hospital with continued bleeding from her ostomy site. Upon admission patient was hemodynamically stable without evidence of ostomy bleed. Two days after this admission patient again had an ostomy bleed. She went for emergent TIPS procedure which was successful in reducing the portosystemic gradient from 13 mmHg to 4 mgHg. After TIPS procedure patient had continued, albeit reduced bleeding from stomal varices requiring an additional pRBC transfusion. She was stabilized and discharged from hospital six days post TIPS procedure. Patient has since been lost to follow up.
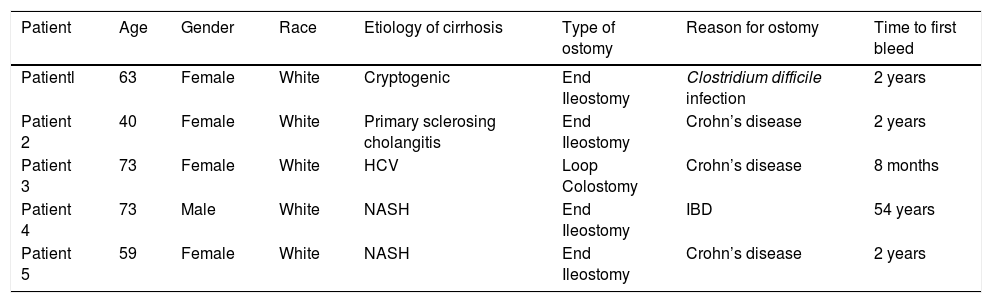
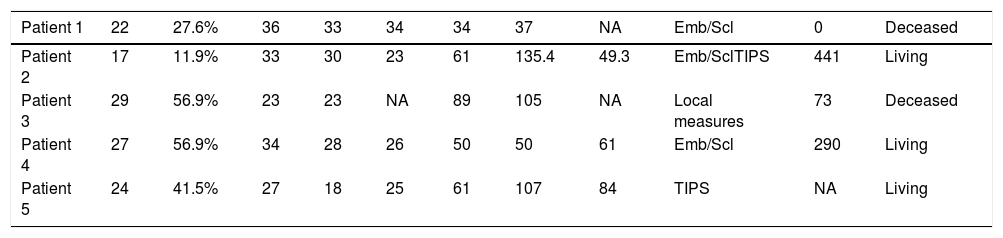
ResultsFive patients who presented to our tertiary care center with a PVB were included in this study. The average age was 61.6, 80% were female, and all were Caucasian. The mean MELD-Na on admission was 23.8. Four of the patients had an end-ileostomy and one had a loop colostomy. All patients had cirrhosis with resultant portal hypertension. The etiology of cirrhosis included one patient with PSC, one with HCV, two with NASH and one that was cryptogenic (Table 2). Therapies that were performed included one patient that received a TIPS alone, two patients that received coil embolization and sclerotherapy, and one patient that received combination of TIPS, sclerotherapy, and embolization. Hemostasis was achieved in 75% of patients that received therapy and all patients who had resolution of bleeding while in hospital were discharged home. The patient that received only sclerosant embolization continued to have bleeding and succumbed to hemorrhagic shock while in the hospital. Of the four patients that were discharged from the hospital the bleeding free survival to date is 441, 73 (this patient died on hospice), 290, and one lost to follow up (Table 3).
Patient demographics.
| Patient | Age | Gender | Race | Etiology of cirrhosis | Type of ostomy | Reason for ostomy | Time to first bleed |
|---|---|---|---|---|---|---|---|
| Patientl | 63 | Female | White | Cryptogenic | End Ileostomy | Clostridium difficile infection | 2 years |
| Patient 2 | 40 | Female | White | Primary sclerosing cholangitis | End Ileostomy | Crohn’s disease | 2 years |
| Patient 3 | 73 | Female | White | HCV | Loop Colostomy | Crohn’s disease | 8 months |
| Patient 4 | 73 | Male | White | NASH | End Ileostomy | IBD | 54 years |
| Patient 5 | 59 | Female | White | NASH | End Ileostomy | Crohn’s disease | 2 years |
Laboratory analysis, treatment modality and survival.
| Patient 1 | 22 | 27.6% | 36 | 33 | 34 | 34 | 37 | NA | Emb/Scl | 0 | Deceased |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient 2 | 17 | 11.9% | 33 | 30 | 23 | 61 | 135.4 | 49.3 | Emb/SclTIPS | 441 | Living |
| Patient 3 | 29 | 56.9% | 23 | 23 | NA | 89 | 105 | NA | Local measures | 73 | Deceased |
| Patient 4 | 27 | 56.9% | 34 | 28 | 26 | 50 | 50 | 61 | Emb/Scl | 290 | Living |
| Patient 5 | 24 | 41.5% | 27 | 18 | 25 | 61 | 107 | 84 | TIPS | NA | Living |
Parastomal bleeding is a serious potential complication in patients with prior ostomies who also have cirrhosis or other causes of increased portal pressure. The reported prevalence of PVB ranges from 3-5 to 26%.5,6 The true prevalence of PVB is difficult to define as estimates vary in the literature due to heterogeneous patient populations, observer variability, and the underlying etiology of portal hypertension.7 As a quaternary referral care center, we suspect that the prevalence of PVB at our center is consistent with the estimates described in the literature.
Diagnosis and management of PVB has not been well established. When a patient presents with PVB, first line therapy to stop bleeding can consist of application of pressure over the bleed, cauterization with silver nitrate positioning, surgical suturing and ligation.8 These locals methods have been shown to be efficient alone in controlling PVB but more often than not patients will inevitably rebleed, necessitating more invasive methods.9-12Stomal revisions have proven to be successful in controlling parastomal bleeds. Beck, et al. demonstrated that mucoutaneuous disconnections have less intraoperative blood loss and a lower overall morbidity than stomal relocations.13-15Additional interventions include sclerotherapy, endovascular embolization, ballon-occluded retrograde transvenous obliteration, splenectomy, rarely liver transplantation and TIPS. TIPS is described in the literature as the most common intervention for parastomal variceal bleed as shown in Table 1.
Despite TIPS being the most common, new methods and techniques are constantly being developed and researched to help combat the morbidity associated with PVB. Vangeli, et al. looked at 21 patients receiving either TIPS or TIPS plus embolization showed that rebleed rate in TIPS alone was 42 vs. 28% when combined with embolization.16 Absolute contraindications to TIPS procedure include pulmonary hypertension and right sided heart failure with relative contraindications being hepatic encephalopathy, sepsis, and chronic portal vein thrombosis. 17TIPS traditionally has been the preferred definitive therapy but not all patients are candidates due to the aforementioned contraindications as well as cost and technical skill required. Valaydon and Desmond describe a case where TIPS was contraindicated due to the degree of hepatic encephalopathy. The patient received coil embolization and sclerosis using Fibrovein sclerosant with successful resolution of PVB.4 Ward, et al. describe seven patients that underwent direct intrahepatic portal systemic shunt for PVB bleed management when TIPS was either unsuccessful or contraindicated.18
Additional treatment modalities include percutaneous transhepatic embolization using Oynx liquid embolic solution in conjunction with coil embolization. A case series describes the benefits of Oynx solution in helping with complete embolization of varices and tiny tributaries while utilizing coil embolization more proximally at larger varix to help achieve occlusion.19 Newer treatments include a recent case by Fergusson, et al. that described a novel use of a hemorrhoid banding device for successful control of PVB.20
Early recognition of PVB and an understanding of the availability of treatment modalities are imperative as mortality from acute variceal bleed is high. Table 3 uses data from an article by Reverter, et al. that looked at mortality of patients with acute variceal bleed based on their MELD scores. They analyzed data from 178 patients with cirrhosis and acute variceal bleed and were able to extrapolate a MELD based model to estimate mortality in cirrhotic patients that develop an acute variceal bleed.21
The treatment decisions in our case series are in accordance with what was demonstrated in the literature. Two patients underwent TIPS, while an additional patient had TIPS deferred when portal pressures were found to be unimpressive. Three patients received embolization and three patients received sclerotherapy. One patient had cessation of bleeding with local conservative measures. Notably, the patient who underwent TIPS alone had rebleed shortly after their procedure, while the patient who underwent TIPS in combination with embolization did not experience a bleed. This mirrors the aforementioned findings by Vangeli, et al.
ConclusionWith cirrhosis on the rise from hepatitis C, NASH, and other historical etiologies of cirrhosis the risk of parastomal bleeding will likely increase in those individuals with prior ostomy formations. Management of esophageal varices includes primary and secondary prophylaxis. Preventive measures such as nonselective beta blockade, esophageal varices banding and emergent therapy can include the use of Blakemore or TIPS. PVB does not currently have any primary prophylaxis and as such therapy is only initiated when bleeding arises. PVBs are something that most gastroenterologist and hepatologists will face during their career and it is important to recognize and treat them early due to high mortality rates. No clear census has been established on how to treat PVBs but a stepwise approach from least invasive to more invasive could likely be adopted in patients presenting with slow stomal variceal bleed. New therapies are constantly being developed and it is important for physicians to be up to date on therapies available to help them manage PVBs.
Abbreviations- •
AVM: atriovenous malformation.
- •
CKD: chronic kidney disease.
- •
CT: computed tomography.
- •
ESRD: end stage renal disease.
- •
GI: gastrointestinal.
- •
Hb: hemoglobin.
- •
Hct: hematocrit.
- •
HCV: hepatitis C virus.
- •
IR: interventional radiology.
- •
MELD: Model for End Stage Liver Disease.
- •
NASH: nonalcoholic steatohepatitis.
- •
OSH: outside hospital.
- •
Plt: platelets.
- •
PMH: past medical history.
- •
pRBC: packed red blood cell.
- •
PSC: primary sclerosing cholangitis.
- •
PVB: parastomal variceal bleeding.
- •
TIPS: transjugular intrahepatic portosystemic shunt.
- •
UC: ulcerative colitis.
The authors declares that there is no conflict of interest regarding the publication of this article.
GrantsNo grants to report.