
Edited by: Marco Arrese - Pontifical Catholic University of Chile, Santiago, Chile
More infoLiver disease poses a substantial burden in Latin America. This burden is primarily attributed to a high level of alcohol consumption and the increasing prevalence of risk factors associated with metabolic dysfunction-associated steatotic liver disease (MASLD), such as sedentary lifestyles, easy access to ultra-processed foods, obesity, and type 2 diabetes mellitus. These epidemiological trends are cause for concern, especially considering that there are significant challenges in addressing them due to disparities in access to liver disease screening and care. In this article, we aim to provide an overview of the current situation regarding liver disease in Latin America. We also discuss recent multinational proposals designed to address the growing MASLD burden via its integration into existing non-communicable diseases policies, at both local and global levels. Additionally, we emphasize the urgent need to establish effective public health policies that target both MASLD risk factors and excessive alcohol consumption. Furthermore, we discuss the development of liver transplantation programs, areas for improvement in medical education and research capabilities, and how the fostering of extensive collaboration among all stakeholders is crucial for addressing liver disease in the region.
Latin America is a region composed of 20 countries, representing around 8% of the global population and exhibiting wide diversity in terms of ethnicity and genetic background [1]. This region is characterized by pronounced economic and social inequities, despite being home to several upper-middle-income and high-income countries [1]. Some countries have a very high Human Development Index (HDI) score (≥0.800), like Chile, Argentina, Uruguay, Costa Rica, and Panama, while others only have a medium one (0.550–0.699), such as Haiti, Honduras, Guatemala, and Nicaragua, all listed in descending order [2]. Regional disparities are also reflected in inhabitant lifestyles, including their dietary patterns and alcohol use, and in healthcare accessibility. Together, these factors lead to significant variability in terms of the burden of communicable and non-communicable liver disease [3,4].
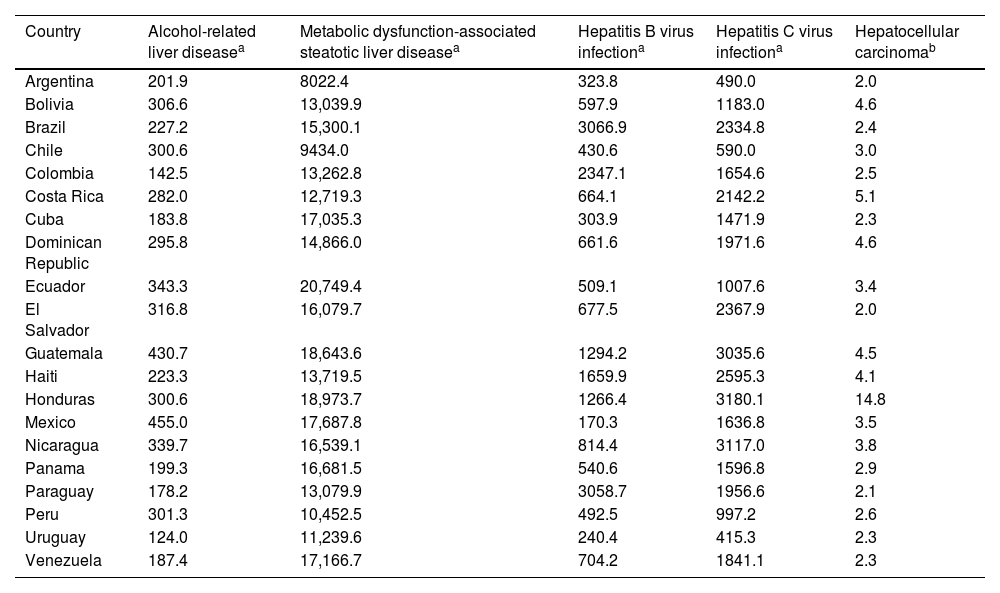
Chronic liver disease (CLD) is the second cause of years of working life lost [5] and one of the leading burdens of disease in the Americas, especially due to alcohol-related liver disease (ARLD) and metabolic dysfunction-associated steatotic liver disease (MASLD), previously known as non-alcoholic fatty liver disease (Table 1) [6,7]. Other common causes of CLD include hepatotropic viruses infection, including the hepatitis B virus (HBV) and hepatitis C virus (HCV), with their prevalence varying throughout the region [8]. However, epidemiological data on liver disease are scarce in Latin America, mainly because of a complex interplay of disease-specific, demographic, socioeconomic, and health system factors. For example, figures regarding the natural history of MASLD are based on data pertaining to Latin Americans living in the United States of America (USA), despite the fact that environmental and socioeconomic conditions may affect the course of this condition [9–12].
Age-standardized prevalence (per 100,000 inhabitants) of the leading causes of chronic liver disease in Latin America (2019); data were collected from the Global Burden of Disease database [13].
| Country | Alcohol-related liver diseasea | Metabolic dysfunction-associated steatotic liver diseasea | Hepatitis B virus infectiona | Hepatitis C virus infectiona | Hepatocellular carcinomab |
|---|---|---|---|---|---|
| Argentina | 201.9 | 8022.4 | 323.8 | 490.0 | 2.0 |
| Bolivia | 306.6 | 13,039.9 | 597.9 | 1183.0 | 4.6 |
| Brazil | 227.2 | 15,300.1 | 3066.9 | 2334.8 | 2.4 |
| Chile | 300.6 | 9434.0 | 430.6 | 590.0 | 3.0 |
| Colombia | 142.5 | 13,262.8 | 2347.1 | 1654.6 | 2.5 |
| Costa Rica | 282.0 | 12,719.3 | 664.1 | 2142.2 | 5.1 |
| Cuba | 183.8 | 17,035.3 | 303.9 | 1471.9 | 2.3 |
| Dominican Republic | 295.8 | 14,866.0 | 661.6 | 1971.6 | 4.6 |
| Ecuador | 343.3 | 20,749.4 | 509.1 | 1007.6 | 3.4 |
| El Salvador | 316.8 | 16,079.7 | 677.5 | 2367.9 | 2.0 |
| Guatemala | 430.7 | 18,643.6 | 1294.2 | 3035.6 | 4.5 |
| Haiti | 223.3 | 13,719.5 | 1659.9 | 2595.3 | 4.1 |
| Honduras | 300.6 | 18,973.7 | 1266.4 | 3180.1 | 14.8 |
| Mexico | 455.0 | 17,687.8 | 170.3 | 1636.8 | 3.5 |
| Nicaragua | 339.7 | 16,539.1 | 814.4 | 3117.0 | 3.8 |
| Panama | 199.3 | 16,681.5 | 540.6 | 1596.8 | 2.9 |
| Paraguay | 178.2 | 13,079.9 | 3058.7 | 1956.6 | 2.1 |
| Peru | 301.3 | 10,452.5 | 492.5 | 997.2 | 2.6 |
| Uruguay | 124.0 | 11,239.6 | 240.4 | 415.3 | 2.3 |
| Venezuela | 187.4 | 17,166.7 | 704.2 | 1841.1 | 2.3 |
This review explores the available data on the epidemiology of liver disease in Latin America, highlighting the differences between Latin America and other regions, such as North America, Europe, and Asia. It also discusses the main regional gaps in the public health agenda to tackle liver disease.
2Risk factors for liver disease in Latin AmericaRegionally, there are multiple factors that contribute to the burden of liver disease. For instance, social determinants of health (SDoH), such as income, social protection, education, food insecurity, and the built environment play a key role in people's dietary, physical activity, alcohol use, and access to treatment patterns, all of which are linked to liver disease prevalence and outcomes. SDoH are largely significant in Latin America, as the region is characterized by deleterious colonial legacies, enormous socioeconomic disparities, vast social injustice, and far-reaching health inequities [14]. Furthermore, environmental aspects like exposure to hepatotropic viruses, genetic elements, and metabolic dysfunction risk factors, including overweight, obesity, and type 2 diabetes mellitus (T2DM), all impact the prevalence and outcomes of liver disease regionally [3]. These factors, described in detail below, can interact synergistically and lead to fibrosis progression, cirrhosis, and hepatocellular carcinoma (HCC) (Fig. 1).
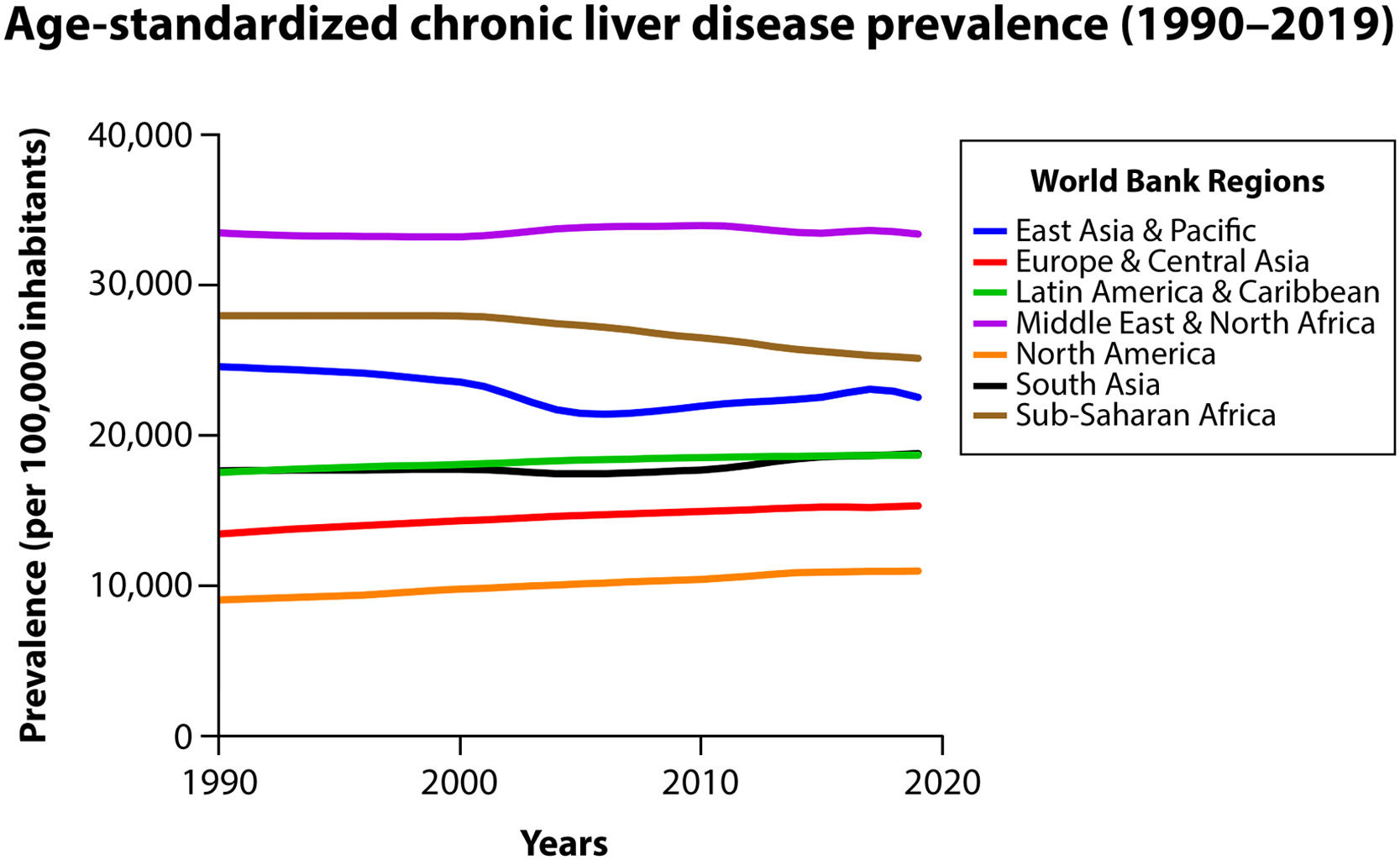
Trends in age-standardized prevalence of chronic liver disease (including all causes) among the different World Bank regions (1990–2019); data were collected from the Global Burden of Disease database [13].
Dietary intake varies widely across Latin America, shaped by a complex interplay of cultural, socioeconomic, and environmental factors [15,16]. However, despite regional variance, overall diet quality in the region is suboptimal. A global diet quality study of 185 countries found that the 2018 mean Alternative Healthy Eating Index, a validated metric of diet quality which ranges from 0 to 100, was lowest in this region at 30.3 (95% uncertainty interval [UI], 28.7–32.2); meanwhile, the global average was 40.3 (39.4–41.3) and the highest score was seen in South Asia at 45.7 (43.8–49.3) [15]. Moreover, the Latin American Study of Nutrition and Health, which includes eight countries (Argentina, Brazil, Chile, Colombia, Costa Rica, Ecuador, Peru, and Venezuela) found that less than 3.5% of 9218 individuals met the optimal intake level of nutritious food like vegetables, nuts, whole grains, fish, and yogurt [16].
Since the 1980s, Latin America has witnessed a profound nutrition transition. Diets that were traditionally rich in vegetables, legumes, and grains have been replaced by elevated intakes of processed foods high in fat and sugar [17], which are items that are more typical of the so-called Western dietary pattern, which increases the risk of MASLD by 56%. In fact, Latin Americans consume more than triple the amount of added sugar recommended by the World Health Organization (WHO) and three of the world's five highest sugar-sweetened beverage-consuming nations are found in the region [17].
As for physical activity, a major player in preventing and treating MASLD, sedentarism, favored by factors including urbanization and increasing screen time, is another critical concern in the region [18]. Latin America has the highest prevalence of insufficient physical activity among adults at 39.1% (95% UI 37.8–40.6) regionally, whereas the global prevalence sits at 27.5% (25.0–32.2) and Oceania has the lowest prevalence at 16.3% (14.3–20.7) [19]. In gender terms, Latin American women exhibit a higher prevalence of insufficient physical activity at 43.7% (42.9–46.5) compared to men at 34.3% (32.5–35.5). As for adolescents, only 15% meet physical activity recommendations in the region [20].
2.2Alcohol consumptionThe Americas is the second region worldwide with the highest prevalence of alcohol use disorders (AUDs), at 8.2% of those aged ≥15 years old, especially due to intake rates in Latin American countries such as Argentina, Chile, and Uruguay; Europe has the highest prevalence in this regard, at 8.8% [21]. Within the same age group, Latin American per capita consumption of alcohol is estimated at 6.8 liters of pure alcohol, while global estimates average 6.4 liters [22], with 4.9% of Latin Americans having an AUD [23]. Gender wise, Latin American men have a higher prevalence of AUDs than women (7.8% versus 2.0%, respectively, also among those aged ≥15 years old); similar proportions have been observed on a global scale, with 8.6% of men and 1.7% of women having an AUD [6,22].
Current evidence suggests that alcohol use patterns can lead to the development and progression of ARLD. A systematic review of 5 studies comparing daily versus non-daily alcohol intake demonstrated that daily alcohol consumption was associated with a significant increase in the risk of cirrhosis compared to non-daily alcohol intake, with a pooled relative risk of 1.71 for men and 1.56 for women. This suggests that days of abstinence, so-called “liver holidays”, may decrease the impact of alcohol intake on the liver [24]. Harmful thresholds of alcohol consumption remain ill-defined in the literature and further research is needed to establish precise amounts that determine excessive risk for liver disease development in specific populations. More research is also required to better characterize the differences among distinct types of alcohol in terms of how they impact the risk of developing liver disease.
Alcohol use can impact liver diseases other than ARLD. For example, a modeling study exploring the association between alcohol intake and CLD in the USA demonstrated that alcohol use caused 1700 (95% UI 1000–2500) acute HBV and HCV infections attributable to heavy alcohol intake episodes, as well as 14,000 (5900–19,500) chronic HBV and 1700 (700–2400) chronic HCV infections resulting from heavy alcohol use interfering with spontaneous infection clearance; alcohol intake and its interactions with other risk factors (obesity, HBV, and HCV) also led to 54,500 (50,900–58,400) new cirrhosis cases [25].
2.3Obesity and metabolic dysfunctionIn recent years, Latin America has had a substantial increase in the prevalence of obesity, a significant risk factor for developing CLD, especially in individuals of lower socioeconomic status (SES) [26]. This upward obesity trend, along with an overweight rising prevalence, pose a major public health challenge in Latin America [27,28]. In fact, Latin America has one of the highest prevalence rates worldwide, with 57% of the adult population (54% of men and 70% of women) being overweight and 19% being obese (15% of men and 24% of women) [29,30]. Countries with the highest prevalence of obesity in those aged ≥20 years old are Chile (22.0% in men and 30.3% in women), Mexico (20.6% in men and 32.7% in women), and Uruguay (23.3% in men and 25.4% in women) [31]. Figures in children and adolescents are also alarming, with 16% of children being overweight or obese in the region [32] and, among those aged <20 years old, estimates showing that countries with the highest obesity rates are: Uruguay – 9.7% in boys and 18.1% in girls, Chile – 11.9% in boys and 12.4% in girls, and Mexico – 10.5% in boys and 9.8% in girls [26,32].
As for metabolic syndrome (MetS), which is characterized by obesity, high blood pressure, hyperglycemia, and dyslipidemia, the prevalence among those aged 18–65 years old in Latin America sits at 24.9% (range: 18.8–43.3), with the figure being 25.3% in women and 23.2% in men [33,34]. Additionally, a cross-sectional study including individuals aged 25–64 years old in seven Latin American cities exhibited an overall prevalence of MetS of 21% [35]. The cities with the highest prevalence were Mexico City (27%), Barquisimeto (26%), Santiago (21%), and Bogota (20%), while Lima (18%), Buenos Aires (17%), and Quito (14%) showed the lowest prevalence [35].
2.4GeneticsCertain genetic polymorphisms have been associated with the development of liver disease and its progression. One of the most relevant polymorphisms is the patatin-like phospholipase domain-containing protein 3 (PNPLA3) nonsynonymous gene variant (rs738409 c.444 C>G p.I148M). This PNPLA3 high-risk variant has been robustly related to steatosis, steatohepatitis, and fibrosis in MASLD and ARLD patients [36–38]; it has also been linked to HCC in both conditions [39,40]. Moreover, a recent analysis of 414,209 United Kingdom Biobank study participants found a synergistic relationship between the PNPLA3 I148M variant, obesity, and excessive alcohol intake and an increased risk of cirrhosis, HCC, and liver disease-related mortality [41]. This variant has also been linked with liver fibrosis in patients with HCV and autoimmune hepatitis (AIH) [42,43].
The prevalence of the PNPLA3 p.I148M variant is notably high in Latin America, compared to other regions. For instance, a systematic clinical review reported that the highest frequency of this variant was found in Latin Americans at 48.4%, while the figure for all five regions studied was 26.2% and the lowest frequency occurred in Africans at 11.8% [39]. In Chile, the frequency of the variant is around 59% in the general population [44], while Argentina exhibits a frequency of 63.7% [45]. In recent years, regional assessments of the impact of this variant have been undertaken. Findings have shown that, for example, Amerindian populations in Mexico exhibit a predisposition towards and increased severity of ARLD in the presence of this variant [46,47], as do individuals with Hispanic ancestry living in the USA [48,49].
There are other genetic variants involved in the development of liver disease. Of note, the transmembrane 6 superfamily member 2 (TM6SF2) rs58542926 C>T variant has been associated with increased hepatic triglyceride content and fibrosis and cirrhosis progression in MASLD and ARLD [50,51]. However, data on the frequency of these in Latin America are scarce. In Brazil, a study including MASLD patients found TM6SF2 CC, CT, and TT genotype frequencies of 83%, 15%, and 0.7%, respectively, but these were not associated with MASLD susceptibility and progressive histological forms [52]. In Chile, a study of chronic HCV patients showed a prevalence of the TM6SF2 CC and CT variants of 90.2% and 9.8%, respectively, but no association was found between these and the risk of steatosis or fibrosis [53]. Other genetic factors, including the membrane-bound O-acyltransferase domain-containing 7 and 17-beta hydroxysteroid dehydrogenase 13 genes, have been demonstrated to have an important role in increasing the risk of steatosis, fibrosis, and HCC in MASLD and ARLD patients [54–56], but their frequency in Latin America is unknown.
3The evolving burden of liver disease: moving towards non-communicable diseases3.1CirrhosisCirrhosis is one of the leading causes of death worldwide, being responsible for 2.4% of global deaths in 2019, according to WHO [57]. Prevalence figures for Latin America are limited but Global Burden of Disease (GBD) data suggest that the prevalence can reach up to 2.0% among the general population [58]. In Europe, it has been estimated at 0.3–0.8% according to some population-based studies, which have evaluated the prevalence of cirrhosis using non-invasive tests [59]. Several studies conducted in the Americas have shown a shift in the etiological cause of cirrhosis in recent decades [60,61]. This is likely in relation to the epidemiological changes described in the sections below.
3.2Alcohol-related liver diseaseARLD represents a significant global health concern, especially in Western countries. A recent systematic review of 35 studies including 513,278 participants found an ARLD prevalence of 3.5% in the overall population, 2.6% in primary care, and 51.0% in patients with an underlying AUD, with the prevalence of cirrhosis due to ARLD being 0.3%, 1.7%, and 12.9%, respectively [62]. In Latin America, GBD data placed the prevalence of alcohol-related cirrhosis at 0.29% in 2019, a figure which has remained stable over the last decades. ARLD is the leading cause of cirrhosis in Argentina, Brazil, Chile, Mexico, and Peru [21] and accounts for about 53% of cirrhosis cases in the region [63].
Alcohol use can also interact with risk factors for other liver diseases like MASLD, HBV, and HCV, leading to a higher burden of liver disease [25]. Alcohol-related hepatitis (ARH), characterized by an abrupt onset of jaundice, malaise, decompensated liver disease, and coagulopathy, is another acute consequence of alcohol misuse [64–67]. Severe ARH episodes have elevated mortality in the short and long term, with rates having been as high as 43% at 6 months in a global cohort [68]. Preliminary Latin American data showed that ARH patients had survival rates of 75% at 30 days, which dropped to 62.8% at 90 days, and extremely low rates of access to early liver transplantation, at only 3.2% [69]. Although ARH incidence data are scarce, studies on Caucasian and Hispanic populations suggest that 10–35% of ALD patients develop an ARH episode [65].
3.3Metabolic dysfunction-associated steatotic liver diseaseIn recent decades, the world has seen a significant shift in the burden of liver disease, with steatotic liver disease (SLD, formerly known as fatty liver disease) becoming the leading liver disease, with MASLD having a global prevalence of 38% [70,71]. A recent systematic review involving 63 studies and over 1.2 million people found that overweight and obese individuals, cigarette smokers, and males had a 3-, 1.7-, and 1.6-fold higher MASLD risk, respectively [72]. A recent systematic review and meta-analysis concluded that the prevalence of MASLD in Latin America is around 24% among the general population [73]. The prevalence of MASLD in South America is one of the highest worldwide at 35.7%, with this region having one of the most rapid annual prevalence changes globally, at 2.7% [71]. Studies have estimated the MASLD prevalence in Brazil, Colombia, Chile, and Mexico to be 35.2%, 26.6%, 23.0%, and 17.0%, respectively [12,74]. Data have suggested that MASLD severity may be greater in Latin Americans, but more data are needed to support this observation [75].
This upward trend in MASLD prevalence correlates with the rising prevalence of T2DM, which is particularly high in Chile and Mexico (8.6% and 13.5%, respectively), overweight, and obesity [76]. Of note, metabolic dysfunction can interact with alcohol, increasing the risk of MASLD long-term [77]. A recent nomenclature change consensus process in the SLD field endorsed by the Latin American, American, and European societies on liver disease proposed the inclusion of a new disease category, MetALD, in an aim to describe those patients at the intersection between MASLD and ARLD [7,77]. Although MetALD is an innovative concept, further research in Latin America is required to establish the natural history of patients belonging to this subgroup, as well as to define the thresholds of alcohol use associated with liver damage in individuals with metabolic dysfunction.
3.4Hepatitis B and C virus infectionThe global HBV burden is decreasing worldwide, in part due to pre-transfusion testing, effective antiviral agents, and widespread anti-HBV vaccination at birth [78]. In 2019, GBD data demonstrated an acute HBV infection incidence of 1002 per 100,000 inhabitants globally, which was lower in Latin America at 463 per 100,000 inhabitants. As for CLD due to HBV infection, the estimated age-standardized prevalence was 1694 per 100,000 inhabitants in 2019 in Latin America. However, despite there being an intermediately high endemicity of HBV in the region, there are some areas with high endemicity, including the Amazon basin region of northern Brazil, Colombia, Peru, and Venezuela, northwestern Argentina, Haiti, and the Dominican Republic [3]. According to the WHO Global Health Observatory, global HBV immunization coverage among 1-year-olds was 84% in 2022, with similar coverage in the Americas at 83%. As for hepatitis D virus (HDV) infection, which can only exist in the presence of HBV, significant data gaps exist. It has been estimated that anti-HDV prevalence among people with HBV surface antigen ranges from 2.9–22.3%, with higher rates being found in areas such as northern Brazil and the western Amazon region [79–81].
Chronic HCV infection rates are low in Latin America. Before the direct-acting antiviral (DAA) era, HCV prevalence was estimated to be 0.9–1.7% [82]. DAA use has changed the natural history of chronic HCV infection, but several surveillance and treatment access issues impede progress with regard to achieving the WHO goal of eliminating viral hepatitis as a public health threat by 2030 [83].
3.5Autoimmune liver diseasesAIH and primary biliary cholangitis (PBC) are the most prevalent autoimmune liver diseases globally, while primary sclerosing cholangitis (PSC) is less prevalent [84]. Unfortunately, epidemiological data on these conditions are extremely scarce in Latin America and most have been extrapolated from the USA. A recent study from the USA estimated that the prevalence of AIH sits at 31.2 per 100,000 inhabitants, which was higher in females and individuals aged >65 years old [85]. When this prevalence was compared among races and ethnicities, data showed that Hispanics had a lower prevalence compared to Caucasians. A Chilean cohort study showed that AIH is a frequent cause for liver transplantation, with a frequency of 13% in adult liver transplant candidates [86]. In Argentinean adults, AIH explains 26% of acute liver failure cases [87].
Global incidence and prevalence of PBC are estimated at 1.76 and 14.60 per 100,000 inhabitants, respectively [88]. Evidence from a multicenter study in the USA of PBC patients suggested that Hispanics could have more frequent progression to advanced liver disease, ascites, hepatic encephalopathy, and variceal bleeding than Caucasians [89]. A cross-sectional study demonstrated that Hispanics with PBC had an increased prevalence of overlap syndrome, reduced response to ursodeoxycholic acid treatment, and more frequent complications of portal hypertension than non-Hispanic patients [90]. A Mexican study including 78 patients with PBC demonstrated that 62.8% were positive for an additional autoimmune disease, which was a slightly higher association than that found in other regions [91]. The most common autoimmune-associated conditions were Sjögren's syndrome, hypothyroidism, Raynaud´s syndrome, CREST (calcinosis, Raynaud's phenomenon, esophageal dysmotility, sclerodactyly, and telangiectasia) syndrome, and rheumatoid arthritis. Healthcare access disparities in Hispanic patients with PBC can explain some of these differences [86]. A cross-sectional study of 377 hospitalized cirrhotic patients from 65 centers in 13 Latin American countries showed that 6% of admitted patients had AIH, while 3% had PBC and only 1% had PSC [87].
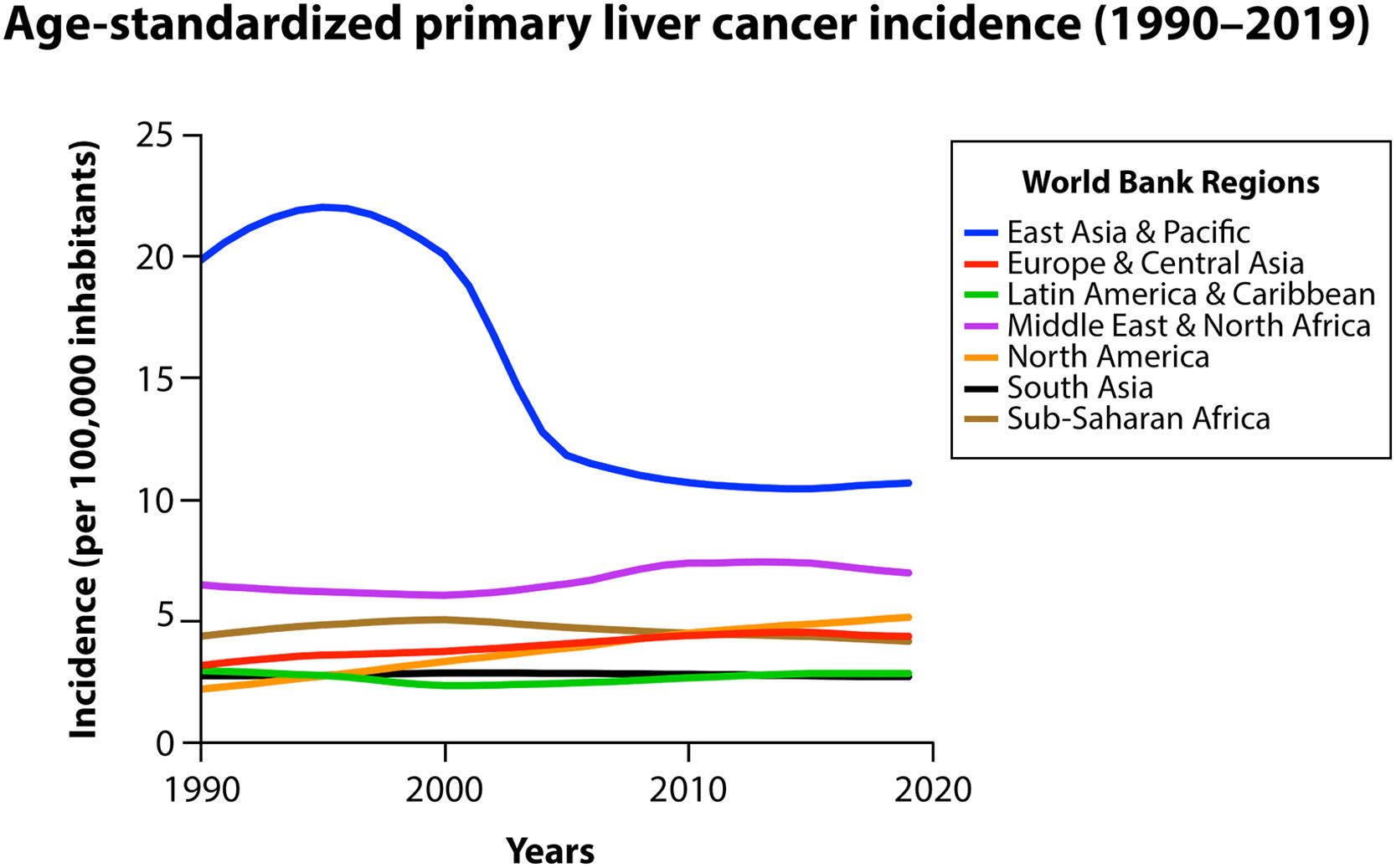
3.6Hepatocellular carcinoma and other neoplasmsAround 85% of primary liver cancers globally are due to HCC [92]. HCC was the sixth most diagnosed cancer and the third leading cause of cancer mortality in 2020 and 4.6% of these deaths occurred in Latin America [92]. HCC is a high lethality cancer in this region, with a ratio between incidence and mortality close to 1 [92]. Regionally, the most common causes of HCC are HCV infection and ARLD, similar to what is observed in Europe [93,94]. However, in some areas of Brazil and Peru HBV infection is a leading cause of HCC at 38% and 34%, respectively. Nonetheless, the epidemiology of HCC is evolving, as MASLD is rapidly rising as a cause in Latin America, and this trend will probably be sustained in the next decades, in a similar fashion to North America (Fig. 2) [94–96]. Unfortunately, around one-third of patients with HCC in Latin America will be diagnosed incidentally during advanced stages of disease and outside of surveillance programs [93]. A retrospective cohort study of 14 South American centers in 6 countries demonstrated that only 47% of HCC cases were diagnosed through such programs [97].
Trends in age-standardized incidence of primary liver cancer among the different World Bank regions (1990–2019); data were collected from the Global Burden of Disease database [13].
Acute liver failure (ALF), also known as fulminant hepatic failure, is characterized by severe acute or subacute temporary liver damage in patients without a prior history of CLD. Although data in Latin America are scarce, a Brazilian retrospective study demonstrated that, between 2006–2015 and among 325 adult patients, the most frequent causes of ALF were cryptogenic (34%), drug-induced liver injury (DILI) (26%), AIH (18%), acute HBV infection (8%), Wilson's disease (6%), hepatitis A virus (HAV) infection (4%), acetaminophen overdose (1%), and acute pregnancy steatotic liver (1%) [98]. The main causes of DILI in this cohort were anti-tuberculosis regimen (21%), non-steroidal anti-inflammatory drug (21%), and antibiotic (19%) intake [98]. An Argentinian study including 363 adult patients who underwent liver transplantation due to ALF between 1998–2016 showed that the main etiology was cryptogenic (28.3%), followed by AIH (25%), HBV (17%), non-acetaminophen DILI (14%), and HAV 1.1% [99].
3.8Acute-on-chronic liver failureAcute-on-chronic (ACLF) represents a clinical syndrome characterized by a sudden worsening of the clinical condition of patients with cirrhosis [100]. Patients with ACLF rapidly develop multi-organ failure and exhibit high risk of short-term death [101]. Due to the fact that ACLF is a relatively novel concept, its epidemiology is not well known. Prevalence of ACLF differs throughout global regions and is driven by the etiology of the underlying CLD and ACLF triggers [102]. In a recent study analyzing a prospective cohort of 1274 patients from seven Latin American countries, it was found that Native American ancestry and race were factors independently associated with ACLF [103]. More research on the features and burden of ACLF is needed in Latin America.
3.9Drug-induced liver injuryDILI, which is primarily related to exposure to common drugs but also to other substances like dietary supplements and less commonly to xenobitoics, has a broad spectrum of phenotypes and varying disease severity. Most cases worldwide are associated with anti-infectious agents [104]. However, DILI´s precise global epidemiology is unknown. Extensive efforts to establish large-scale registries have been undertaken in USA, Latin America, and Europe [105–107]. Based on data from these registries and other sources, it has been estimated that DILI is a relatively infrequent liver disorder, with an annual incidence ranging from 13–19 cases per 100,000 inhabitants [108]. The Latin American DILI registry is an ongoing initiative aimed at raising awareness about it and herbal-induced liver injury. The latter is of particular significance for a region that is characterized by a high rate of herb consumption, which may be on the rise [98]. It is thus imperative to review regulatory aspects relating to the use of herbal supplements in Latin America, following Europe's lead, which has undertaken similar endeavors [108].
4Healthcare access disparitiesCLD is particularly concerning in Latin America, as there are prominent healthcare disparities [3]. A myriad of issues, including socioeconomic inequalities with regard to factors like access to education, healthcare infrastructure, and medical treatment can all contribute to these disparities [109], which have been specifically observed with regard to some conditions. In ARLD, for instance, epidemiological evidence suggests that the alcohol-harm paradox, which is a phenomenon where people of low SES tend to experience greater alcohol-related harm than those of high SES, even at lower levels of alcohol intake, is present at a country level [110,111]. Therefore, low- and lower-middle-income countries can experience a higher AUD prevalence, even when the amount of alcohol consumption is the same or lower than in countries of higher income [23,112]. In countries outside Latin America, having Hispanic heritage has also been linked with disparities. For example, a recent study including USA 2015–2021 data showed that Hispanics had an increased risk of waitlist mortality [113].
Furthermore, a significant proportion of physicians have little awareness about CLD in Latin America, which results in an underestimation of its prevalence and associated risks [27]. For instance, MASLD awareness is low among physicians and also patients, despite the common presence of metabolic risk factors. This leads to underdiagnosing, under-referring, and delayed treatment of patients at risk of disease progression [114]. Low awareness can also contribute to the under-recording of MASLD in electronic medical records, affecting epidemiological estimates and resource allocation [115]. Moreover, the fragmented regional healthcare systems that exhibit poor communication throughout do not enable the creation of multidisciplinary teams for tackling liver disease.
In terms of treatment, access is essential. Although great advances have been made in treating liver disease regionally, especially in HCV infection and HCC management, a significant proportion of patients have suboptimal treatment access due to factors like having a low income or living in deprived or rural areas [87,116]. For example, only a few countries in the region guarantee universal DAA access for the treatment of HCV infection, despite the advent of generic drugs [83,117]. As for HCC, access to transarterial chemoembolization, prior to sorafenib initiation, is lower compared to other regions [116,118]. Globally, patients with decompensated cirrhosis from low-income countries experience higher mortality than those from high-income countries, independent of medical risk factors [119], which is likely due to disparities in access to essential diagnostic and treatment measures. Strategies to overcome these barriers include carrying out cost-effectiveness analyses, health technology assessments, and collective negotiations and using generic and biosimilar treatment via flexible patent laws [120].
As for liver transplantation outcomes, Latin American data are comparable to other regions [121,122]. Nonetheless, despite the fact that, for example, Argentina's 1-month post-liver transplantation survival rate increased from 70% to 82% in the last two decades, all while waitlist mortality decreased [99], significant barriers to liver donation, together with inadequate financial and legislative support, can threaten regional liver transplantation practices [123]. Latin America's donor rate is lower compared to Europe or North America, and is extremely low in some countries. This leads to disparities in liver transplantion, with Argentina and Brazil having an annual liver transplantation rate of >10 transplants per million inhabitants, while Venezuela, the Dominican Republic, Paraguay, and Bolivia only have a rate of 0.2–0.4 and Guatemala, Trinidad and Tobago, Honduras, Nicaragua, El Salvador, and Haiti do not routinely perform liver transplantation [124,125]. Low donor rates in Chile result in around 38% of patients being dropped from transplantation due to disease progression or waitlist death, despite income level and Model for End-Stage Liver Disease score system utilization [122,126]. Efforts and policies are thus needed to improve donation rates and liver transplantion outcomes [122,127].
5The global and regional public health agenda for liver diseaseLiver diseases like MASLD only began to receive widespread attention as of about five years ago, in relation to the policies needed to address it [128] and its recognition as a global public health threat [129]. Others, such as HBV and HCV, received such recognition well before and in 2016 WHO set out a global health sector strategy to end viral hepatitis [130]. While WHO has championed viral hepatitis elimination, it has been surprisingly silent on MASLD and metabolic dysfunction-associated steatohepatitis (MASH), with no mentions of these in their global non-communicable disease (NCD) action plan and implementation roadmap or in related publications like their framework for meaningful engagement of people living with NCDs and mental health and neurological conditions [128,131,132].
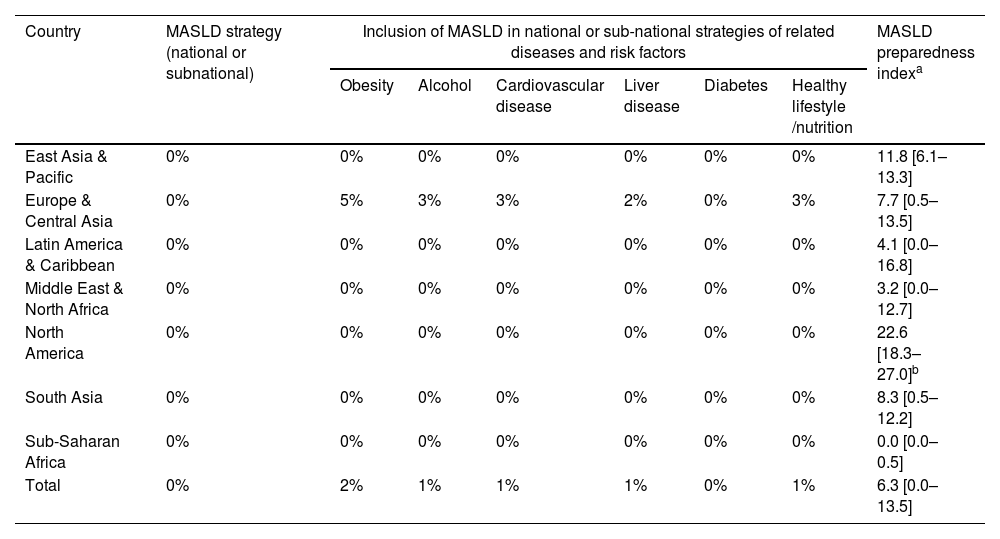
In a study of 102 countries, MASLD and MASH were found to be greatly absent from national and global health agendas and around a third of countries scored zero, out of 100, on an index measuring preparedness to address these; regionally, no Latin American country scored >26 on this index (Table 2) [128]. MASLD national clinical guidelines were present in only 31% of countries, with Latin America and North America having the highest proportion of countries with such guidelines, at 50% each. However, of the countries that did not respond to the survey, Latin America had the highest regional proportion at 35%, which potentially points to the existence of gaps in disease awareness and data collection regionally. This study underscored the need for collective and coordinated efforts to address MASLD and MASH and to promote disease policy initiatives at national and global levels.
The MASLD strategy review and preparedness index among the different World Bank regions.
| Country | MASLD strategy (national or subnational) | Inclusion of MASLD in national or sub-national strategies of related diseases and risk factors | MASLD preparedness indexa | |||||
|---|---|---|---|---|---|---|---|---|
| Obesity | Alcohol | Cardiovascular disease | Liver disease | Diabetes | Healthy lifestyle /nutrition | |||
| East Asia & Pacific | 0% | 0% | 0% | 0% | 0% | 0% | 0% | 11.8 [6.1–13.3] |
| Europe & Central Asia | 0% | 5% | 3% | 3% | 2% | 0% | 3% | 7.7 [0.5–13.5] |
| Latin America & Caribbean | 0% | 0% | 0% | 0% | 0% | 0% | 0% | 4.1 [0.0–16.8] |
| Middle East & North Africa | 0% | 0% | 0% | 0% | 0% | 0% | 0% | 3.2 [0.0–12.7] |
| North America | 0% | 0% | 0% | 0% | 0% | 0% | 0% | 22.6 [18.3–27.0]b |
| South Asia | 0% | 0% | 0% | 0% | 0% | 0% | 0% | 8.3 [0.5–12.2] |
| Sub-Saharan Africa | 0% | 0% | 0% | 0% | 0% | 0% | 0% | 0.0 [0.0–0.5] |
| Total | 0% | 2% | 1% | 1% | 1% | 0% | 1% | 6.3 [0.0–13.5] |
MASLD, metabolic dysfunction-associated steatotic liver disease.
To address the shortcomings highlighted by the MASLD and MASH preparedness index study, in 2023 over 300 experts from around the world, including from across Latin America, agreed on 29 ranked action priorities across six domains: epidemiology, treatment and care, models of care, education and awareness, patient and community perspectives, and leadership and public health policy. The highest-ranking priorities included standardizing and harmonizing data collection and reporting on the disease human and economic burden, collaboration between liver specialists and primary care physicians for early diagnosis, addressing the needs of individuals with multiple morbidities, and incorporating SLD into relevant NCD strategies and guidelines. This, coupled with the global SLD research agenda, forms the first comprehensive roadmap to drive action at local, regional, and global levels [133,134]. One of the top priorities to address the high and growing prevalence of SLD in the Americas is to expand stakeholder involvement in the region [135]. This means moving most of the care and treatment of MASLD and MASH, for example, to primary care and endocrinology, where lifestyle modifications can be prescribed and monitored. Dietitians are envisioned to play a key role in this process and it is crucial that all healthcare providers consider the social and commercial determinants of health when prescribing disease management strategies [136]. To assess the quality of care provided to address SLD, health outcomes and real-world management need to be studied [137].
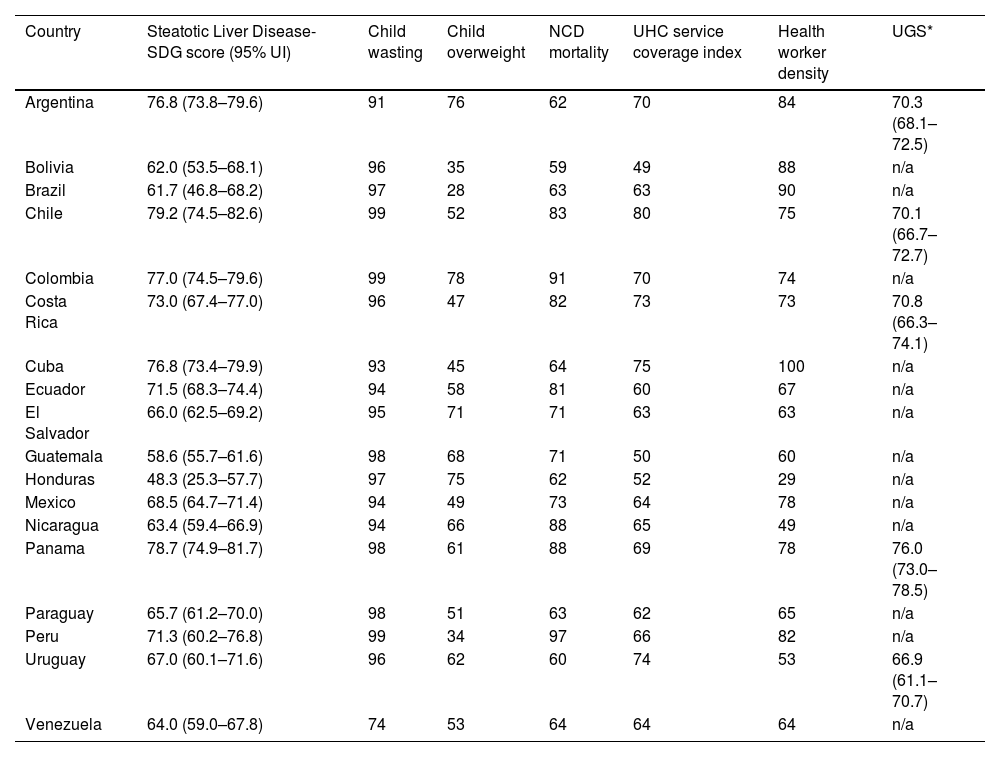
In the absence of a multisectoral framework to tackle SLD, a recent study presented a novel SLD-Sustainable Development Goal (SDG) score for 195 countries and territories, including Latin America, to assess the preparedness for addressing the disease through a whole-of-society approach (Table 3) [138]. This score, which includes several indicators related to health and socioeconomic factors, is a strategic advocacy tool designed to create awareness, advocate for multisectoral collaboration at national and global levels, and guide policymakers, public health experts, and other stakeholders in developing effective disease strategies. By leveraging the insights provided by this score, Latin America, together with the rest of the world, can drive positive change, improve public health outcomes, and contribute to the overall health and well-being of the population.
Steatotic liver disease-SDG scores and indicators for Latin American countries.
| Country | Steatotic Liver Disease-SDG score (95% UI) | Child wasting | Child overweight | NCD mortality | UHC service coverage index | Health worker density | UGS* |
|---|---|---|---|---|---|---|---|
| Argentina | 76.8 (73.8–79.6) | 91 | 76 | 62 | 70 | 84 | 70.3 (68.1–72.5) |
| Bolivia | 62.0 (53.5–68.1) | 96 | 35 | 59 | 49 | 88 | n/a |
| Brazil | 61.7 (46.8–68.2) | 97 | 28 | 63 | 63 | 90 | n/a |
| Chile | 79.2 (74.5–82.6) | 99 | 52 | 83 | 80 | 75 | 70.1 (66.7–72.7) |
| Colombia | 77.0 (74.5–79.6) | 99 | 78 | 91 | 70 | 74 | n/a |
| Costa Rica | 73.0 (67.4–77.0) | 96 | 47 | 82 | 73 | 73 | 70.8 (66.3–74.1) |
| Cuba | 76.8 (73.4–79.9) | 93 | 45 | 64 | 75 | 100 | n/a |
| Ecuador | 71.5 (68.3–74.4) | 94 | 58 | 81 | 60 | 67 | n/a |
| El Salvador | 66.0 (62.5–69.2) | 95 | 71 | 71 | 63 | 63 | n/a |
| Guatemala | 58.6 (55.7–61.6) | 98 | 68 | 71 | 50 | 60 | n/a |
| Honduras | 48.3 (25.3–57.7) | 97 | 75 | 62 | 52 | 29 | n/a |
| Mexico | 68.5 (64.7–71.4) | 94 | 49 | 73 | 64 | 78 | n/a |
| Nicaragua | 63.4 (59.4–66.9) | 94 | 66 | 88 | 65 | 49 | n/a |
| Panama | 78.7 (74.9–81.7) | 98 | 61 | 88 | 69 | 78 | 76.0 (73.0–78.5) |
| Paraguay | 65.7 (61.2–70.0) | 98 | 51 | 63 | 62 | 65 | n/a |
| Peru | 71.3 (60.2–76.8) | 99 | 34 | 97 | 66 | 82 | n/a |
| Uruguay | 67.0 (60.1–71.6) | 96 | 62 | 60 | 74 | 53 | 66.9 (61.1–70.7) |
| Venezuela | 64.0 (59.0–67.8) | 74 | 53 | 64 | 64 | 64 | n/a |
NCD, non-communicable disease; SDG, Sustainable Development Goal; UGS, urban green space; UHC, universal health coverage; UI, uncertainty interval.
Digital health interventions (DHIs) are another type of tool with the potential to help in caring for people with or at risk of liver NCDs. In a study conducted in Spain, 295 physicians were surveyed about their knowledge, beliefs, attitudes, practices, and access regarding DHIs in SLD management [139]. Physicians reported high familiarity with DHIs, but only a minority had received training on their use, and a comparative analysis demonstrated that physicians were more likely to recommend DHIs for patient care if they had received such training. This study concluded that addressing concerns raised by respondents like a lack of evidence of DHI utility and their education, training, and access needs with regard to DHIs may help to increase use of these technologies overall and, more importantly, directly improve patient outcomes.
6Challenges in overcoming liver disease in Latin America and future perspectivesMultiple barriers should be addressed in Latin America to decrease the burden of liver disease, including the proper identification of people at risk of development and progression of CLD, individuals with asymptomatic liver disease, and those at risk for HCC. Due to the vast prevalence of genetic polymorphisms in Latin America, new tools based on genotyping and integration of different variants into polygenic risk scores could be promising techniques to identify subjects at risk of SLD and HCC [140,141]. Simple methods should also be widely adopted to stratify and provide early referral of those with advanced liver fibrosis, including using the Fibrosis-4 index and other inexpensive tools, especially in primary care and in specific populations, such as in patients with T2DM. Early detection of HBV and HCV infections is key to achieve the global goal of eliminating viral hepatitis as a public health threat by 2030. Thus, adults should be screened for HBV and HCV at least once during their lifetime and universal access to antivirals and HBV vaccination must be promoted in the region [142]. HCV and HBV education and prevention programs that include periodic screening should be provided among high-risk populations, especially in men who have sex with men, people living with HIV, and people who inject drugs [83]. Efforts should also focus on the micro-elimination of HCV in specific scenarios [143,144].
It is essential to have public policies to reduce and manage the burden of liver disease and its health consequences in Latin America [22,145]. In the case of ARLD, for instance, establishment of alcohol-related public health policies is heterogeneous in the region [22]. An ecological study including data from 20 Latin American countries demonstrated that having a higher number of public health policies in place was associated with lower mortality due to ARLD, lower AUD prevalence, and lower alcohol-attributable road traffic mortality. In addition, the presence of a national plan on alcohol, driving-related alcohol policies, and restrictions on alcohol access exhibit the highest association with lower ARLD mortality in Latin America [22]. On the other hand, despite the high and rising prevalence of SLD globally, two landmark studies demonstrated that none of the studied countries had specific disease policies [128,146]. Public health policies should also be put in place to promote healthy lifestyles and prevent HCC.
Research on liver disease needs to be undertaken in Latin American countries. In fact, although Latin America is one of the regions with the highest prevalence of MASLD, relevant studies remain scarce, especially on epidemiology and factors like genetics, socioeconomics, lifestyles, and cultural traditions and how these impact the disease [27]. Insufficient opportunities to obtain funding and a clinically oriented medical training, among others, represent significant barriers for implementing high tier research on liver disease in Latin America. Global efforts to act on the established SLD research and action agendas may be helpful in promoting regional studies [133,147]. Creating regional research networks between researchers across Latin America could also generate much-needed data in the field of SLD and other conditions.
7ConclusionsLatin America is a large and heterogeneous region with important disparities in terms of liver disease management. ARLD and MASLD are the leading causes of liver disease, but viral hepatitis still greatly affects some geographic areas and high-risk groups. The epidemiological pattern of MASLD is related to sedentary lifestyles, broad access to ultra-processed food, and a sustained increase in the prevalence of obesity and T2DM. Socioeconomic differences and inequities greatly influence the development of, quality of, and access to screening and treatment programs for liver disease, while the establishment of public health policies on alcohol, MASLD, and other liver conditions and risk factors are lacking throughout Latin America. To grow the liver disease community of practice, wide dissemination of current concepts on liver conditions, including the new SLD nomenclature, which incorporates the novel disease category of MetALD, is needed. Furthermore, extensive collaboration between scientific societies, governments, non-governmental organizations, pharmaceutical and diagnostics industries, and other stakeholders is essential to address a range of liver diseases as public health threats.
Author contributionsL.A.D. and M.A. conceptualized and designed the article. L.A.D., M.V.-R., M.A., and J.V.L. were responsible for data collection, analysis, and interpretation. L.A.D. drafted the article, and all authors critically reviewed its content before approving the submitted version.
This project has received partial funding from the European Union's Horizon 2020 Research and Innovation Programme under grant agreementno. 825510. M.V.-R. and J.V.L. acknowledge support to ISGlobal from the grantCEX2018-000806-S, funded by MCIN/AEI/10.13039/501100011033, and the ‘Generalitat de Catalunya’,through the CERCA Program, outside of the submitted work.





![Trends in age-standardized prevalence of chronic liver disease (including all causes) among the different World Bank regions (1990–2019); data were collected from the Global Burden of Disease database [13]. Trends in age-standardized prevalence of chronic liver disease (including all causes) among the different World Bank regions (1990–2019); data were collected from the Global Burden of Disease database [13].](https://static.elsevier.es/multimedia/16652681/0000002900000003/v1_202404281202/S1665268123002788/v1_202404281202/en/main.assets/thumbnail/gr1.jpeg?xkr=ue/ImdikoIMrsJoerZ+w96p5LBcBpyJTqfwgorxm+Ow=)
![Trends in age-standardized incidence of primary liver cancer among the different World Bank regions (1990–2019); data were collected from the Global Burden of Disease database [13]. Trends in age-standardized incidence of primary liver cancer among the different World Bank regions (1990–2019); data were collected from the Global Burden of Disease database [13].](https://static.elsevier.es/multimedia/16652681/0000002900000003/v1_202404281202/S1665268123002788/v1_202404281202/en/main.assets/thumbnail/gr2.jpeg?xkr=ue/ImdikoIMrsJoerZ+w96p5LBcBpyJTqfwgorxm+Ow=)




