Situs inversus (SI) is a rare congenital disorder with a complete mirror image of thoracic and abdominal organs. In adults with SI and decompensated cirrhosis experience with liver transplantation is limited. Orthotopic liver transplantation (OLT) in an adult with cirrhosis using a technique where the recipient liver was placed using a 90-degree rotation of the graft was previously reported by Klintmalm et al, however no other reports using this technique have been described. We report a case of a 41 year-old man with situs inversus and decompensated cirrhosis who successfully underwent OLT using this technique. The donor liver was rotated 90-degrees towards the left and easily fitted into the recipients’ fossa with the left lobe pointing toward the left lower quadrant. The patient had an uneventful recovery and has been followed for 21 months without any complications. This technique has the advantage of preventing compromise of the size of the donor liver, permits an easy reconstruction of vascular and biliary tree and in this case was associated with an excellent outcome.
Situs inversus (SI) is a congenital disorder characterized by the complete inversion of the abdominal and thoracic viscera. It is a rare condition with an estimated incidence of approximately 1/8000-1/25,000 live births.1 The underlying etiology has not been completely elucidated but an involvement of chromosomes 10, 13, and 18 involved in lateralization and polarity seem to play an important role.2 A common cause of hepatobiliary disease and cirrhosis in patients with SI is biliary atresia, a condition found in 10-20% of children with SI.3-5 In adults with SI, decompensated chronic liver disease other than biliary atresia may require orthotopic liver transplantation (OLT), but experience is limited. Although SI was previously considered a contraindication to OLT due to associated vascular malformations, several reports suggest that OLT can be successfully performed in such patients.4-17 Nonetheless performing OLT in patients with SI is technically challenging because the graft cannot be easily placed in the left side of the native liver. There are scarce reports of OLT in adults with SI and experience with these patients is limited.4,17 A previous report in an adult with decompensated cirrhosis and SI successfully used a technique involving a 90 degree rotation of the graft so it could be placed in the recipients’ left upper fossa.17 We report a case of a 41 year old man with cryptogenic cirrhosis and complete SI with dextrocardia that underwent OLT successfully with a modified technique previously described by Klintmalm et al.17
Case reportA 41 year old man with a known history of cryptogenic cirrhosis and SI with dextrocardia followed by the Liver Service presented with recurrent episodes of va-riceal bleeding and large ascites in January of 2004. Given that he had no contraindications, he was listed for liver transplantation with a model for end-stage liver disease (MELD) score of 13 (bilirubin, 1.1 mg/dL; creatinine, 1.4 mg/dL; international normalized ratio, 1.3). Physical examination revealed stigmata of cirrhosis with temporal wasting, palmar erythema, large ascites, splenomegaly, and lower extremity edema. A magnetic resonance imaging study of his abdomen confirmed total SI of all abdominal organs without any significant vascular abnormalities. In addition the liver was small, had findings consistent with cirrhosis without any liver masses and there was evidence of portal hypertension with splenomegaly (Figure 1).
Magnetic resonance imaging of the patient prior to liver transplantation. The image shows SI of abdominal organs without any significant vascular abnormalities. The liver was small and cirrhotic without any liver masses and there was evidence of portal hypertension with splenomegaly.
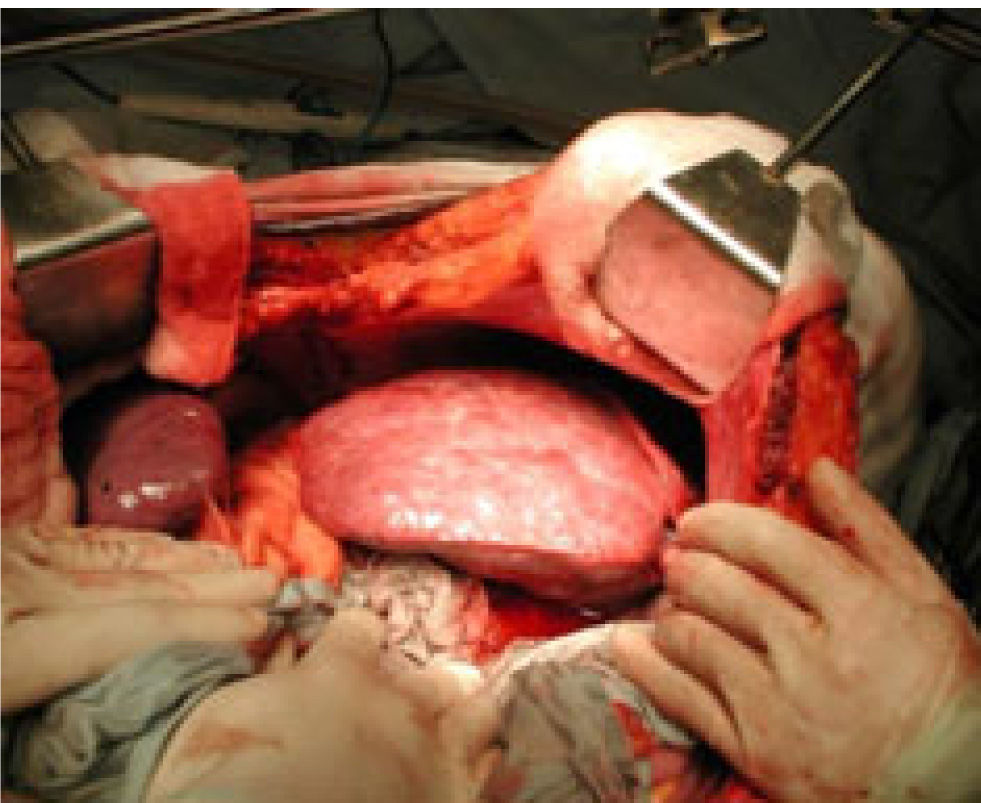
The patient underwent an OLT on April 6 of 2004. The donor was a healthy 19 year-old man (76.4 kilograms and 178 cm tall) who had sustained a severe head trauma. Procurement of the donor graft was performed using standard technique with Custodiol solution. A standard incision for OLT was performed in the recipient and complete SI of all organs was confirmed. The cirrhotic liver was found in the left upper quadrant as expected (Figure 2). No other unexpected anatomic abnormalities were found in the abdominal cavity. Large varices, splenomegaly and a prominent splenic vein indicating severe portal hypertension were present. The left and right hepatic arteries were identified and ligated and the hepatic hilium dissected. The liver was dissected from the vena cava and then the portal vein was clamped. Afterwards the hepatic veins were clamped and oversewn and the native liver removed.
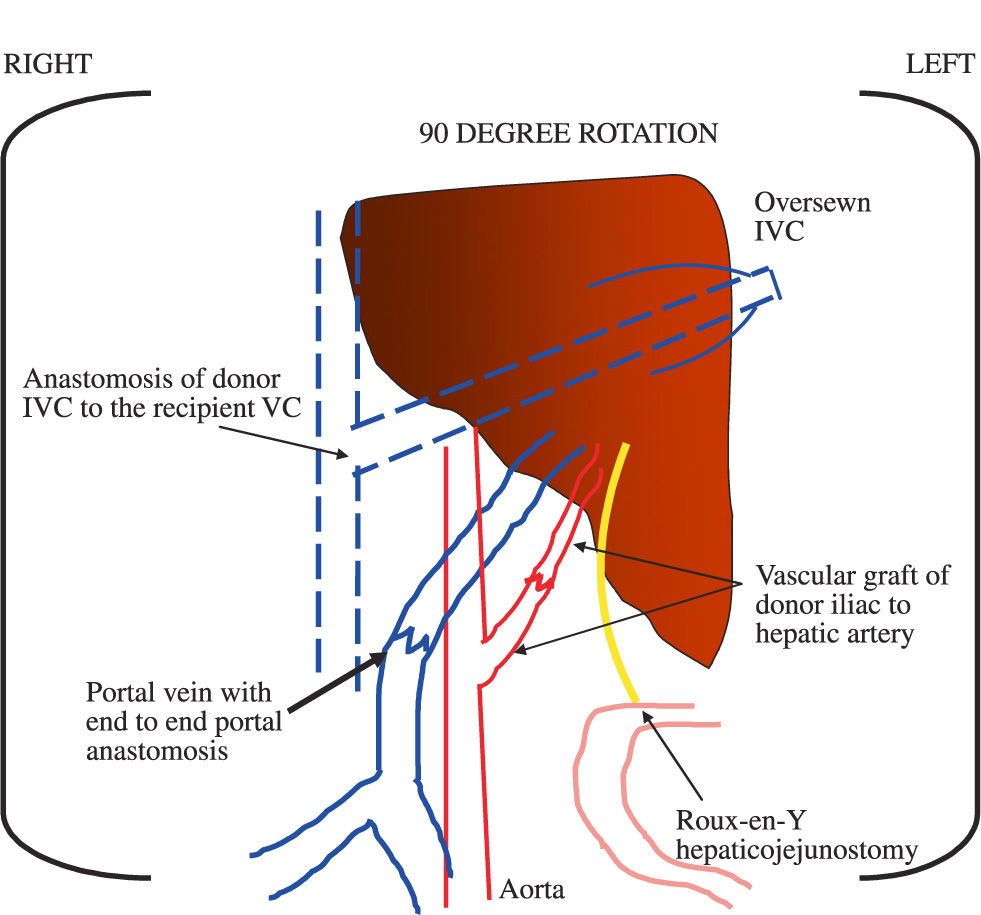
During the operation positioning of the graft was best fitted by rotating it 90 degrees to the left, thereby pointing the left lobe towards the left lower quadrant and the right lobe in the recipient hepatic fossa on the left upper quadrant of the abdomen (Figure 3) as previously described by Klintmalm et al.17 The suprahepatic vena cava of the graft was oversewn and the donor infrahepatic vena cava was sewn end-to-side to the recipient vena cava (Figure 3). An end-to-end portal vein anastomosis was performed with successful reperfusion of the graft after removal of clamps. A vascular graft using the donor iliac artery was performed from the aorta to the donor hepatic artery (Figure 3). A choledo-choledochostomy was not performed because in our experience this type of reconstruction is associated with recurrent parasitic infections and obstruction of the biliary tree in our country, therefore the biliary system was reconstructed by performing a Roux-en-Y hepaticojejunostomy (Figure 3). During the operation, the patient received a total of 8 units of packed red blood cells and 6 units of fresh frozen plasma. The operation was completed in approximately 6 hours without any major complications of bleeding or prolonged ischemia.
The patient had an uneventful recovery and within 2 days was transferred out of the Intensive Care Unit into a regular ward bed where he remained hospitalized for a total of 9 days. After transplantation the patient has remained well and only presented one episode of mild acute rejection 12 months after transplantation successfully treated with oral steroids. He has remained in excellent condition 21 months after transplantation.
DiscussionAlthough SI was considered to be an absolute contraindication to liver transplantation, experience with OLT and live-donor liver transplantation in patients with SI has significantly evolved over the past 15 years.4-17 In many centers experience with both orthotopic and live-donor liver transplantation in SI has significantly advanced, particularly in children where most cases are associated with biliary atresia. However in adults without biliary atresia experience is still limited.4,17 Nonetheless, case reports not only describe different techniques for OLT, but also for live-donor liver transplantation in adults.4
The technical difficulties in performing OLT in adults with SI not only relate to the reversed orientation of organs and hepatic vessels, but also to a small left upper fossa left behind after removing the native liver. As occurs with non-SI patients whole deceased donor graft placement is preferred and although in some cases it may be difficult it is still technically feasible. The operation described by Klintmalm et al. for adults with SI proposed a technique with common sense: placement of the liver in the empty space.17 In our opinion this is an easy way to fit the liver in the fossa left behind with several advantages. The first is that the donor liver does not need to be reduced in size; the second is that the end to end anastomoses of the IVC and portal vein to the native vena cava can be easily performed; the third is that the biliary reconstruction can be easily dealt with by either performing a choledo-choledochostomy or by creating a Roux-en-Y hepaticojejunostomy; fourth there no risk of venous outflow obstruction due to kinking of suprahe-patic vessels; and finally this technique allows the use of an even large donor liver for a small recipient in most cases. One potential limitation with this technique is the need for an intact vena cava which in many cases of patients with SI can be associated with malformations.
Although Klintmalm’s technique is recommended as the procedure of choice in SI,17 we performed two variations of operation. The first was the construction of a vascular graft between the aorta and the donor hepatic artery using the donor iliac artery. This was done because the common hepatic artery of the donor was felt to be small. This technique avoids tension between the aorta and hepatic artery and has a lesser risk of thrombosis than the use of artificial grafts.18 The second was the reconstruction of the biliary system with a Roux-en-Y hepaticojejunostomy instead of using a choledo-choledochostomy due to recurrent parasitic infections that commonly occur in our country and can obstruct the biliary tree after OLT.
In conclusion this case demonstrates that OLT in adults with SI is safe and can be successfully performed by rotating the donor liver 90 degrees towards the left and then easily fitted into the recipients’ fossa with the left lobe pointing toward the left lower quadrant. There are several technical advantages with this technique and in this case the operation was not associated with any short-term or long-term complications. Therefore we recommend OLT using the 90 degree rotation technique in adult patients with complete SI in need of liver transplantation.