Heart surgery is one of the most important tools for the treatment of cardiovascular diseases. Postoperative pulmonary complications in patients undergoing heart surgery represent a meaningful clinical problem.
Respiratory physiotherapy is essential in the management of patients during postoperative period, contributing to a better prognosis.
Our objective is to evaluate the efficacy of respiratory physiotherapy prior to cardiac surgery in reducing postoperative complications and hospital stay.
MethodsRandomized, controlled and observational study. A group of 92 patients who underwent heart surgery with extracorporeal circulation were analyzed in the Hospital Puerta del Mar (Spain), divided into 2 groups (control group and experimental group with previous respiratory physiotherapy). We study different postoperative complications and hospital stay.
ResultsAtelectasis, pleural effusion, and sternal dehiscence were altered between both groups. An improvement in the intubation time and the reintubation rate was reported in the experimental group, in addition, lower oxygen consumption, an improvement in the fulfillment of respiratory physiotherapy following surgery and a shorter overall hospital stay and in the post-operative care unit was also observed.
ConclusionFulfillment of respiratory physiotherapy preceding to heart surgery decreases pulmonary complications and hospital stay, as well as accelerates the recovery of the breathing capacity.
La cirugía cardiaca es una de las herramientas más importantes para el tratamiento de las enfermedades cardiovasculares. Las complicaciones pulmonares posoperatorias en pacientes sometidos a cirugía cardiaca representan un problema clínico significativo.
La fisioterapia respiratoria es esencial en el manejo de los pacientes durante el posoperatorio, contribuyendo a un mejor pronóstico.
Nuestro objetivo es evaluar la eficacia de la fisioterapia respiratoria previa a la cirugía cardiaca en la reducción de las complicaciones posoperatorias y la estancia hospitalaria.
MétodosEstudio aleatorizado, controlado y observacional. Se analizó un grupo de 92 pacientes sometidos a cirugía cardiaca con circulación extracorpórea en el Hospital Puerta del Mar (España), divididos en dos grupos (grupo control y experimental con fisioterapia respiratoria previa). Estudiamos diferentes complicaciones posoperatorias y estancia hospitalaria.
ResultadosLa atelectasia, el derrame pleural y la dehiscencia esternal se alteraron entre ambos grupos. Se observó una mejora en el tiempo de intubación y en la tasa de reintubación en el grupo experimental, además de un menor consumo de oxígeno, una mejora en el cumplimiento de la fisioterapia respiratoria tras la cirugía y una estancia hospitalaria global y en la unidad de cuidados posoperatorios más corta.
ConclusiónEl cumplimiento de la fisioterapia respiratoria previa a la cirugía cardiaca disminuye las complicaciones pulmonares y la estancia hospitalaria, asimismo, acelera la recuperación de la capacidad respiratoria.
Cardiovascular diseases are a group of disorders of the heart and blood vessels, and they are the main cause of death and disability all over the world.1 According to the 2017 World Health Organization (WHO) report, 17.7 million people died in 2015 due to this cause, which represents a 31% of all deaths.2 In many cases, treatments with different medicines or even surgical interventions such as coronary shunts or valvular substitutions are necessary to obtain a secondary prevention of cardiovascular diseases in patients with a final diagnosis.2 Heart surgery is one of the most important tools for the treatment of cardiovascular diseases.1,3
Postoperative pulmonary complications in patients undergoing heart surgery with cardiopulmonary bypass represent a significant clinical problem with a negative impact over morbidity, mortality, hospital stay and the cost for health care with an incidence that can vary from 5% to 90%, depending on how complications are defined.1,4–10
Respiratory physiotherapy is essential in the management of the patients in the postoperative contributing to a better prognosis.4 Respiratory physiotherapy in the early postoperative period after coronary artery bypass grafting has been widely used to reverse or minimize postoperative pulmonary complications.11 Different studies have proved the effectiveness of the inspiratory muscle training (IMT) in the restoration of ventilation, reduction in the duration of hospital stay, the improvement of functional capacity and the quality of life of patients who underwent into a coronary artery bypass grafting (CABG) during the first phases of cardiac rehabilitation.1
Respiratory physiotherapy performed prior to heart surgery can produce improvements in tidal volume, enforced vital capacity, the forced expiratory volume in the first second, the maximum inspiratory and expiratory pressure and, thereby, a decrease in the incidence of atelectasis and in the clinical stay. However, other studies have not proved that these spirometry parameters produce differences in both inspiratory and expiratory muscle strength. Even so, respiratory physiotherapy seems to play an important role in the preoperative and postoperative period in patients undergoing to a heart surgery.4,7,12
Although the preoperative training of the inspiratory muscle can reduce the risk of developing postoperative pulmonary complications such as pneumonia and atelectasis after the CABG and the valvular surgery, are necessary some tests that provide evidence for routine preoperative implementation of this type of training.8
MethodsStudy and participantsThis study is randomized, controlled and observational. The type of randomization is simple.
The data were collected from 92 patients who underwent cardiac surgery with extracorporeal circulation in influence area in Hospital Universitario Puerta del Mar (Cádiz, Spain) since from August 17th to February 13th, 2021.
The inclusion and exclusion criteria were:
- •
Criteria of inclusion: patient who enters in surgery waiting list and is going to be undergoing to heart surgery with extracorporeal circulation.
- •
Criteria of exclusion: emergency/urgency surgery patients; patients in waiting list who are to undergo aortic valve replacement by TAVI technique; patients intervened by partial sternotomy or thoracotomy; patients intervened previously of heart surgery (reoperations). Patients who have been less than 30 days in waiting list until the moment of the procedure; patients who have been more than 3 months in waiting list; patients who during the postoperative are reintervened due to a complication other than respiratory; patients diagnosed with Covid-19.
In the preoperative consult are explained the exercises for the thoracic expansion with spirometer and it is indicated a frequency of around 3–7 times per day during at least 30 days. The exercises consist of taking deep breaths with the Tri-Ball® spirometer as visual incentive in seated position and standing with a brief apnea at the end, followed by a slow passive exhalation. It is tested that the patient understands and makes the exercises adequately.
SurgeryValve replacements (aortic, mitral, tricuspid), valvuloplasty, surgical myocardial revascularization surgeries, aortic surgeries, resection of cardiac tumors and adult congenital heart diseases. In all cases with extracorporeal circulation and cardiac arrest.
Outcome measures- •
Preoperative variables
The preoperative variables considered were: age (expressed in years), sex (woman, man), left ventricular ejection fraction (LVEF; percentage calculated by transthoracic echocardiography via Simpson's method for volume calculation), arterial hypertension (systolic blood pressure≥140mm Hg and/or numbers of diastolic pressure≥90mm Hg), diabetes mellitus (blood glucose≥200mg/dL), dyslipidemia (plasma total cholesterol≥200mg/dL and/or numbers of plasma triglycerides≥200mg/dL), smoking (defined by WHO as smoker, non-smoker and ex-smoker), alcoholism according to the survey of AUDIT-C (Alcohol Use Disorders Identification Test-consumption questions) cut-off point of 5 to man and 4 to woman, body-mass index (BMI), asthma, sleep apnea–hypopnea syndrome (SAHS), and chronic obstructive pulmonary disease (COPD) according to diagnosis before hospitalize.
- •
Perioperative variables
The perioperative variables considered were the type of intervention (valvular, coronary, valvular+coronary and other kind of surgery with extracorporeal circulation (ECC)), time of ECC and time of ischemia (in minutes), kind of close (sternal cerclage wires, sternal cerclage wires and Nitinol staples, cerclage with wires, bridles and osteosynthesis with patches and screws), time of intubation (in hours) and reopening due to bleeding.
- •
Postoperative variables
Postoperative variables were: sternal dehiscence (diagnosed by clinical examination supported by thorax radiography and computed axial tomography (CAT) of the thorax), infection of the wound, pleural effusion and atelectasis (according to clinical and imaging criteria), sepsis (diagnosed with the scoring of 2 or more points in SOFA scale, Sequential [Sepsis-Related] Organ Failure Assessment), breathing infection (clinical, microbiologic and radiologic criteria), progress in results with the Tri-Ball® spirometer and the additional O2 through nasal cannula during the days of hospitalization in ward (liters). The spirometer progress was studied as the fraction of air displaced by the patient in relation to that displaced before surgery. The day before surgery the volume of air displaced by the patient was measured and registered. These variables were always measured at 15:00h (double-blind).
Variables related to hospitalization periods (post-operative care unit, hospitalization on the ward and total hospitalization) are measured in days. Mortality was also quantified.
Data analysisAll the data were taken in an anonymized way and by expert personnel not directly involved in the investigation (double-blind). The statistical program IBM SPSS Statistics (IBM Corps, vs. 28.0.0) was used to perform the statistical analysis.
- •
Descriptive statistics
To determine the population average was used the interval estimation. The confidence interval used was 95% and to calculate the confidence limits of the average are used the standard error of the average and the principles of the normal distribution. For dispersion measures was used the standard error. Qualitative variables are presented as percentages (IC 95%). Qualitative variables are presented by a bar chart or sectorial diagram, as appropriate. Bar chart is used for discrete quantitative variables and the histogram for continuous variables.
- •
Inferential statistics
Level of significance considered will be p<0.05 (IC 95%).
For qualitative variables are made the contingency tables, using the Chi-squared and Fisher's tests.
For quantitative variables is made a previous analysis of normality, using the principal laws of distribution of randomize variables. Considering the estimated sample size, it will be used in this study the Kolmogorov–Smirnov test. If the independent variable is qualitative dichotomous will be used the T of Student and the U of Mann–Whitney, based on whether the dependent variable meets normality conditions or not.
ResultsThe sample of this study had a total of 92 patients, with an age average of 63.4±1.04 years of which the 71.7% were men and the 28.3% women. As for the cardiovascular risk factors, the 63% presented AHT, the 33.7% DM, the 50% dyslipidemia, the 22.8% history of active smoking and the 29.3% were ex-smokers. The 15.2% of the sample presented oenolism as history. Another medical history of interest: the 7.6% had the diagnosis of asthma, the 6.5% chronic obstructive pulmonary disease and the 7.6% obstructive sleep apnea–hypopnea syndrome. The BMI average of 28.98±0.46 and a left ventricular ejection fraction of 56.83±1.25%.
Out of the total sample, the 46.7% of the patients underwent a valvular surgery, the 37% a surgical myocardial revascularization surgery, the 7.6% a valvular surgery+coronary surgery and the 8.7% a surgery for another reason, all of them with an extracorporeal circulation in the procedure. The average of ischemia time was 70.14±2.91min and ECC of 86.56±3.75min. In 77.2% of the patients were used wires for the sternal cerclage, in the 16.3% wires and staples and wires and bridles in the 5.4%. After the immediate postoperative, the complications observed were: plural effusion in the 48.9% of the sample, the 29.3% of the sample was diagnosed of atelectasis, the 13% of the patients with breathing infection and the 5.4% with sternal dehiscence.
Patients were intubated an average of 12.17±1.46h, a 7.6% of the patients needed reintubation and had a stay average in the post-operative care unit of 3.93±0.33 days. The average hospitalization period in ward was 9.15±1.25 days. The total hospitalization period was 12.99±1.35 days and the 1.1% of patients died.
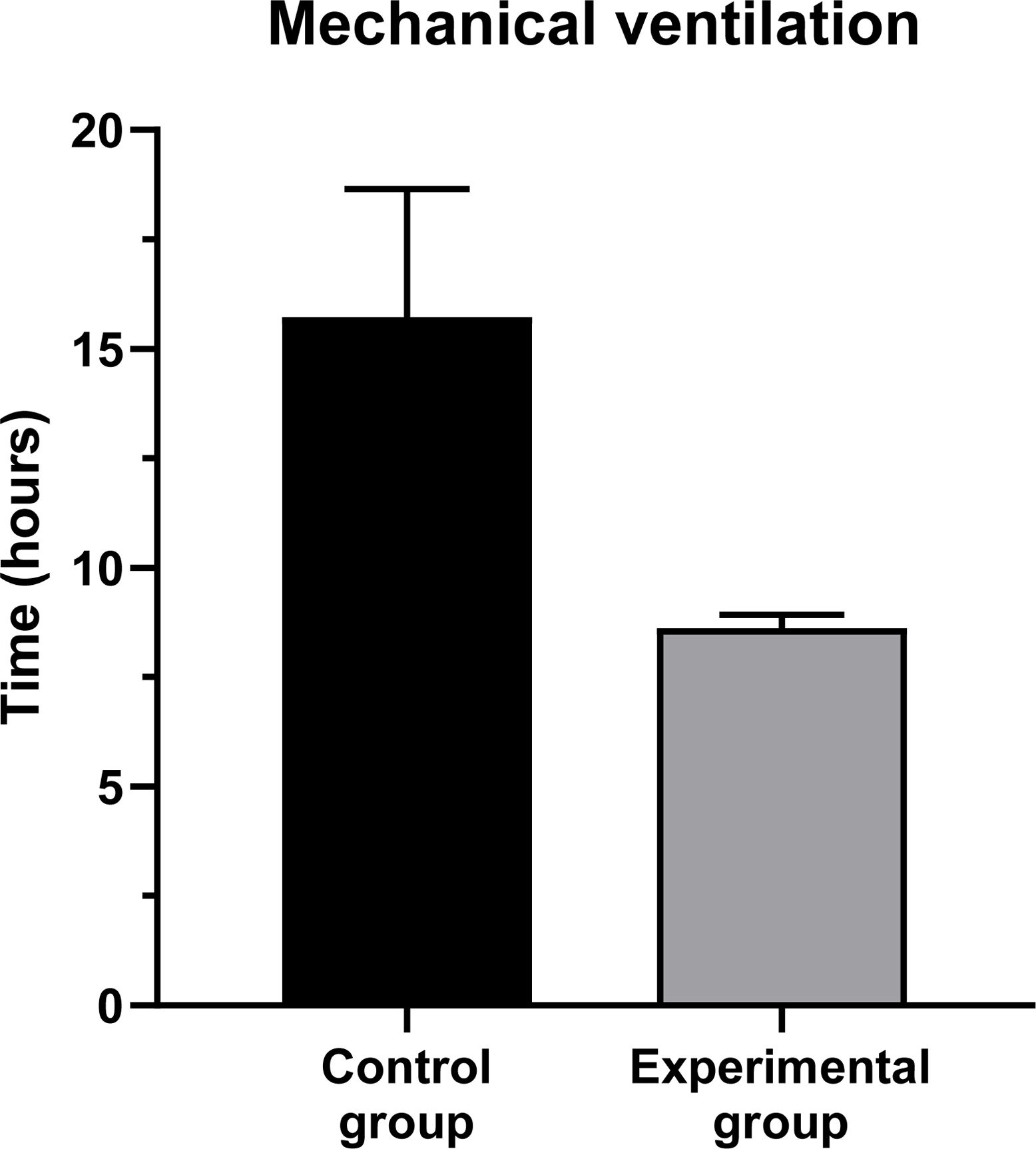
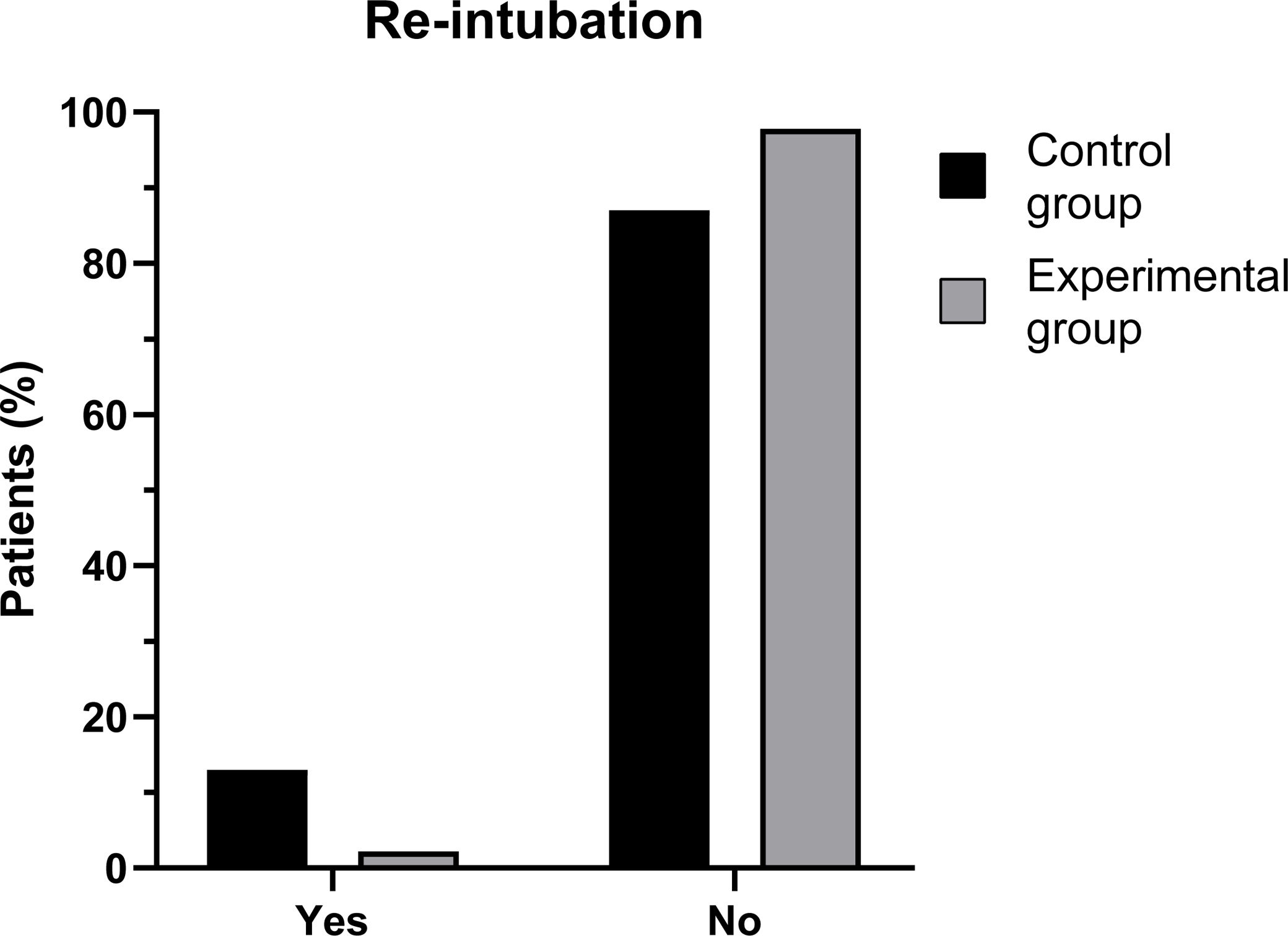
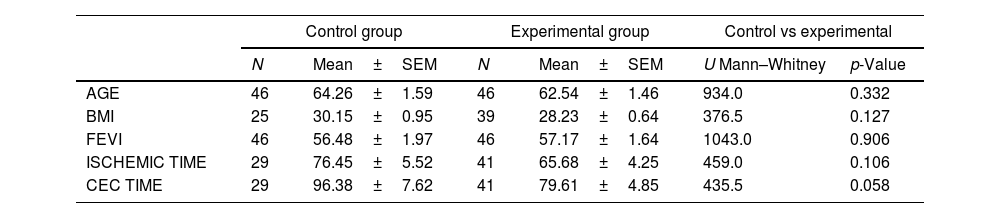
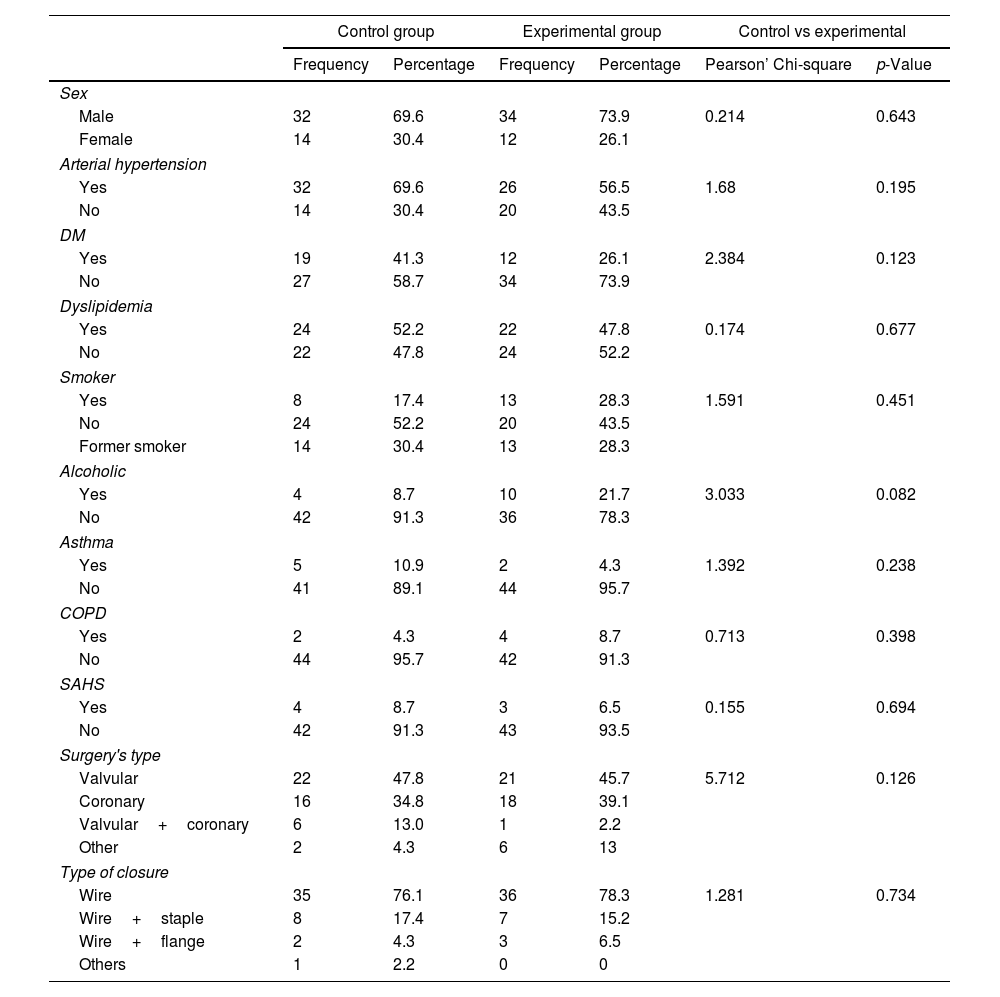
Studying the qualitative and quantitative preoperative variables no statistically significant differences were found between the control and the experimental groups. Neither were found differences in the perioperative variables with exception of intubation time (15.73±2.92h vs 8.62±0.30; p<0.001; Fig. 1) and the need of reintubation (13% vs 2.2%; p=0.049; Fig. 2). Tables 1 and 2 show all the data of the variables measured according to their experimental group whose comparisons were not statistically significant.
Mean±standard error of quantitative variables by experimental group.
| Control group | Experimental group | Control vs experimental | ||||
|---|---|---|---|---|---|---|
| N | Mean±SEM | N | Mean±SEM | U Mann–Whitney | p-Value | |
| AGE | 46 | 64.26±1.59 | 46 | 62.54±1.46 | 934.0 | 0.332 |
| BMI | 25 | 30.15±0.95 | 39 | 28.23±0.64 | 376.5 | 0.127 |
| FEVI | 46 | 56.48±1.97 | 46 | 57.17±1.64 | 1043.0 | 0.906 |
| ISCHEMIC TIME | 29 | 76.45±5.52 | 41 | 65.68±4.25 | 459.0 | 0.106 |
| CEC TIME | 29 | 96.38±7.62 | 41 | 79.61±4.85 | 435.5 | 0.058 |
BMI: body mass index; FEV1: forced expiratory volume; CEC time: Cardiopulmonary Bypass (CPB) with Extracorporeal Circulation time.
Mean±standard error of qualitative variables by experimental group.
| Control group | Experimental group | Control vs experimental | ||||
|---|---|---|---|---|---|---|
| Frequency | Percentage | Frequency | Percentage | Pearson’ Chi-square | p-Value | |
| Sex | ||||||
| Male | 32 | 69.6 | 34 | 73.9 | 0.214 | 0.643 |
| Female | 14 | 30.4 | 12 | 26.1 | ||
| Arterial hypertension | ||||||
| Yes | 32 | 69.6 | 26 | 56.5 | 1.68 | 0.195 |
| No | 14 | 30.4 | 20 | 43.5 | ||
| DM | ||||||
| Yes | 19 | 41.3 | 12 | 26.1 | 2.384 | 0.123 |
| No | 27 | 58.7 | 34 | 73.9 | ||
| Dyslipidemia | ||||||
| Yes | 24 | 52.2 | 22 | 47.8 | 0.174 | 0.677 |
| No | 22 | 47.8 | 24 | 52.2 | ||
| Smoker | ||||||
| Yes | 8 | 17.4 | 13 | 28.3 | 1.591 | 0.451 |
| No | 24 | 52.2 | 20 | 43.5 | ||
| Former smoker | 14 | 30.4 | 13 | 28.3 | ||
| Alcoholic | ||||||
| Yes | 4 | 8.7 | 10 | 21.7 | 3.033 | 0.082 |
| No | 42 | 91.3 | 36 | 78.3 | ||
| Asthma | ||||||
| Yes | 5 | 10.9 | 2 | 4.3 | 1.392 | 0.238 |
| No | 41 | 89.1 | 44 | 95.7 | ||
| COPD | ||||||
| Yes | 2 | 4.3 | 4 | 8.7 | 0.713 | 0.398 |
| No | 44 | 95.7 | 42 | 91.3 | ||
| SAHS | ||||||
| Yes | 4 | 8.7 | 3 | 6.5 | 0.155 | 0.694 |
| No | 42 | 91.3 | 43 | 93.5 | ||
| Surgery's type | ||||||
| Valvular | 22 | 47.8 | 21 | 45.7 | 5.712 | 0.126 |
| Coronary | 16 | 34.8 | 18 | 39.1 | ||
| Valvular+coronary | 6 | 13.0 | 1 | 2.2 | ||
| Other | 2 | 4.3 | 6 | 13 | ||
| Type of closure | ||||||
| Wire | 35 | 76.1 | 36 | 78.3 | 1.281 | 0.734 |
| Wire+staple | 8 | 17.4 | 7 | 15.2 | ||
| Wire+flange | 2 | 4.3 | 3 | 6.5 | ||
| Others | 1 | 2.2 | 0 | 0 | ||
DM: diabetes mellitus; COPD: chronic obstructive pulmonary disease; SAHS: sleep apnea–hypopnea syndrome.
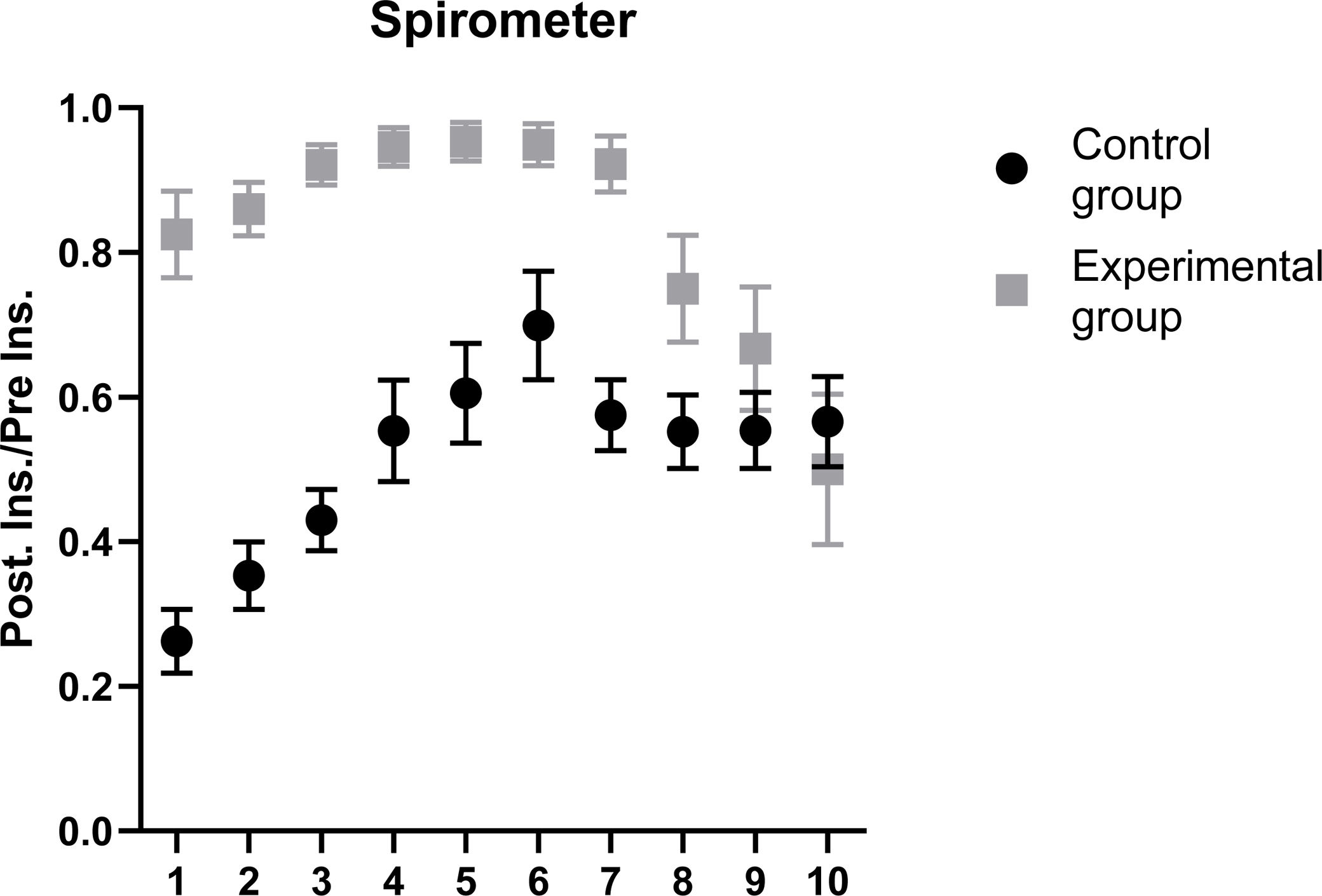
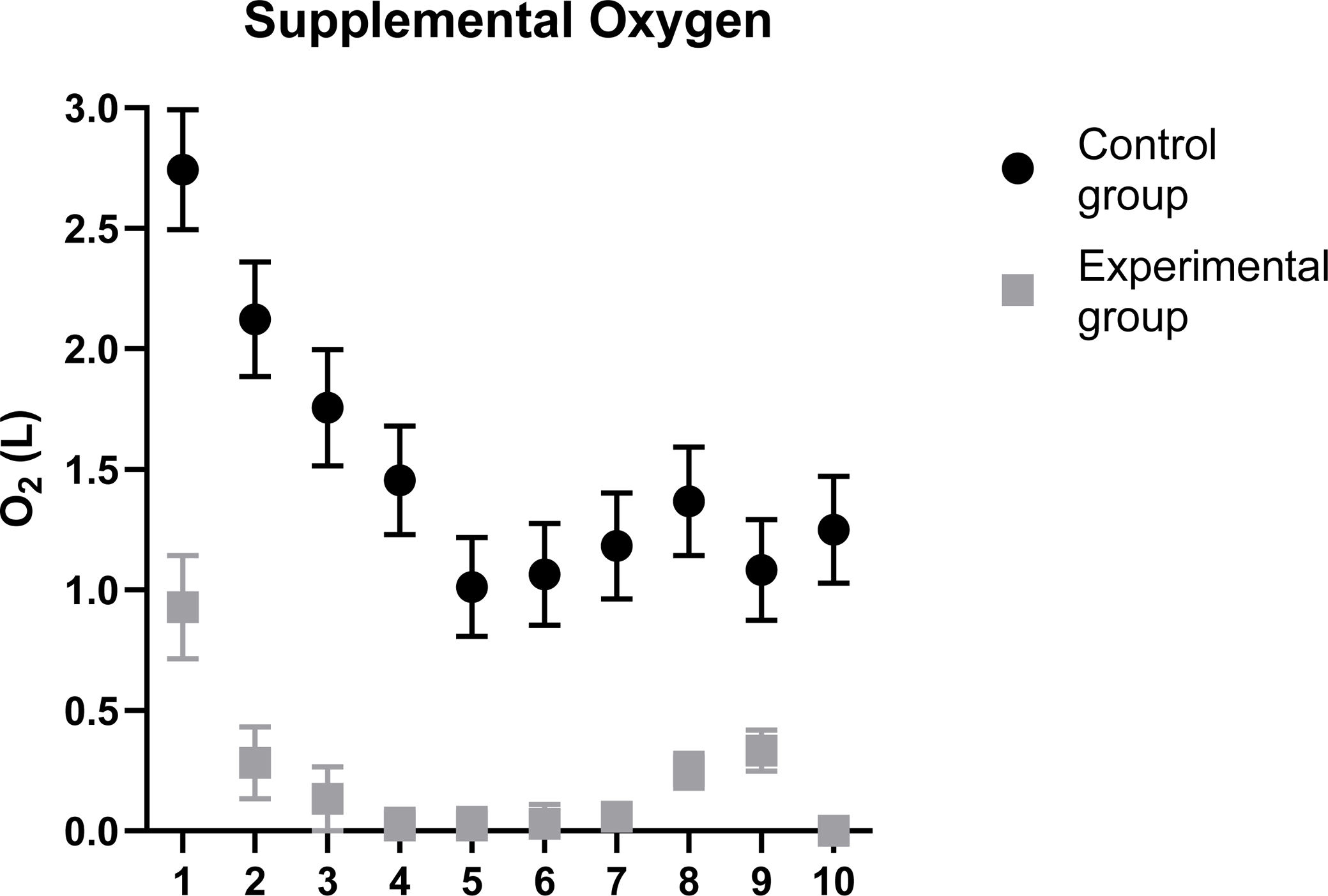
When comparing the progression with the spirometer of patients in ward, we found statistically significant results in the experimental group during the first 7 days of hospitalization in ward (Fig. 3). We also found differences statistically significant in the need of additional oxygen for the experimental group during the first 7 days of hospitalization in ward (Fig. 4), being both results better in the experimental group.
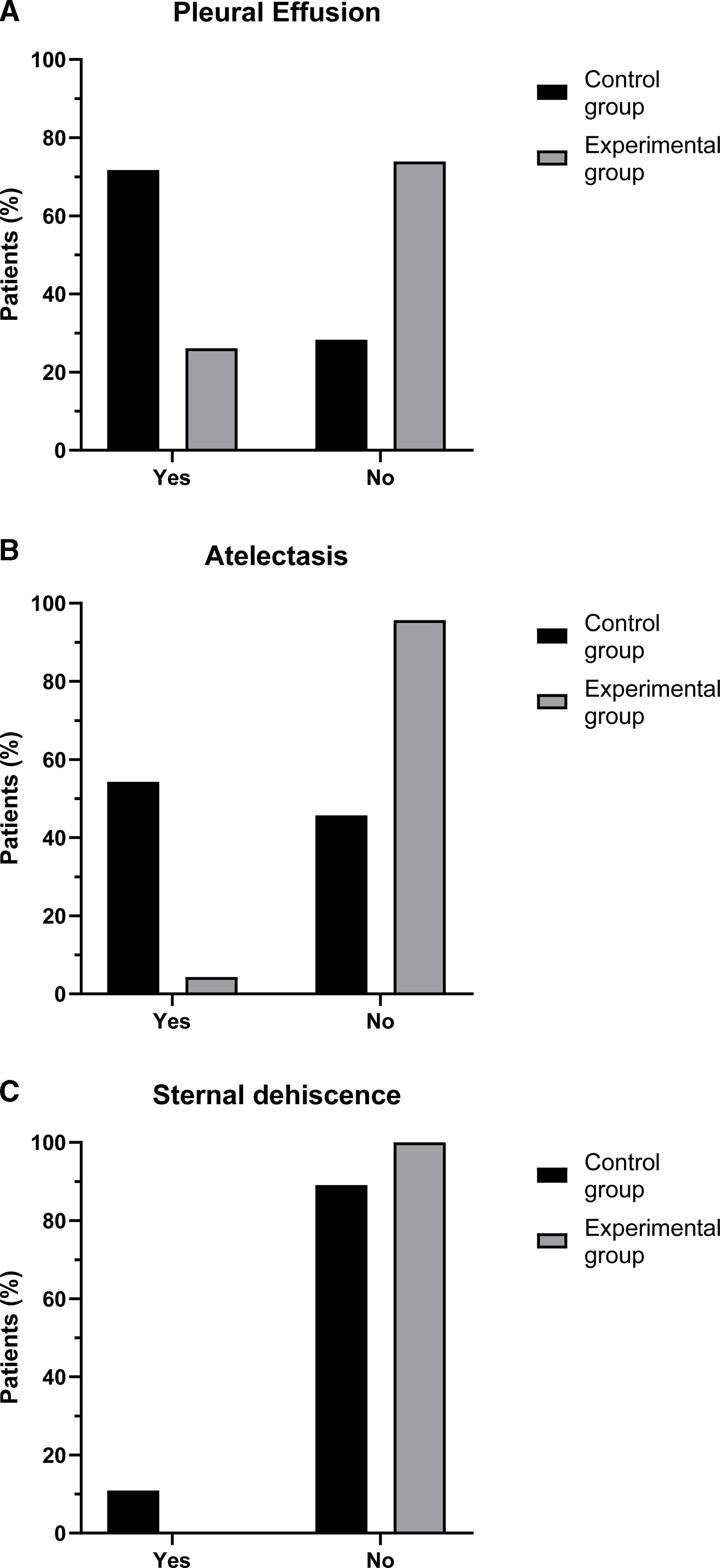
Analyzing the postoperative complications, a lower percentage of pleural effusion in the experimental group (26.1% vs 71.7%; p<0.001; Fig. 5A) and a lower percentage of atelectasis (4.3% vs 54.3%; p<0.001; Fig. 5B) was observed.
Other postoperative complication analyzed was the sternal dehiscence, finding a lower percentage in the experimental group being statistically significant (0% vs 10.9%; p=0.021; Fig. 5C). No statistically significant differences were found between groups when studying postoperative complications of breathing infection and sepsis.
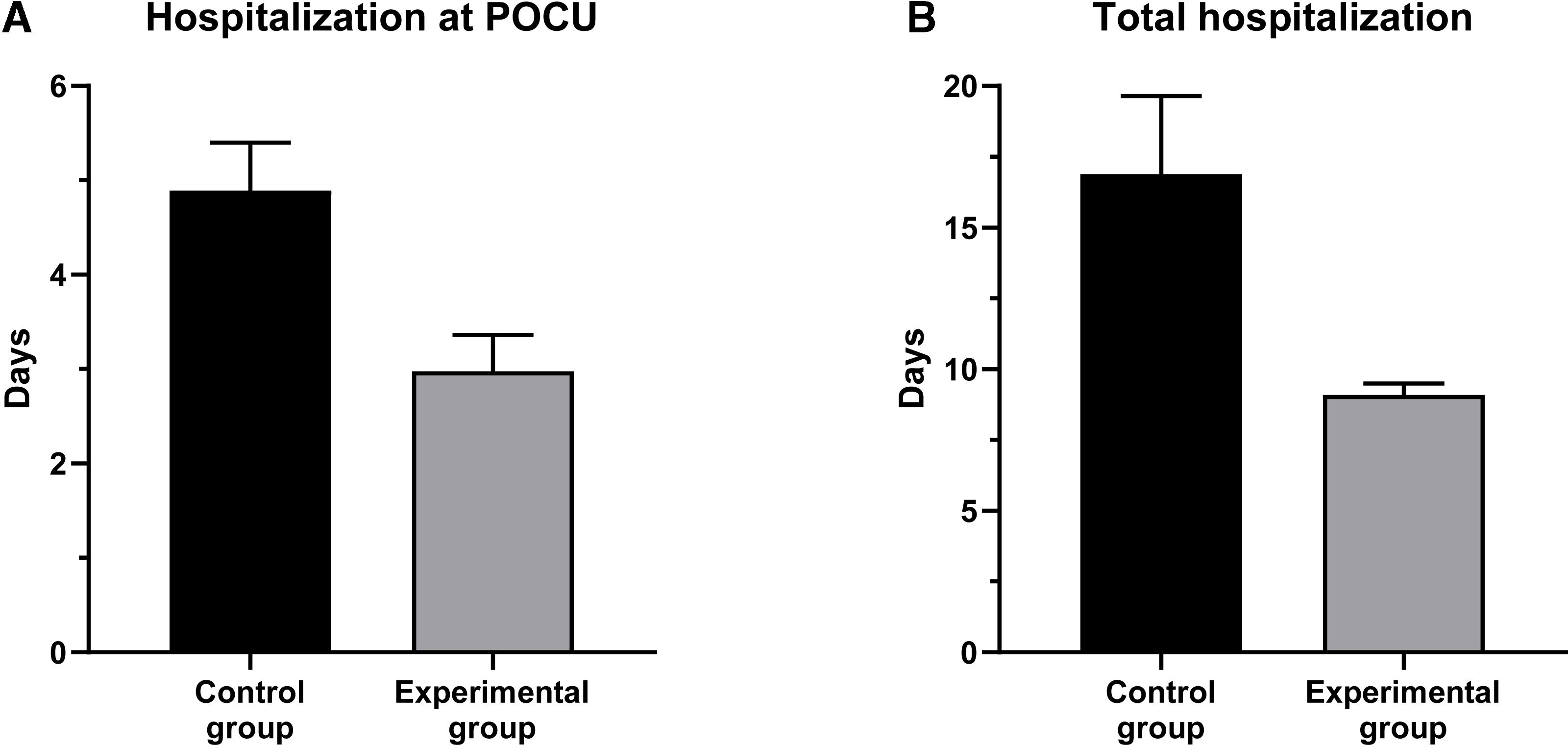
When studying the hospital stay, we find a lower hospitalization period in the post-operative care unit in the experimental group (2.98±0.38 vs 4.89±0.5; p<0.001; Fig. 6A). The hospitalization period in ward did not show any differences, but there were differences in the overall hospitalization period in favor of the experimental group (9.09±0.41 vs 16.89±2.76; p<0.001) that was lower (Fig. 6B).
DiscussionIn this paper we demonstrate that respiratory physiotherapy consisting of thoracic expansion exercises with a spirometer performed at a frequency of 3–7 times a day during 1–3 months (see material details and methods) reduces intubation time and the possibility of reintubation and reduces the quantity of needed oxygen in the postoperative period. Furthermore, this approach has been shown to result in shorter hospitalizations and post-operative care unit stay time, also reducing the possibilities of postoperative complications like atelectasis, pleural effusion, and sternal dehiscence.
Other studies have analyzed the effect of respiratory physiotherapy before surgery, finding that there are no differences in the time of mechanical ventilation.12 Nevertheless, these studies were conducted with a smaller number of patients and focused on CABG. Our data support the hypothesis developed by Herdy et al. that, with a smaller sample size and focusing on CABG, they founded a decrease of mechanical ventilation time in the group of patients that had received physiotherapy during at least 5 days before the surgery.13
Our results demonstrate that the inspiratory muscle training provides a decrease in the intubation time and in the possibility of reintubation, as in the meta-analysis conducted by Snowdon.14
Regarding the perioperative complications, it has been highly argued about the efficacy of this preoperative respiratory physiotherapy on its decrease. Thus, deep breathing exercises seem to reduce atelectasis,15 whereas respiratory physiotherapy, at least 5 days before surgery, decreases atelectasis as well as the incidence of pneumonias and atrial fibrillations.13 The explanation of this reduction in the most important pulmonary complications would be due to the improvement of resistance and strength of the respiratory muscles with the inspiratory muscle training.15 The preoperative training of inspiratory musculature seems to reduce the postoperative pulmonary complications7,8 although still some papers argues the contrary.16 These differences could be due to the small sample size, of those studies, which could be the most relevant limitation of studies with contrary results to those presented herein. In addition, we have found a decrease in the incidence of pleural effusion, atelectasis, and sternal dehiscence in the intervention group with a use of spirometer for 7 days, what endorses and strengthens the evidence that support the need of routinely implementing this procedure in conical practice.
Following our protocol, preoperative respiratory physiotherapy not only decreases postoperative complications, but also decreases the need of additional oxygen in the 7 days following surgery. This may be due to the improvement of the maximum inspiratory pressure and the maximum expiratory pressure to the fifth postoperative day and due to an increase of the volume minutes before surgery.12
As well as improving the maximum expiratory pressure, the respiratory physiotherapy, and the mobilization of members in the preoperative period, it improves the arterial oxygen saturation16 and the forced expiratory volume in the first minute in the postoperative period and forced vital capacity.7
Finally, our study is consistent with other studies that have shown that preoperative respiratory physiotherapy reduces the hospitalization period.12,15 However, unlike what happens in Teixeira's work or in the reviewed by Osman,8 our protocol produces an improvement in the hospitalization period in the post-operative care unit. The quality of our results in total hospitalization period or in the hospitalization period in the post-operative care unit are due exclusively to the breathing exercises carried out before surgery. Not as in Nardi's work16 in which they only achieved the improvement with the combination of the respiratory physiotherapy and the mobilization of members.
ConclusionsSupported by the results described above and the large number of patients used in our study (sample size larger than the rest of previous literature analyzed in the present study), we can propose that our 30–90 days protocol performing thoracic expansion exercises with spirometer 3/7 times per day previous the heart surgery decreases the preoperative complications, reduces the hospitalization period, improving, thus, the recovery of the patient and, secondarily, reducing the necessary health expenditure in these kind of interventions.
Ethics approval and consent to participateThis study was conducted in accordance with the Declaration of Helsinki and with the Data Protection Regulation (EU) 2016/679 of the European Parliament. Ethical approval for this study was granted by the Ethics Committee on Drug Research of Cádiz (Spain).
Data availabilityThe data that support the findings of this study are available from the corresponding author upon reasonable request.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestsThe authors declare no competing interests.
The authors are grateful to the participating patients and their families.