Intraductal papillary neoplasm of the bile duct (IPNB) is a specific entity, characterized by intraluminal growth of bile duct epithelia with a fine fibro-vascular core from microscopy [1]. IPNB has many unique characteristics in risk factor [2], pathogenesis [3,4] and disease nature [5]. The nature of IPNB includes slow growth, multiplicity [6,7], various cell types, various degrees of invasion [5,6] and various amounts of mucin production, resulting in the many characteristics of IPNB [8].
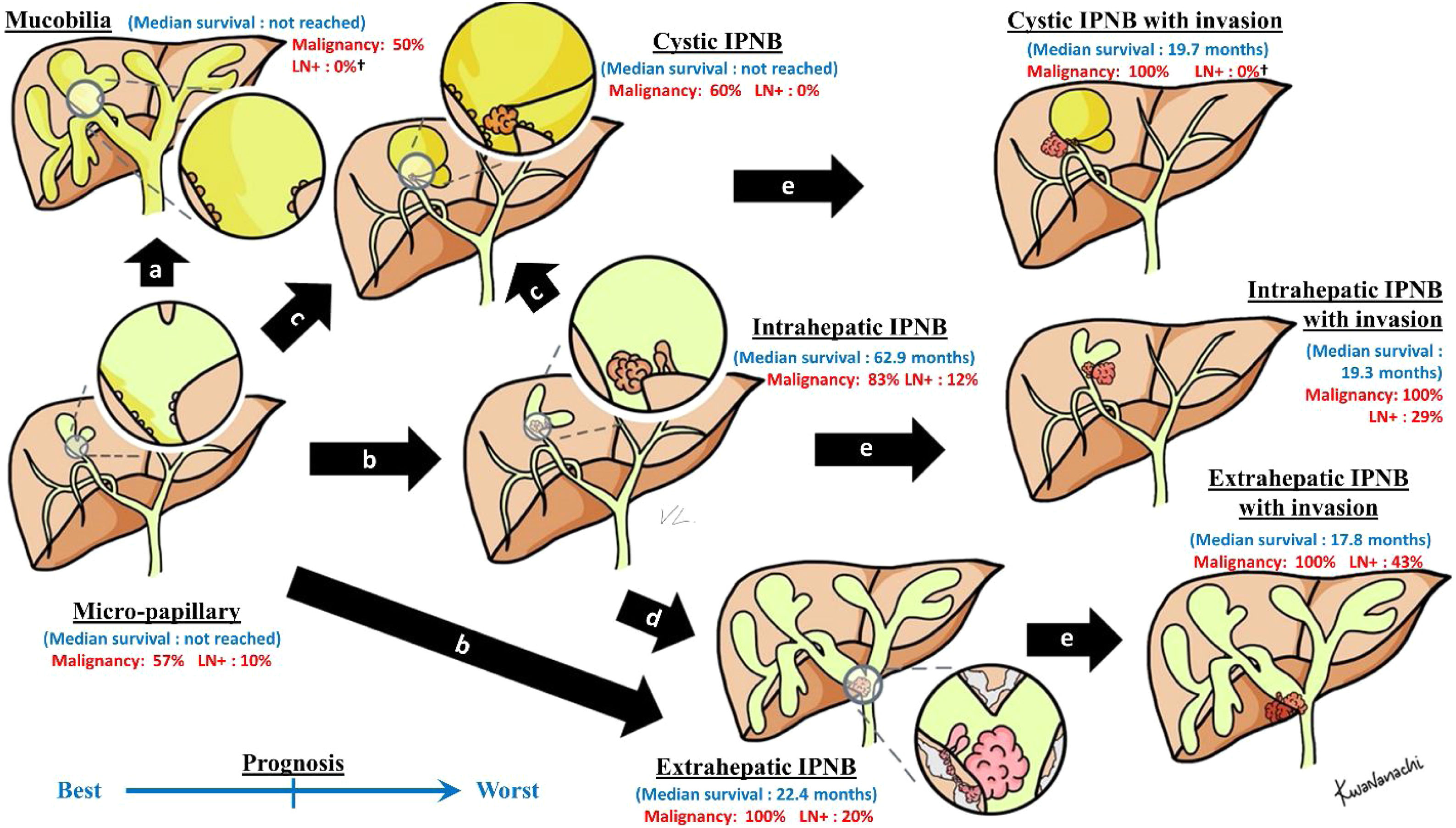
We have classified IPNB, in order to predict the patient prognosis and guide the treatment, according to its morphology, into five common subtypes [9], including (i) intrahepatic intraductal lesion (i.e., presence of an intraductal tumor with unilateral intrahepatic duct dilatation), (ii) extrahepatic intraductal lesion (i.e., presence of an intraductal tumor with bilateral intrahepatic duct dilatation), (iii) cystic variant (i.e., cystic tumor with a papillary tumor inside and the presence of bile duct communication), which has a radiological picture similar to a hepatic mucinous neoplasm [10,11], (iv) micro-papillary lesion (i.e., disproportional bile duct dilatation in the absence of any discernible tumor), and (v) macro-invasive IPNB (i.e., presence of a mass-forming tumor incorporate with intraductal tumor) [9]. However, we still believe that the progression of IPNB is more a continuous spectrum that is unable to be clearly divided type by type. Since North-Eastern Thailand is an endemic area for bile duct tumors [12], we had opportunities to find IPNB patients who did not undergo surgical resection for various reasons, allowing us to observe the in-vivo progression of IPNB. We found the progression of IPNB from one class to another. We, therefore, are proposing this progression model of IPNB (Fig. 1).
Proposed model of IPNB progression. The blue numbers indicate median survival of the patients treated by curative-intent resection of the IPNB, based on the author experience [9]. The red numbers indicate malignancy rate, and chance of lymph node involvement of curative-intent resection of the IPNB, based on the author experience, according to pathological examination [9]. †The indicated number may be imprecise due to small sample size, unpublished data. IPNB: intraductal papillary neoplasm of the bile duct, LN+: chance of lymph node involvement.
We believe that all IPNBs start from a micro-papillary type, with various degrees of mucin production. When IPNB produces a large amount of gross mucin without any bile duct obstruction by the tumor, it would present a mucobilia picture; diffuse biliary dilatation without a discernible mass (a). If the predominant progression is by intraductal tumor growth and there is a relatively low amount of gross mucin production, it would be typical IPNB; intraductal mass in dilated bile duct (b). When the degree of biliary obstruction has increased to nearly complete obstruction at any level of the intrahepatic bile duct (relative with the viscosity of the mucin), the cystic IPNB appears [13] (c). Since the hepatic hilum is the region which consists of a complicated network of peri-biliary gland [14], that enhances the progression of the tumor; IPNB with luminal extension approaching this point is usually related with a worse prognosis [9,15] (d). Some mutation makes IPNB more invasive, resulting in vertical extension through the bile duct to adjacent liver parenchyma (e), increasing the chance of lymph node involvement and distant metastasis.
To the best of our knowledge, this is the first proposed model of the progression of IPNB. Our model would explain the presence of a combined morphology, the differences in nature of each morphology of the IPNB, in terms of the chance of lymph node involvement, distant metastasis and prognosis of the patients.
Financial supportThe authors received no financial support for the manuscript.
Conflict of interestThe authors have no conflicts of interest to declare.
The authors thank (a) Dr. Kwanchanok Losuwarat for illustrating the figure, and (b) Mr. Ian Thomas for assistance with the English-language presentation of the manuscript.





![Proposed model of IPNB progression. The blue numbers indicate median survival of the patients treated by curative-intent resection of the IPNB, based on the author experience [9]. The red numbers indicate malignancy rate, and chance of lymph node involvement of curative-intent resection of the IPNB, based on the author experience, according to pathological examination [9]. †The indicated number may be imprecise due to small sample size, unpublished data. IPNB: intraductal papillary neoplasm of the bile duct, LN+: chance of lymph node involvement. Proposed model of IPNB progression. The blue numbers indicate median survival of the patients treated by curative-intent resection of the IPNB, based on the author experience [9]. The red numbers indicate malignancy rate, and chance of lymph node involvement of curative-intent resection of the IPNB, based on the author experience, according to pathological examination [9]. †The indicated number may be imprecise due to small sample size, unpublished data. IPNB: intraductal papillary neoplasm of the bile duct, LN+: chance of lymph node involvement.](https://static.elsevier.es/multimedia/16652681/000000230000000C/v3_202212060650/S1665268120302246/v3_202212060650/en/main.assets/thumbnail/gr1.jpeg?xkr=ue/ImdikoIMrsJoerZ+w96p5LBcBpyJTqfwgorxm+Ow=)




