Laparoscopic surgery is well accepted as a safe technique when performed on a third trimester pregnant woman.
ObjectiveThe aim is to describe the anaesthetic management of a group of patients undergoing this type of surgery.
Material and methodsAn analysis was made of records of 6 patients in their third trimester of pregnancy and who underwent urgent laparoscopic surgery from 2011 to 2013.
Clinical CasesThe study included 6 patients, with a diagnosis of acute cholecystitis in 4 of them. The other 2 patients had acute appendicitis, both of who presented threatened preterm labour.
ConclusionThe most frequent indications for laparoscopic surgery during the last trimester of birth were found to be acute cholecystitis and acute appendicitis. Acute appendicitis is related to an elevated risk of presenting threatened preterm labour.
Anteriormente la cirugía laparoscópica se contraindicaba en el tercer trimestre de gestación, aunque recientemente ha ganado aceptación como la técnica más segura para el binomio madre-hijo.
ObjetivoDescribir el manejo anestésico y la evolución clínica de las pacientes que cursan el tercer trimestre de gestación y requirieron cirugía laparoscópica de urgencia en el Hospital General Dr. Manuel Gea González.
Material y métodosEstudio transversal, descriptivo y observacional. Se seleccionaron de la base de datos los expedientes clínicos de las pacientes embarazadas en el tercer trimestre que ameritaron cirugía laparoscópica de urgencia durante el período de enero de 2011 a abril de 2013 en el Hospital General Dr. Manuel Gea González.
Casos clínicosSe incluyeron 6 pacientes. Cuatro se intervinieron por colecistitis aguda y 2 por apendicitis aguda. Dos recibieron anestesia total intravenosa y 4 anestesia general balanceada. Todas recibieron tocolisis profiláctica y el feto fue vigilado en el perioperatorio por un ginecoobstetra. Las 2 pacientes con apendicitis presentaron amenaza de parto pretérmino.
ConclusiónEn el tercer trimestre del embarazo puede requerirse cirugía urgente por diversas dolencias; en nuestro estudio se presentó en el 72% por colecistitis y en el 28% por apendicitis. La sepsis abdominal es factor de riesgo para amenaza de parto pretérmino.
The majority of anaesthetists are familiar with patient management during birth and in caesarean section operations but when the pregnant patient undergoes non-obstetric surgery it is a different matter, since the actual anaesthetic implications of pregnancy are to be managed in addition to those of the laparoscopic surgery1.
It has been calculated that in the United States 2% of pregnant women undergo some type of emergency non-obstetric surgery,2 per year and this becomes a challenge for both the anaesthetist and the surgeon. The main aspects of consideration are: the anaesthetic risk of the mother relating to her pregnancy, the drugs to be used and the maintenance of correct utero-placental blood flow.3–5 The most frequent surgical interventions in these patients are: appendectomies, cholecystectomies and adnexal surgery.6–8 It is believed that 4.5% of pregnancies continue full term with non symptomatic cholecystitis whilst only 0.05% present with acute cholecystitis. Of the latter, 40% require surgical intervention.9,10 The specific risks for the mother and for the foetus when undergoing non-obstetric surgery are: loss of foetus, foetal asphyxia, pre-term labour, membrane rupture, associated risks of unsuccessful intubation and thromboembolic phenomena.11,12
Up until recently, the lack of experience of this type of intervention in the third trimester of pregnancy resulted in it being a contraindication. At present, despite the increase of this procedure, there is still a need for further guidelines or directives for correct management of anaesthesia.
The aim of this study was to describe the experience we had with anaesthesia management in emergency laparoscopic surgery in third trimester pregnant women.
Material and methodsA transversal, descriptive, observational study was conducted which had been previously approved by the Research and Ethics of Research Committee of the Hospital General Dr. Manuel Gea González. The data base was reviewed for the surgical interventions carried out in the hospital, from 1st January 2011 to 30th April 2013.
All cases of emergency laparoscopic surgery for third trimester pregnant patients which took place between 1st January 2013 and 30th April 2013 were included. Cases without a complete medical record were excluded.
Data was collated relating to medical information, post-operative diagnosis, anaesthetic management, haemodynamic behaviour during surgery and the evolution of the patient and her baby.
The following data was recorded: patients’ ages, number of pregnancies, weeks of gestation when undergoing surgery, anaesthetic technique used, blood pressure during surgery, foetal heartbeat and uterine activity before and after surgery, transportation to the post-anaesthetic care unit or the intensive therapy unit, reason for pregnancy termination, method (delivery or caesarean section) and weeks of pregnancy at delivery.
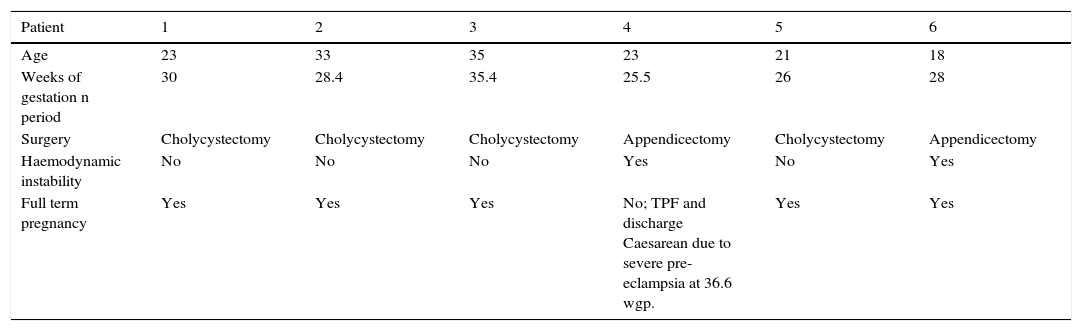
ResultsDuring the period of study 6 laparoscopic surgical procedures were carried out. These are described below.
Case 1Patient aged 23, with multiple pregnancies, 3 previous deliveries and a current pregnancy of 30 weeks gestation period. She started with symptoms indicative of cholecystitis during the first trimester of pregnancy and went to a private physician who confirmed the diagnosis with ultrasonography and recommended cholecystectomy after delivery. However, the symptoms increased and she was referred to the Hospital General Dr. Manuel Gea González for assessment. The diagnosis of cholecystitis was confirmed and it was decided that laparoscopic cholecystectomy be performed. The gynaecology department monitored the foetal heart rate during hospitalisation and before and after surgery. No abnormalities were found at any time.
Nifedpine tocolysis was administered prophylactically from one day prior to the procedure and betamethasone for lung maturity. The anaesthetic technique consisted of the administration of a general balanced anaesthesia based on fentanyl, propfol and desflurane and with rocuronium as a neuromuscular relaxant. Surgery was performed without incident for a period of 50min. The mean blood pressure was stable and above 70mmHg. The patient was extubated without any problem and taken to the post-anaesthetic care unit, where the foetal heart rate was again monitored. She was transferred to her hospital room and discharged from hospital after 2 days. The pregnancy went to term in the same hospital, with a healthy baby being delivered vaginally.
Case 2Patient aged 33, with multiple pregnancies, with one previous delivery and a current pregnancy of 28.4 weeks gestation period. She was referred from another hospital with acute cholelithiasis. The patient presented with jaundice and total bilirubin levels in the blood of 4mg/dl. The diagnosis of acute cholelithiasis and cholestatic jaundice was confirmed and a laparoscopic cholecystectomy under general anaesthetic was proposed (sufentanil, propfol, rocuronium and desflurane). The administration of anaesthesia was without incidence and the patient remained haemodynamically stable.
Nifedpine was administered as a tocolytic and betamethasone for prophylactic lung maturity by the Obstetrics and Gynaecological Department. Foetal heart rate was monitored intermittently during her hospital stay, and stayed within standard parameters. The duration of surgery was 65min. On extubation the patient was transferred to the post-anaesthetic care unit and later to her hospital room. She was discharged the following day. Telephonic follow-up was used and she informed us that her pregnancy had progressed to full term, and that she had had a healthy baby delivered vaginally in a hospital in the State of Mexico.
Case 3Patient aged 35, pregnant for the first time and at 35.5 weeks gestation period, who presented at the Emergency Department of Hospital General Dr. Manuel Gea González with a colicky type abdominal pain, a dull ache, located in the epigastrium, which increased with the ingestion of cholecystokinetics. Clinical symptoms were accompanied by fever, nausea and vomiting. Abdominal ultrasound was performed after which the diagnosis of cholelithiasis was made. Laparoscopic cholecystectomy was performed the following day under total intravenous anaesthesia based on the administration of sufentanil, propfol, and rocuronium. Rectal indomethacin was administered as a tocolytic and betamethasone to promote lung maturity.
Surgery duration was 45min and after extubation the patient was transferred to the post-anaesthetics care unit and later to her hospital room. She was discharged from hospital the following day and her pregnancy continued to be monitored in the Hospital General Dr. Manuel Gea González. She had an apparently healthy baby by vaginal delivery at 39 weeks of pregnancy.
Case 4Patient aged 23, with multiple pregnancies, one previous delivery and one previous abortion, currently in her third pregnancy at 25.5 weeks gestation period. The patient mentioned she had suffered from diffuse abdominal pain, nausea and vomiting of one-week duration, and therefore went to her private doctor who prescribed paracetamol and bonadoxin. As a result of no improvement she presented at the Emergency Department of the Hospital General Dr. Manuel Gea González, where she was diagnosed with a fever of 39°C and leucocytosis of 21,000/mm3 The diagnosis of probable acute appendicitis was given, and diagnostic laparoscopy under general anaesthesia based on fentanyl, propofol, rocuronium and desflurane was performed with the discovery of an acute stage III appendicitis. An appendectomy was therefore performed. During surgery, which lasted for 65min, the patient presented with a tendency towards hypotension. A mean blood pressure of 60mmHg was even reported. This responded to the administration of intravenous chrystalloid fluids and did not require aminergic support.
Similarly to the other patients she received foetal lung maturity based on betamethasone, and tocolysis with rectal indomethacin. She was extubated and monitored in the post-anaesthetics care unit immediately after surgery. Foetal heart rate stayed within normal parameters. However, 6h after surgery there was uterine activity and a threat of pre-term delivery. This was managed by the administration of nifedipine, with additional doses of rectal indomethacine and complete repose.
The threat of pre-term labour receded and she was discharged 2 days later, with the recommendation that alarm signals would require further assessment by the emergency services. The patient returned at 36.6 weeks of gestation period due to headaches and tinnitus. Her blood pressure was 160/100mmHg, there was oedema in her lower limbs and protein in her urine. It was decided that a caesarean be performed due to pre-eclampsia. A healthy baby was delivered and both mother and baby were monitored for 2 days, after which they were discharged from the hospital.
Case 5Patient aged 21, who had already had 2 caesarean sections and a previous normal delivery. Her current pregnancy was at 26 weeks gestation period. She had a week-long duration of a colicky type abdominal pain, unspecified fever, and yellow colouring in the whites of her eyes, for which she presented at the Emergency Department of the Hospital General Dr. Manuel Gea González, where an abdominal ultrasound was performed. This revealed a gallbladder with an enlarged wall, a double halo image and dilated bile duct. We decided to perform cholecystectomy the following day. The operation lasted 40min and total intravenous anaesthesia was administered based on sufentanil, propfol, and rocuronium. The patient remained haemodynamically stable and foetal heart rate remained within standard parameters before and after surgery. The patient was discharged the following day and her pregnancy reached full term, with an apparently healthy baby being born by caesarean section and short birth interval in a maternity hospital of the Federal District. We obtained this information telephonically.
Case 6Patient aged 18, with multiple pregnancies, 2 previous deliveries and a current pregnancy at 28 weeks gestation period. She presented with abdominal pain of 8-day duration which she had not previously consulted a doctor about. On reaching the Surgical Department of the Hospital General Dr. Manuel Gea González she presented with signs of severe sepsis (fever of 39°C, leucocytosis of 24,000/mm3, pre-eclampsia and blood pressure of 90/60mmHg), abdominal pain in the lower left quadrant and clear symptoms. We decided to perform a diagnostic laparoscopy for a probable appendectomy. The procedure was performed under general anaesthesia, which was started using a rapid sequence intubation based on fentanyl, propfol, and rocuronium. Foetal heart rate stayed within normal levels before and after surgery and the patient received tocolysis and foetal lung maturity with the administration of nifedipine and betamethasone respectively. The patient presented with haemodynamic instability, which required aminergic support with norepinephrine, administered via a central venous catheter placed at the anterior jugular vein during surgery, which led to a mean blood pressure level remaining at above 65mmHg. The appendectomy due to acute stage IV appendicitis lasted for 70min. She was intubated and taken to the intensive care unit of the hospital. During her stay she presented with pre-term labour which was managed with the administration of tocolytics (nifedipine and indomethacin) by the obstetrics and gynaecological department and was resolved after 5 days. She was discharged from hospital thirteen days later and the pregnancy progressed to full term (see Table 1).
Main characteristics of the cases.
| Patient | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| Age | 23 | 33 | 35 | 23 | 21 | 18 |
| Weeks of gestation n period | 30 | 28.4 | 35.4 | 25.5 | 26 | 28 |
| Surgery | Cholycystectomy | Cholycystectomy | Cholycystectomy | Appendicectomy | Cholycystectomy | Appendicectomy |
| Haemodynamic instability | No | No | No | Yes | No | Yes |
| Full term pregnancy | Yes | Yes | Yes | No; TPF and discharge Caesarean due to severe pre-eclampsia at 36.6 wgp. | Yes | Yes |
TPD: threat of pre-term delivery; wgp: weeks of gestation period.
In our study we found that the most frequent reasons for performing diagnostic laparoscopy in pregnant women were cholecystitis and appendicitis. This has also been reflected in previous studies.12 In our research we found that appendicitis is directly related to threatened pre-term labour, a fact that was described by Meis et al.13 They also discovered that abdominal sepsis was a risk factor for the development of threatened pre-term labour which is comparable to that found in our study, where the patients with complicated appendicitis presented with threatened pre-term labour. Haemodynamic instability, specifically a mean blood pressure below 65mmHg, has been described in the literature as an additional risk factor for the development of pre-term labour. However, in our study the patient who presented with trans-anaesthetic hypotension did not have threatened pre-term labour.
Although we agree that pregnancy is not the ideal moment to perform non-obstetric surgery, we are also aware that surgical emergencies may occur in all population groups and that pregnant women are no exception. As this is the case, an anaesthetic technique requires selecting. Our study aimed to provide information to support the safety of laparoscopy in pregnant patients.
ConclusionsIt is particularly important to quickly recognise the main abdominal conditions in pregnant patients (appendicitis, cholecystitis) to establish the correct protocol and to avoid complications.
In general, laparoscopic surgery during the third trimester of pregnancy is associated with good peri-natal outcomes. Pre-term labour appears to be more related to the underlying sickness rather than the surgical or anaesthetic procedure itself. The key to success in the peri-operative care of the pregnant woman for non-obstetric surgical intervention is therefore the work of the gynaecologist, obstetrician, surgeon and anaesthetist.
Laparoscopic procedures are increasingly preformed during pregnancy. Current evidence shows that the approach is a safe alternative and applicable during pregnancy and that it is an effective tool for the prevention of associated complications.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: López-Collada Estrada M, Martínez RO. Cirugía laparoscópica de urgencia en el tercer trimestre de gestación y su manejo anestésico. Experiencia de un hospital general. Cir Cir. 2016;84:429–433.