Oral presentations at the XVI National Congress of the Mexican Association of Hepatology
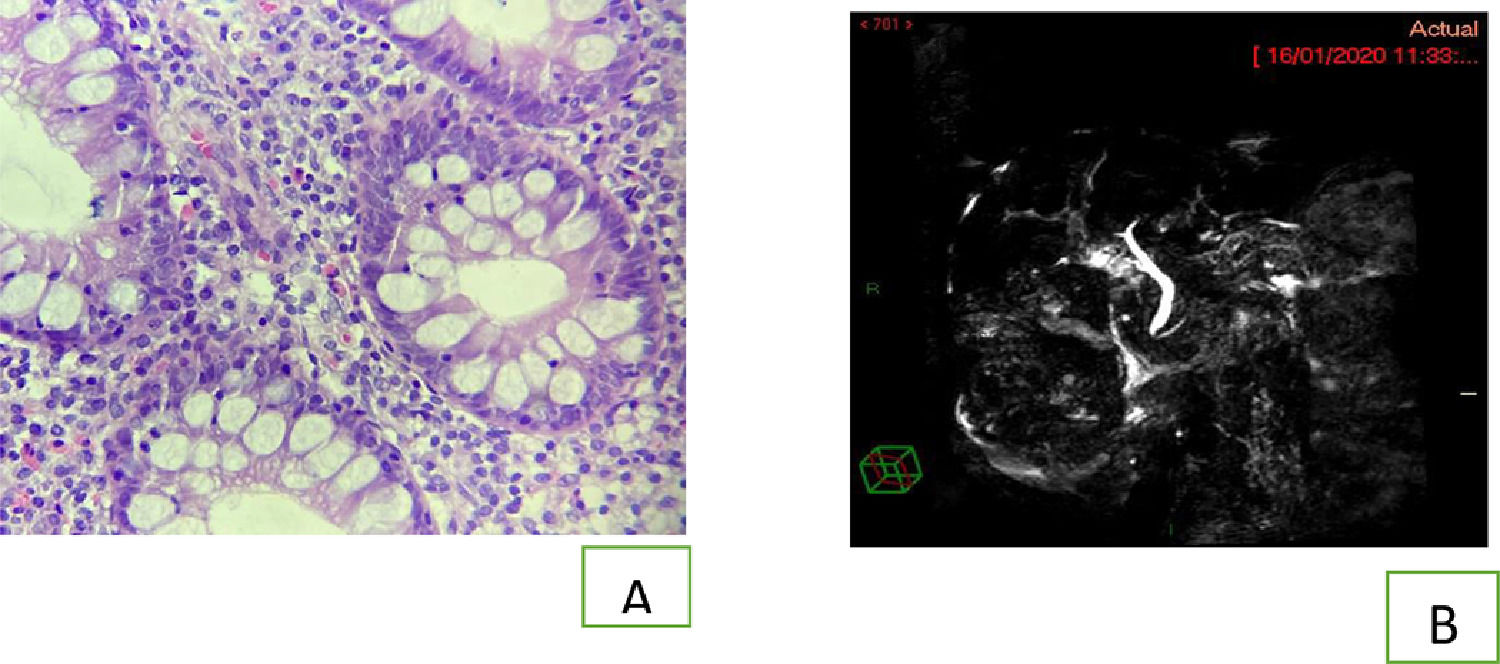
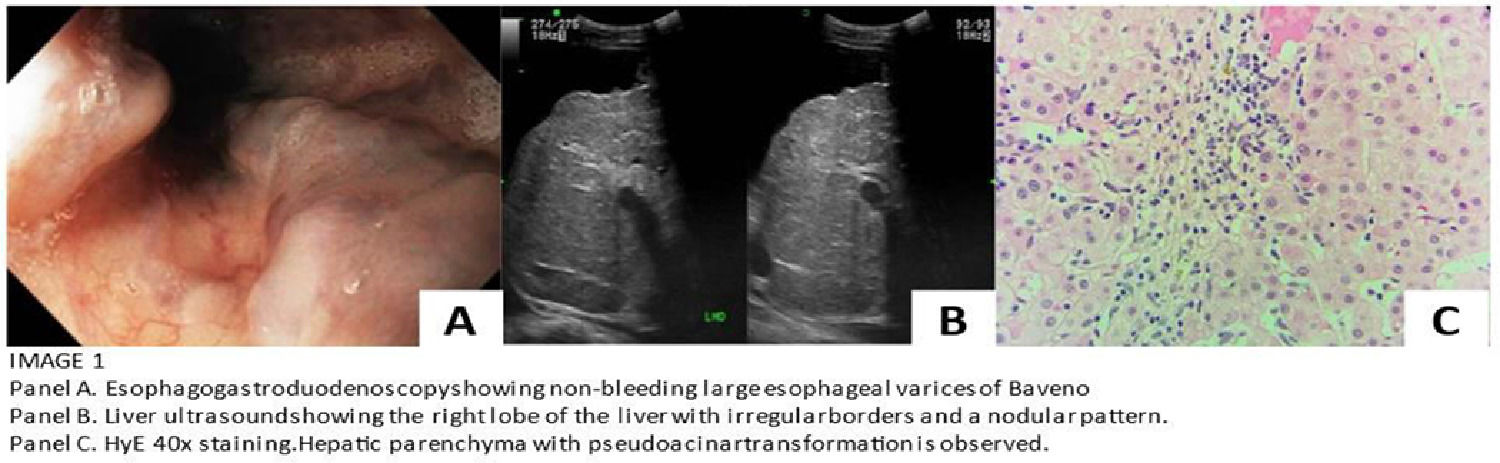
More infoLiver involvement is not unusual in patients with inflammatory bowel disease (IBD), where one third of patients have abnormal liver biochemical tests, becoming a diagnostic challenge. Primary biliary cholangitis (CPB) is an autoimmune liver disease that presents with chronic cholestasis, the presence of specific antibodies and histological findings of destructive non-suppurative cholangitis. Genetic, immunological, and environmental factors that contribute to the pathogenesis of IBD may also contribute to associated hepatobiliary disorders. Objective: Present the case of a 67-year-old woman who consulted for cholestatic symptoms. Medical record of smoking for 25 years was suspended 15 years ago with a smoking index of 5. She reported a history of weakness, asthenia, self-limited palmar and plantar pruritus of 2 years of evolution, associated with abnormal liver function tests (total bilirubin 1.8 mg / dl, INR 1.40, albumin 3.2 g / dL). The initial physical examination revealed jaundice in the sclera, palmar erythema, evidence of telangiectasia in the abdomen, collateral circulation with medusa caput, positive ascitic wave, and splenomegaly. R factor is cholestatic, with alkaline phosphatase of 416 U / L, gamma glutamyl transpeptidase 660 U / L, alanine transferase 59 U / L, for which possible viral and autoimmune causes are addressed as the first possibility, reflecting antimitochondrial antibodies with high titers (278 U / L), associated with immunoglobulin G of 2490 mg / dl and immunoglobulin M of 734 mg / dl. During her one-year follow-up, she reported the onset of diarrheal stools Bristol 6, 2 to 3 episodes per day, with occasional urgency and with inflammatory characteristics, due to the presence of mucus and blood. Infectious causes are ruled out, elevated acute phase reactants are reported, followed up with a colonoscopy and biopsy samples, reporting the presence of nonspecific proctitis, chronic colitis with focal ulceration, lymphoid aggregates, focal atrophy, and glandular distortion compatible with ulcerative colitis (UC). (Panel A) Due to the unusual association between UC and PBC, magnetic resonance cholangiography was requested, ruling out the overlap syndrome between primary biliary cholangitis and primary sclerosing cholangitis. (Panel B)
DiscussionA diverse heterogeneous group of hepatobiliary manifestations is reported in both UC and CD, and approximately 5% of adults with IBD have developed chronic liver disease. PBC is not usually associated with IBD, and concomitant reported cases are anecdotal. The presentations are different than the typical CBP without UC. PBC usually affects middle-aged women. The sex ratio is 10: 1 (female to male) and the mean age at diagnosis is 57.5 years. While the disease tends to affect men more often, with a female / male sex ratio of 2: 1 when associated with IBD. The distribution of ulcerative colitis in PBC patients is usually mild with limited bowel involvement. In a review by Tasa et al., eleven of 15 patients described left side colitis and proctitis.
ConclusionThe association between PBC and UC remains rare, as there are still few reported cases regarding the combined presentation of these diseases. Although PSC is the most specific hepatobiliary manifestation among UC patients with cholestasis, PBC should be considered in those with unexplained intrahepatic cholestasis. The use of a reliable test such as AMAs is of utmost importance to avoid misdiagnosis and/or under diagnosis.
The authors declare that there is no conflict of interest.