Aortic valve replacement has been performed conventionally by full sternotomy. Ministernotomy emerged as an alternative approach, and although it has achieved excellent results in high-volume centers, evidence remains limited in low-volume hospitals. This study aimed to evaluate the outcomes of full sternotomy versus mini-J sternotomy as access route in aortic valve replacement in a low-volume center.
MethodsPatients’ data who underwent aortic valve replacement by full sternotomy or mini-J sternotomy at the Cardiac Surgery Department of San Juan de Dios Hospital from 2010 to 2015 was analyzed and obtained from medical records and clinical databases.
ResultsA total of 141 patients who underwent aortic valve replacement were included, 84 were operated by ministernotomy and 57 by full sternotomy. No differences were found in baseline characteristics and males predominated in both groups. Thirty-day mortality was higher in the full sternotomy group (16.4% vs 3.6%, p=0.013), and overall deaths, were higher in female patients (58.3% vs 41.7%, p=0.040). Ministernotomy patients’ post-surgical survival was higher in the first (log-rank p=0.0096) and second months (log-rank p=0.046). Cox regression analysis revealed ministernotomy as an independent protective predictor in short (HR:0.157, 95% CI:0.040–0.619) and mid-term mortality (HR:0.302, 95% CI:0.103–0.884).
ConclusionIn this study, ministernotomy demonstrated to be a feasible and safe technique in aortic valve replacement, with outcomes compared to the standard approach and a greater short-term survival and lower 30-day mortality.
El reemplazo valvular aórtico se ha realizado convencionalmente mediante esternotomía media. La miniesternotomía surgió como alternativa, y aunque ha logrado excelentes resultados en centros de alto volumen, la evidencia sigue siendo limitada en hospitales de bajo volumen. Este estudio tuvo como objetivo evaluar los resultados de esternotomía media en comparación con miniesternotomía en J en un centro de bajo volumen.
MétodosSe analizaron los datos de pacientes sometidos a reemplazo valvular aórtico mediante esternotomía media o miniesternotomía en J en el Departamento de Cirugía Cardiaca del Hospital San Juan de Dios entre 2010 y 2015. La información se obtuvo de registros médicos y bases de datos clínicas.
ResultadosSe incluyeron 141 pacientes; 84 operados mediante miniesternotomía y 57 por esternotomía media. No se encontraron diferencias en características basales, y hubo predominancia masculina. La mortalidad a los 30 días fue mayor en el grupo de esternotomía media (16.4% vs 3.6%, p=0.013), y en el sexo femenino (58.3% vs 41.7%, p=0.040). La supervivencia postquirúrgica fue mayor en el grupo de miniesternotomía en el primer (log-rank p=0.0096) y segundo mes (log-rank p=0.046). La regresión de Cox indicó que la miniesternotomía es un predictor protector en mortalidad a corto (HR:0.157, IC del 95%:0.040–0.619) y mediano plazo (HR:0.302, IC del 95%:0.103–0.884).
ConclusiónEn este estudio, la miniesternotomía demostró ser una técnica factible y segura en el reemplazo valvular aórtico, con resultados comparables al abordaje estándar y mayor supervivencia a corto plazo, así como menor mortalidad a los 30 días.
Worldwide, aortic valve replacement (AVR) is one of the most common cardiac surgical procedures.1,2 Historically, full sternotomy (FS) has been the standard approach for AVR.3,4 However, since the mid-1990s, minimally invasive surgery emerged, aiming to reduce procedure invasiveness without compromising, safety and results of the standard approach.5 Currently, the “J” or inverted “L” ministernotomy (MS) are the most used techniques for minimally invasive aortic valve replacement (MIAVR).4 Although several studies have reported advantages associated with MS such as reduced intraoperative blood loss, surgical trauma, and shorter intensive care units (ICU) and hospital stay6,7; it remains unclear whether there are differences between conventional and minimal access surgery; since the results may be influenced by biases and methodological limitations of the different studies.8
Although some high-volume centers have demonstrated excellent outcomes with MIAVR,9,10 where the improvement of surgical techniques leads to an efficiency and safety at least equivalent to conventional surgery9; evidence in low-volume centers remains limited. The aim of this study was to evaluate outcomes of full sternotomy versus mini-J sternotomy as access route in AVR at a low-volume center.
Patients and methodsThis retrospective observational study was conducted at the Cardiac Surgery Department of San Juan de Dios Hospital in Costa Rica, with data between January 2010 and December 2015. Patients older than 13 years who underwent elective AVR sole procedure, using either full sternotomy or ministernotomy were included. History of previous cardiac surgery or major surgery in the last 3 months, combined or emergency surgery or life expectancy lesser than 3 months were considered exclusion criteria. Data was obtained from medical records and clinical databases.
Ethics statementStudy was conducted in accordance with Helsinki's Declaration Principles, ethical standards and was approved by San Juan de Dios Hospital (HSJD-04-2022) Scientific Ethics Committee. A waiver for obtaining written consent was granted.
Statistical analysisStudy population was divided into two groups according to the access route, and it was age stratified for some determinations. Statistical analysis was performed using SPSS Statistics for Windows (version 24, IBM Corporation, Armonk, NY, USA). Continuous variables were described as medians and interquartile ranges (IQR), while categorical variables as frequencies and percentages. Quantitative variables were compared using the Mann–Whitney U test, while possible associations were analyzed using the Chi-square or Fisher's exact tests. Analyses were carried out using the intention-to-treat principle.
Follow-up was reported as short-term (one/two months), mid-term (six months) and long-term (sixty months). Kaplan–Meier survival curves were used to determine short- and mid-term survival, and differences were evaluated using the log-rank test. The influence of the surgical approach on short, mid and long-term survival was assessed using the Cox proportional hazards model in the total population; missing data was imputed as medians and possible covariates were based on literature. Significant covariates (p<0.05) in the univariable analysis and surgical approach (forced in the model, independent of p-value) were included in a multivariable Cox regression analysis. Hazard ratios (HR) are reported with 95% confidence intervals (CI). Used model was evaluated using a goodness-of-fit test, in which a p-value of <0.05 demonstrated violation of proportional hazards assumption.
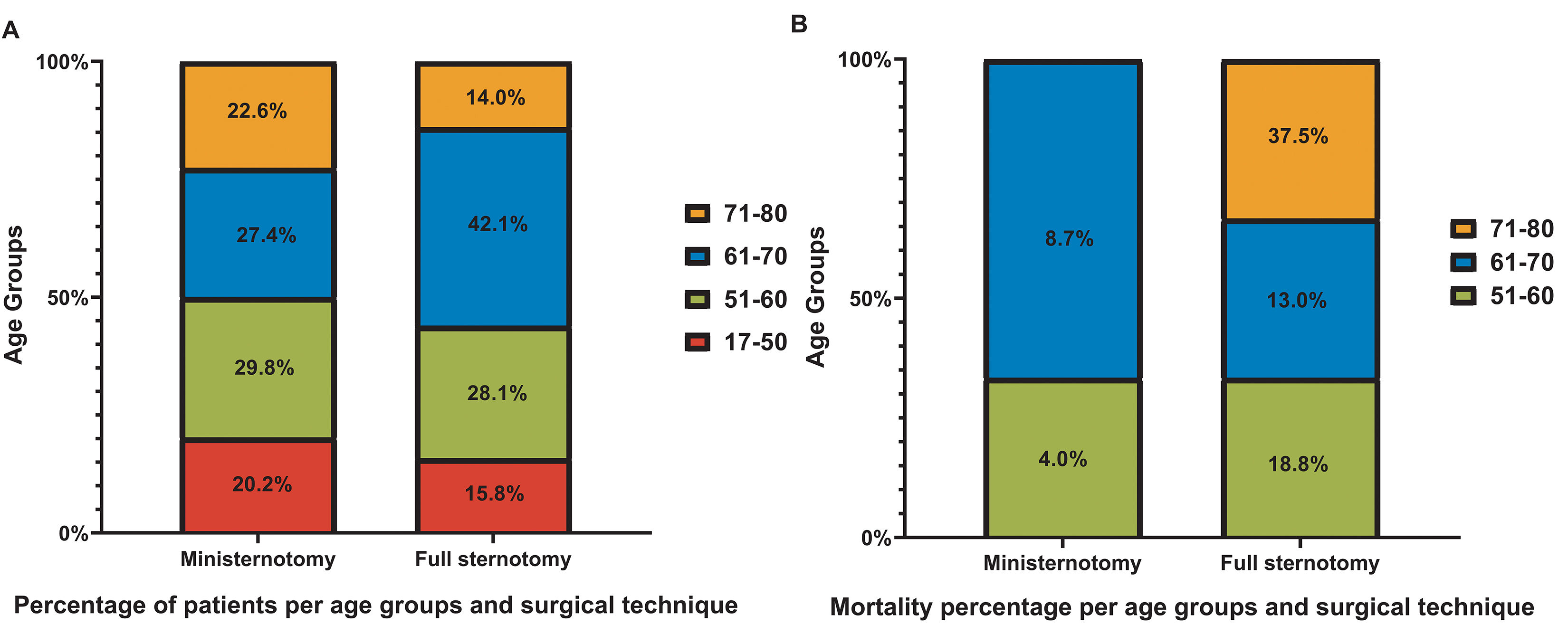
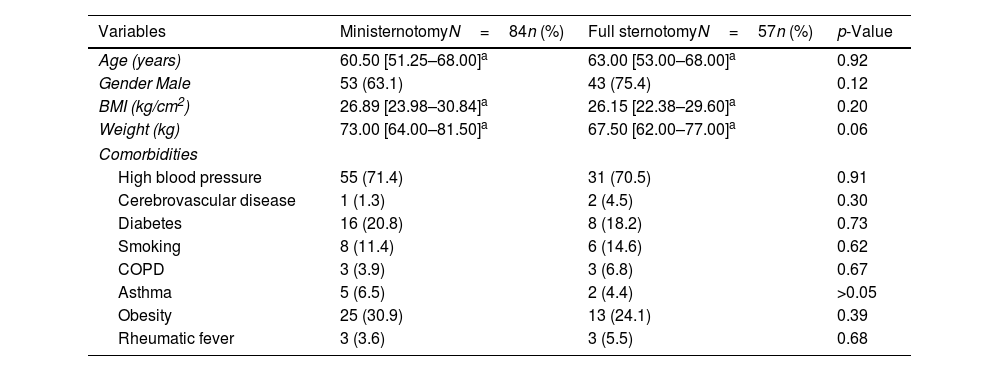
ResultsThe study included records of 141 patients who underwent AVR, 84 were operated through MS and 57 through FS. No difference was identified in baseline age between groups (MS 60.50 [51.25–68.00] vs. FS 63.00 [53.00–68.00], p=0.92). The population was stratified into 4 groups according to age (17–50, 51–60, 61–70, and 71–80 years) and separated according to the surgical technique, with no considerable differences in the distribution of patients among groups. Baseline characteristics are summarized in Table 1.
Baseline characteristics.
| Variables | MinisternotomyN=84n (%) | Full sternotomyN=57n (%) | p-Value |
|---|---|---|---|
| Age (years) | 60.50 [51.25–68.00]a | 63.00 [53.00–68.00]a | 0.92 |
| Gender Male | 53 (63.1) | 43 (75.4) | 0.12 |
| BMI (kg/cm2) | 26.89 [23.98–30.84]a | 26.15 [22.38–29.60]a | 0.20 |
| Weight (kg) | 73.00 [64.00–81.50]a | 67.50 [62.00–77.00]a | 0.06 |
| Comorbidities | |||
| High blood pressure | 55 (71.4) | 31 (70.5) | 0.91 |
| Cerebrovascular disease | 1 (1.3) | 2 (4.5) | 0.30 |
| Diabetes | 16 (20.8) | 8 (18.2) | 0.73 |
| Smoking | 8 (11.4) | 6 (14.6) | 0.62 |
| COPD | 3 (3.9) | 3 (6.8) | 0.67 |
| Asthma | 5 (6.5) | 2 (4.4) | >0.05 |
| Obesity | 25 (30.9) | 13 (24.1) | 0.39 |
| Rheumatic fever | 3 (3.6) | 3 (5.5) | 0.68 |
Note:
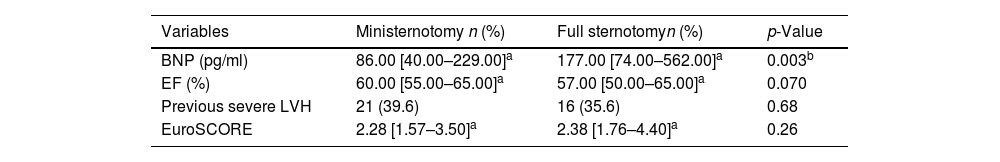
Main preoperative variables were similar between both groups (Table 2). The only difference identified was in atrial natriuretic peptide type B (BNP) range, which was higher in FS group.
Preoperative characteristics of the study population.
| Variables | Ministernotomy n (%) | Full sternotomyn (%) | p-Value |
|---|---|---|---|
| BNP (pg/ml) | 86.00 [40.00–229.00]a | 177.00 [74.00–562.00]a | 0.003b |
| EF (%) | 60.00 [55.00–65.00]a | 57.00 [50.00–65.00]a | 0.070 |
| Previous severe LVH | 21 (39.6) | 16 (35.6) | 0.68 |
| EuroSCORE | 2.28 [1.57–3.50]a | 2.38 [1.76–4.40]a | 0.26 |
Note:
Regarding the EuroSCORE surgical risk stratification, most of the population was at low risk. No differences were found between risk levels and the surgical technique (low risk MS 56.4% (n=44), EM 56.1% (n=32); intermediate risk MS 35.9% (n=28), MS 28.1% (n=16); and high risk MS 7.7% (n=6), MS 15.8% (n=9); p=0.28).
Intraoperative variables, aortic cross-clamp time and cardiopulmonary bypass time (CPB), which were similar in both groups. The median aortic cross-clamp time was 78.00min [67.50–91.25] and 77.00min [67.00–91.00], p=0.68 in MS and FS, respectively. While the CPB (median) was 98.50min [81.50–116.25] and 99.00min [87.75–124.00], p=0.48 respectively.
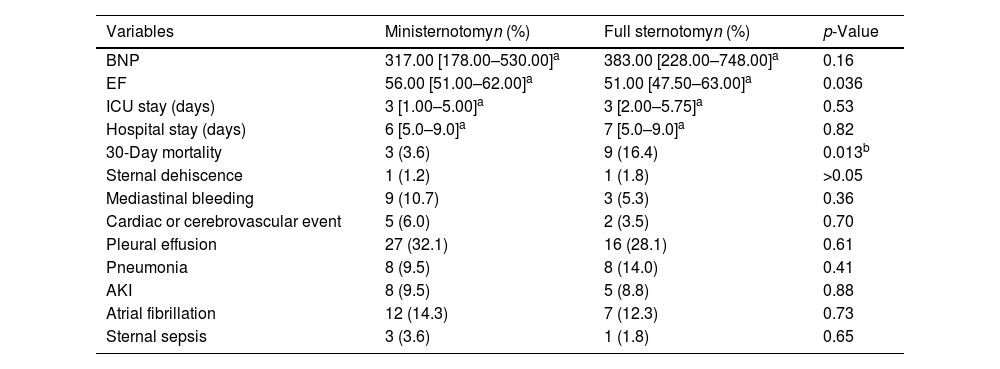
Postoperative characteristics between groups were highly similar (Table 3). It was observed that the ventricular ejection fraction was higher in ministernotomy (MS 56.0% [51.00–62.00] vs FS 51.00 [47.50–63.00], p=0.036). Mediastinal bleeding was more frequent in MS patients 10.7% (n=9) compared to FS 5.3% (n=3, p=0.36), although it was not significant. The conversion rate from MS to FS was 4.76% (n=4); (data was analyzed according to “intention to treat”).
Postoperative outcomes.
| Variables | Ministernotomyn (%) | Full sternotomyn (%) | p-Value |
|---|---|---|---|
| BNP | 317.00 [178.00–530.00]a | 383.00 [228.00–748.00]a | 0.16 |
| EF | 56.00 [51.00–62.00]a | 51.00 [47.50–63.00]a | 0.036 |
| ICU stay (days) | 3 [1.00–5.00]a | 3 [2.00–5.75]a | 0.53 |
| Hospital stay (days) | 6 [5.0–9.0]a | 7 [5.0–9.0]a | 0.82 |
| 30-Day mortality | 3 (3.6) | 9 (16.4) | 0.013b |
| Sternal dehiscence | 1 (1.2) | 1 (1.8) | >0.05 |
| Mediastinal bleeding | 9 (10.7) | 3 (5.3) | 0.36 |
| Cardiac or cerebrovascular event | 5 (6.0) | 2 (3.5) | 0.70 |
| Pleural effusion | 27 (32.1) | 16 (28.1) | 0.61 |
| Pneumonia | 8 (9.5) | 8 (14.0) | 0.41 |
| AKI | 8 (9.5) | 5 (8.8) | 0.88 |
| Atrial fibrillation | 12 (14.3) | 7 (12.3) | 0.73 |
| Sternal sepsis | 3 (3.6) | 1 (1.8) | 0.65 |
Note:
Regardless of the surgical technique, the median ICU stay after surgery was 3 days for all patients (MS 3 days [1.00–5.00] vs MS 3 days [2.00–5.75], p=0.53). Meanwhile, the median hospital stay after surgery was one day longer in FS, although this variance was not significant (MS 6 days [5.0–9.0] vs FS 7 days [5.0–9.0], p=0.84).
Overall 30-day mortality among all patients was 8.51%. The causes of early mortality within 30 days were cardiogenic shock, left ventricular dysfunction, ascending aorta tear, septic shock, among others. This rate was significantly higher in the FS group compared to the MS group (MS 3.6% (n=3) vs FS 16.4% (n=9), p=0.013).
Regardless the access route, the median age of deaths was 67.50 years [55.50–70.50] compared to 61.00 years [52.00–68.00] for survivors. However, no association between mortality and the participant's age was found (p=0.23).
Population distribution according to access route and age revealed that older patients undergoing AVR through FS may experience higher mortality. In contrast, no fatalities were reported among patients aged 71–80 years who underwent MIAVR (Fig. 1).
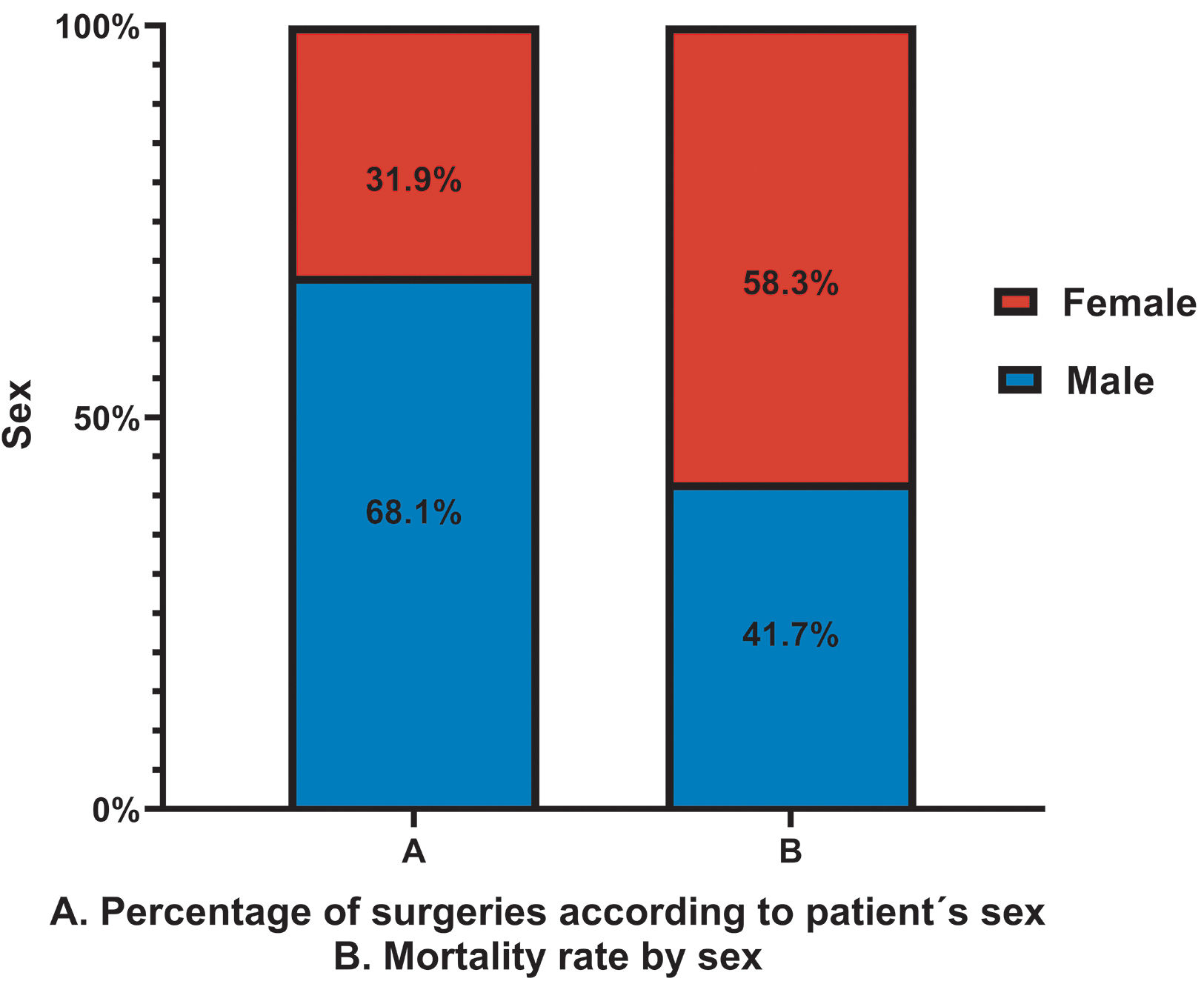
Regardless the access surgery, higher mortality was identified in females (p=0.040), despite the higher initial male-to-female ratio (greater than 2:1) (Fig. 2). Furthermore, a higher mortality rate among females is evidenced in segregated data by the access surgery.
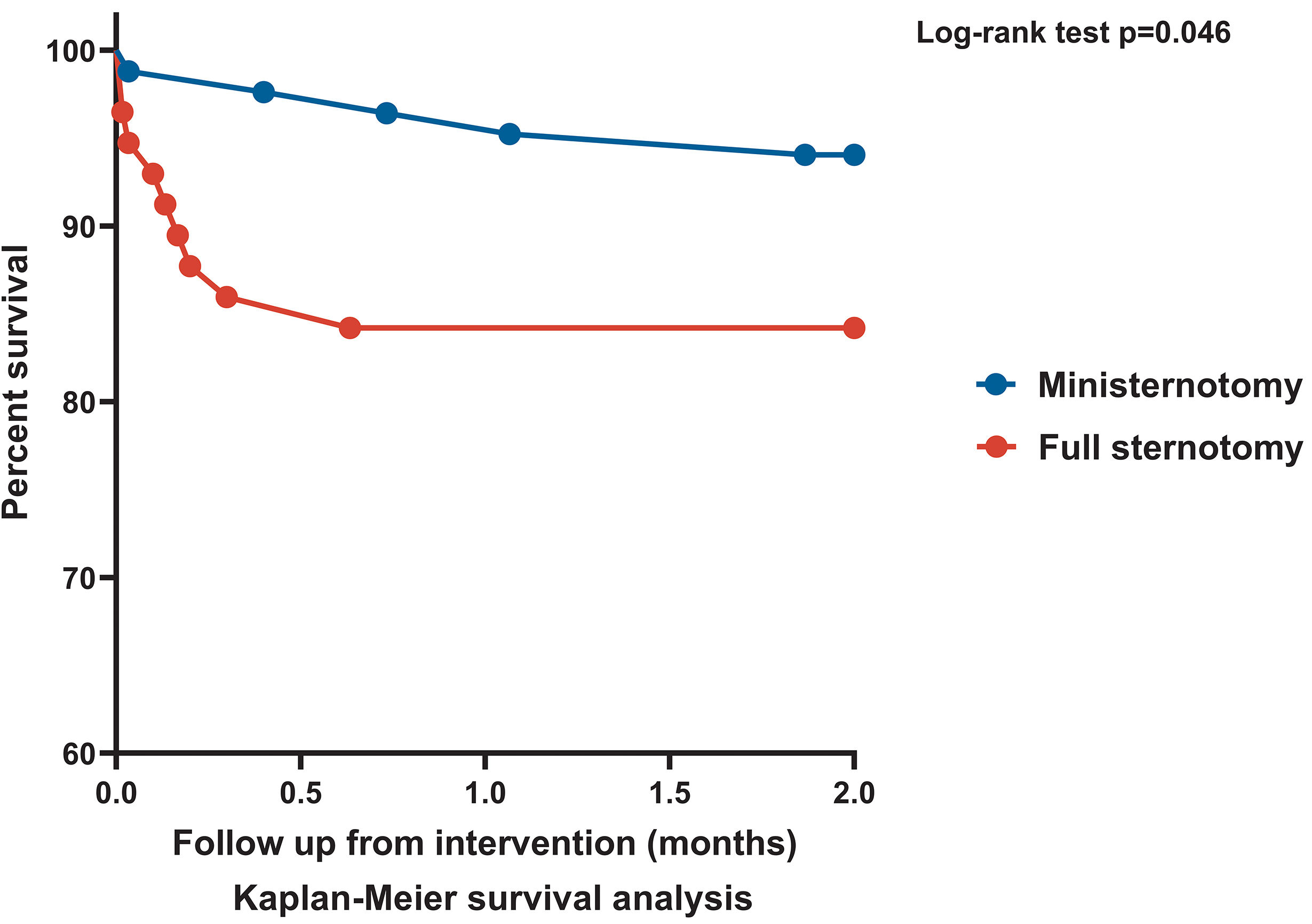
A significant difference was identified between the survival curves according to surgery at 30 (log-rank p=0.0096) and 60 (log-rank p=0.046) days after the intervention (Fig. 3). However, this difference did not persist beyond 90 days.
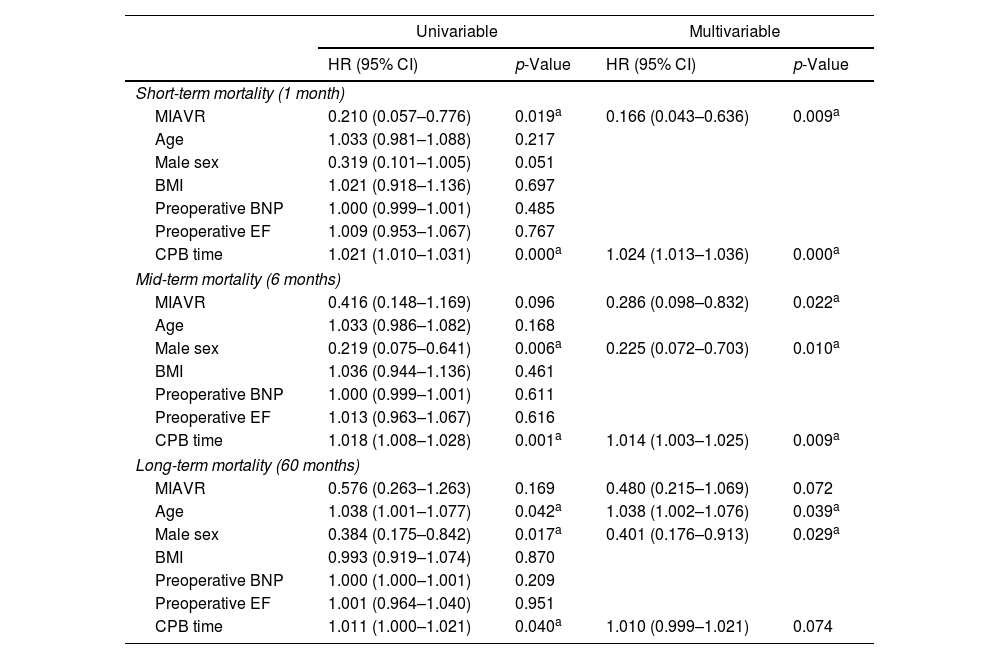
Cox regression analyses results for mortality risk factors are shown in Table 4. Univariable and multivariable analyses identified longer CPB time as predictor for short-term mortality; whereas MIAVR was identified as protective factor.
Cox regression analysis for investigating the effect of surgical approach mortality in the overall population.
| Univariable | Multivariable | |||
|---|---|---|---|---|
| HR (95% CI) | p-Value | HR (95% CI) | p-Value | |
| Short-term mortality (1 month) | ||||
| MIAVR | 0.210 (0.057–0.776) | 0.019a | 0.166 (0.043–0.636) | 0.009a |
| Age | 1.033 (0.981–1.088) | 0.217 | ||
| Male sex | 0.319 (0.101–1.005) | 0.051 | ||
| BMI | 1.021 (0.918–1.136) | 0.697 | ||
| Preoperative BNP | 1.000 (0.999–1.001) | 0.485 | ||
| Preoperative EF | 1.009 (0.953–1.067) | 0.767 | ||
| CPB time | 1.021 (1.010–1.031) | 0.000a | 1.024 (1.013–1.036) | 0.000a |
| Mid-term mortality (6 months) | ||||
| MIAVR | 0.416 (0.148–1.169) | 0.096 | 0.286 (0.098–0.832) | 0.022a |
| Age | 1.033 (0.986–1.082) | 0.168 | ||
| Male sex | 0.219 (0.075–0.641) | 0.006a | 0.225 (0.072–0.703) | 0.010a |
| BMI | 1.036 (0.944–1.136) | 0.461 | ||
| Preoperative BNP | 1.000 (0.999–1.001) | 0.611 | ||
| Preoperative EF | 1.013 (0.963–1.067) | 0.616 | ||
| CPB time | 1.018 (1.008–1.028) | 0.001a | 1.014 (1.003–1.025) | 0.009a |
| Long-term mortality (60 months) | ||||
| MIAVR | 0.576 (0.263–1.263) | 0.169 | 0.480 (0.215–1.069) | 0.072 |
| Age | 1.038 (1.001–1.077) | 0.042a | 1.038 (1.002–1.076) | 0.039a |
| Male sex | 0.384 (0.175–0.842) | 0.017a | 0.401 (0.176–0.913) | 0.029a |
| BMI | 0.993 (0.919–1.074) | 0.870 | ||
| Preoperative BNP | 1.000 (1.000–1.001) | 0.209 | ||
| Preoperative EF | 1.001 (0.964–1.040) | 0.951 | ||
| CPB time | 1.011 (1.000–1.021) | 0.040a | 1.010 (0.999–1.021) | 0.074 |
Note:
MIAVR showed no influence on mid-term mortality in univariable analysis. Univariable and multivariable analysis identified longer CPB time as an independent predictive risk factor, while male sex was protective in mid-term mortality. Multivariable analysis showed influence of MIAVR on mid-term mortality [HR 0.286 (0.098–0.832), p=0.022].
Surgical approach univariable and multivariable analysis showed no influence in long-term mortality. Univariable Cox regression analyses identified age and CPB time as predictors for late mortality; while male sex was identified as protective factor for late mortality. Multivariable analysis showed age (HR 1.038, 95% CI 1.002–1.076, p=0.039) as the independent predictive risk factor for long-term mortality. Male sex (HR 0.401, 95% CI 0.176–0.913, p=0.029) was identified as protective factor.
DiscussionThis study represents the first regional initiative that compares outcomes of MS and FS as access route to AVR in a low-volume center. Although international studies comparing these techniques have been conducted, regional evidence remains scarce11–13 and most results are inconclusive.14
In contrast to other regions reports,4,15–17 this study observed a higher percentage of patients undergoing MIAVR.
Baseline characteristics are comparable between groups and are similar to those reported in other investigations.11,18 A higher prevalence of AVR surgeries was identified in males, which could be linked to the higher incidence of bicuspid aortic valve disease or diagnosis in men19 and a higher risk of coronary artery disease, leading to earlier referrals.19,20 These findings are consistent with international literature.12,21–23 The main comorbidities recorded in this population include high blood pressure, obesity, diabetes, and smoking, as previously documented.6,12,15,24 The percentage of obesity observed is higher than reported in other studies,14,16,17 this aspect could be relevant since it is a known risk factor for cardiovascular diseases25 and is associated with higher stenosis risk and AVR.26 Although no significant difference in obesity rates between groups was observed, MS patients exhibited a slightly higher weight. However, there is insufficient evidence to confirm a significant difference that could affect the results as suggested.25 Additionally, body mass index (BMI) stratification shows that most patients, regardless of the surgical technique, belong in the overweight category.
Contrary to what is commonly reported, where MIAVR associates with increased aortic cross-clamp time and CPB times mainly due to the reduced space and limited surgical exposure,4,15,18,27,28 this investigation found no significant differences between groups in these times, aspect consistent with a recent study suggesting that surgical technique experience may influence these outcomes.29
Mediastinal bleeding was defined in this study as bleeding that required the use of blood product transfusions. Although the overall bleeding rate identified might seem elevate, it aligns with the values reported by other group between 3% and 10%.30,31
Several investigations have reported less postoperative bleeding in MIAVR.3,4,6,12,15 However, in this study, although not statistically significant, MS patients showed a higher percentage of mediastinal bleeding. This difference could be related to MS to FS conversions, which in all cases respond to the case's complexity and the presence of unforeseen conditions during the intervention. The conversion rate in this study (4.76%) is similar to that reported in a pragmatic, open-label controlled trial carried out in the United Kingdom.32 However, other regions have reported lower reconversion rates, ranging from 2% to 4%.6,9,12
Some authors have reported that ICU and hospital stay are shorter in MIAVR.14,33–35 However, in the present study, the ICU median stay was 3 days regardless of the technique used, a measure consistent with findings reported in a study conducted in Mexico.12 Regarding hospital stay, although it appears to be shorter by approximately one day in patients undergoing MIAVR compared to those undergoing FS, this difference was not statistically significant. A similar aspect has been reported by other authors5,7,22 where the absence of significance could be due to the size of the study population. The preoperative and postoperative care protocols were standardized for both groups, with all patients routinely admitted to the ICU during the immediate postoperative period and receiving uniform standard care. This approach can minimize variability in outcomes.
At the institutional level, ICU management policies for cardiac patients mandate a minimum stay of two days. This study marked our first experience that prompted a revision of ICU policies for minimally invasive surgeries. Since 2012, a home care program has been implemented as part of the protocol, enabling patients to be discharged on the fifth postoperative day to continue their recovery at home. This initiative could potentially influence the length of hospital stay while ensuring patients receive ongoing care under the supervision of home care physicians specifically trained in cardiac surgery.
MIAVR is associated with a significant reduction in the 30-day mortality rate, a finding consistent with reports from other European studies14,36 and is estimated to be related to a decreased surgical trauma and faster postoperative recovery.36 Furthermore, a recent multicenter study supports this observation, reporting shorter postoperative hospital stays for MS patients compared to those who underwent FS.37
Although, no deaths were reported in this study among adults aged 71–81 years who underwent MIAVR, compared to those who received conventional surgery, this investigation includes a relatively small population. Consequently, further studies with larger and more diverse populations are needed.
Other retrospective initiatives have also noted that MIAVR leads to lower morbidity and mortality compared to FS in elderly patients.38
Despite the surgical technique used for AVR, a significant association between mortality and female sex was observed. This situation has been widely described previously, and several authors have identified female sex as a risk factor for mortality after cardiac intervention.19,20 Anatomical and physiological factors could contribute to the disparity in mortality.20,39 However, in our population, no evidence has been found to support the relevance of these factors. Therefore, we do not consider these explanations to be applicable to the reality of our country and the cause of these findings will be left for future research.
The mortality rates observed in this study are significantly higher than those predicted by EuroSCORE. It has been shown that, in certain populations, including Latin America, its performance may underestimate the mortality risk.40 Additionally, the differences in technology, surgical expertise, and training resources between developed and low- to middle-income countries may also contribute to the observed variations in mortality rates.
As well, high-volume centers have shown lower mortality rates at 30-day and 1-year compared to low-volume centers.41
Regarding short-term survival, this study determined that it is higher in MS patients for the first and second postoperative month. This is partially consistent with findings from a German study, which identified a significant difference in short- and long-term survival rates in favor of ministernotomy.37 Regionally, evidence is scarce, and to date, no difference between the groups has been found. A study conducted in Chile found no difference between the groups,11 and other studies didn’t evaluate survival.12,13 It is necessary to mention that this difference was not observed in the long term.
LimitationsAs this research incorporates a retrospective data analysis, it presents some limitations, such as the possibility of selection biases since the information was recorded based on the availability of medical records, and the existence of missing data or interpretation errors. It is also necessary to mention that despite being one of the studies with the largest number of patients recorded in the region, the size of the analyzed population remains relatively small, which could limit the ability to detect significant differences between groups. Additionally, this data reflects the experience of a single hospital center and specifically relates to a technique where experience and expertise play a fundamental role; therefore, the results would not be easily extrapolated to other scenarios.
ConclusionThis study showed that in a low-volume center, MIAVR using MS is a feasible and safe technique, with outcomes comparable to the standard approach. FS was associated with a higher 30-day mortality rate and patients undergoing MS exhibited greater short-term survival, suggesting that the technique may impact mortality. Thus, this research may have a great impact not only for the region, where evidence is lacking, but also for low-volume centers seeking adaptable information to their realities and developing minimally invasive cardiac surgery programs worldwide. It provides insights that enable decision-making and progress toward achieving better patient outcomes without the need for large economic or logistical investments. However, to consolidate the findings identified in this research, it is advisable to propose additional studies with increased patient numbers, and prospective interventions. Furthermore, it is essential to encourage the development of similar initiatives in the region.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Conflict of interestsThe authors have no conflicts of interest to declare.
None.