The mortality of cutaneous melanoma has not declined over the past 50 years. The only interventions that can reduce mortality are primary prevention and early diagnosis, and the dermoscopic evaluation is essential to achieve this. Dermoscopy identifies characteristics of melanoma that would go unnoticed to the naked eye.
The aim of this paper is to report the most frequent dermoscopic findings in patients diagnosed with in situ and invasive melanoma.
Material and methodsAn observational and retrospective study of contact dermoscopy was performed using LED Dermlite™ and camera Dermlite™ dermoscope. The findings evaluated were: asymmetry in two axes, association of colours, lack of pigment, irregular points, atypical network, pseudopods, blue veil, ulceration, and peri-lesional pink ring. These dermoscopic findings were compared with the histological diagnosis.
ResultsThe study included 65 patients with cutaneous melanoma; 10 in situ, and 55 invasive. The mean Breslow in invasive melanoma was 3mm. Most patients (35) had localisation in extremities. In all patients, the most frequent dermoscopic finding was asymmetry in two axes, followed by association of two or more colours; in melanoma in situ, asymmetry was the most frequent, followed by atypical-irregular points. In invasive melanoma asymmetry in two axes, the association of two or more colours, and pseudopods, were the most frequent findings.
ConclusionAsymmetry in two axes is the most common dermoscopic finding in in situ and invasive melanoma. The presence of two or more colours in a pigmented lesion should be suspected in an invasive melanoma.
La mortalidad del melanoma cutáneo no ha disminuido en los últimos 50 años. Las únicas medidas que permiten reducirla son la prevención primaria y el diagnóstico oportuno; la evaluación dermatoscópica es fundamental para lograrlo. Permite identificar características del melanoma que pasarían desapercibidas al ojo desnudo.
El objetivo es reportar los hallazgos dermatoscópicos más frecuentes en pacientes con diagnóstico de melanoma in situ e invasivo.
Material y métodosEstudio observacional, retrospectivo en el que se realizó dermatoscopia de contacto utilizando dermatoscopio LED DermliteMR, y cámara fotográfica DermliteMR. Se evaluó asimetría en 2 ejes, asociación de colores, falta de pigmento, puntos irregulares, red atípica, pseudópodos, velo azul, ulceración y anillo rosa perilesional, y se comparó el diagnóstico histológico con los hallazgos dermatoscópicos.
ResultadosFueron 65 pacientes con melanoma cutáneo: 10 in situ y 55 invasivos. La media de Breslow en invasivos fue 3mm. La mayoría de los pacientes (35) tuvieron localización en extremidades. El hallazgo dermatoscópico más frecuente fue asimetría en 2 ejes, seguida de asociación de 2 o más colores; en melanoma in situ el hallazgo más habitual fue la asimetría en 2 ejes seguida de los puntos atípicos; en melanoma invasivo la asimetría en 2 ejes, la asociación de 2 colores o más y los pseudópodos fueron los hallazgos más frecuentes.
ConclusiónLa asimetría en 2 ejes es el hallazgo dermatoscópico más frecuente en melanoma ya sea in situ o invasivo; la presencia de 2 colores o más en una lesión pigmentada debe hacer sospechar de un melanoma invasivo.
Dermatoscopy is a non-invasive technique for the assessment of pigmented lesions aimed at ruling out the presence of cutaneous melanoma. Its correct application makes it possible to decide which lesions are clinically suspicious and should undergo resection or biopsy for diagnostic purposes. It allows for the assessment of skin structures in vivo, from the epidermis to the papillary dermis, which are not visible with the naked eye. Pigment characteristics and distribution in these areas are different in benign lesions and melanoma. The diagnostic certainty of a pigmented lesion assessed with dermatoscopy increases by 30%.1
The removal of all pigmented lesions leads to a high rate of false positives and unnecessary biopsies. On the other hand, failure to suspect of a pigmented lesion corresponding to an incipient melanoma could lead to a late diagnosis.
Due to the lack of effective adjuvant treatments and the fact that melanoma mortality has not changed over the last years, the only alternative for survival improvement is the timely diagnosis in phases where the cutaneous melanoma is thin.
However, deciding which lesions are melanoma and which are not is complex, particularly so in cases with in situ or very thin melanomas (smaller than 1mm and non-ulcerated).
Dermatoscopy is probably the best clinical test that allows for the identification of pigmented lesions with suspected cutaneous melanoma. It is based on the microscopic assessment of pigmented lesions, which allows for the assessment of melanoma-related pigmentation characteristics.
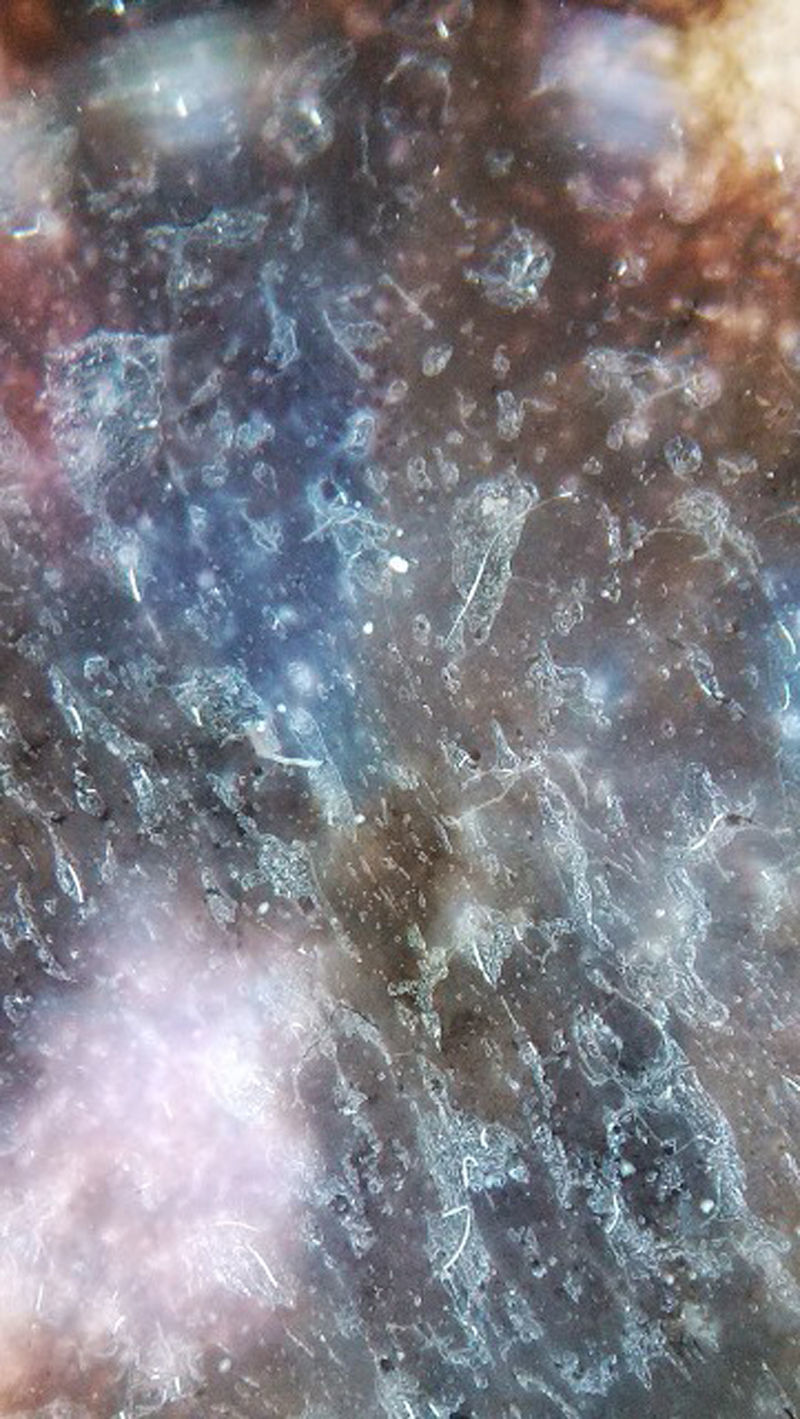
In Mexico, most cutaneous melanomas have historically been diagnosed in locally advanced stages,2,3 with not only dermatoscopic but also clinical macroscopic data which clearly indicates neoplasia, such as ulceration, bleeding and vertical-growth phase (Fig. 1). In these patients, dermatoscopy does not provide more data for the diagnosis of cutaneous melanoma. Nevertheless, in patients with incipient lesions, although they are a minority, the decision of removal or no removal depends on several factors and is particularly important when the melanoma is located in areas which may affect aesthetics or function (the face and soles of feet, for example).
There are many dermatoscopic characteristics associated with cutaneous melanoma, and many of them depend on the experience of the observer and may be somewhat subjective. However, the most common ones include asymmetry and changes in the distribution pattern of colour characterised by the combination of 2 or more colours, or by the presence of irregular pigmented dots. The presence of one or more of these characteristics is generally related to the thickness of the tumour (Breslow), and changes are less evident in superficial and in situ melanomas; the intensity of changes and the number of dermatoscopic findings in pigmented lesions are inversely proportional to the Breslow's level of melanoma.
In general, the “ABCD rule” (asymmetry, border, colour and diameter)4 is recommended for the clinical assessment of pigmented lesions. Nevertheless, this algorithm does not always make it possible to distinguish pigmented lesions from non-pigmented lesions, and it is not considered a reliable technique for superficial melanomas. Changes, particularly in height, appear in intermediate-thickness to thick melanomas.
The objective of this article is to identify which are the most common dermatoscopic findings in patients with cutaneous melanoma without clinical evidence.
Material and methodsThis is an observational and retrospective study which included patients with histological diagnosis of cutaneous melanoma assessed before resection both in a clinical manner and through dermatoscopy. Patients who had clinical evidence of melanoma (tumour, ulceration, exophytic growth) were not included. The study only involved patients with lesions which from a naked-eye clinical assessment could not be identified as a pigmented lesion or a melanoma.
All patients who had appointments during 1 year due to pigmented lesions were assessed with dermatoscopy, using the dermatoscopy DermliteMR, and later photographed with the dermatoscopic camera with LED light DermliteMR. Lesions were analysed with polarised light and/or immersion oil and white LED light. Dermatoscopic characteristics were recorded. In patients with proven melanoma, dermatoscopic findings were correlated with histological characteristics of neoplasia.
The initial dermatoscopy was conducted with the 2-step algorithm: (1) decide whether the pigmented lesion was melanocytic; and (2) If so, determine if it had melanoma characteristics. However, as the study included only patients with cutaneous melanoma, a second step was carried out in which dermatoscopic findings were correlated with prognostic factors for neoplasia.
The dermatoscopic findings analysed were the following: 2-axes asymmetry, colour association, areas with no pigmentation, irregular and atypical pigment dots, atypical pigment network, pseudopods, presence of blue veil, ulceration and peripheral erythema (pink ring).
The study included patients with cutaneous melanomas located anywhere in the body, while patients with mucosal, subungeal, scalp and interdigital melanomas were excluded.
Since there are pigmented lesions with clinical characteristics that confirm the invasive melanoma diagnosis, where dermatoscopy only confirms findings but is not determinant in the diagnosis (Fig. 1), this type of lesions was excluded from the analysis and lesions were only included in cases where the clinical analysis was not evident or presented doubtful melanoma findings (Fig. 2).
ResultsThe study included 65 patients with cutaneous melanoma diagnosis: 40 female patients and 25 male patients, between 18–90 years and a mean age of 65.
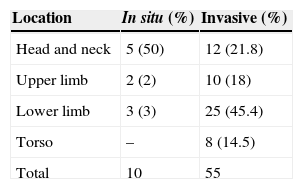
The anatomical sites of melanoma are shown in Table 1.
Location of cutaneous melanoma.
| Location | In situ (%) | Invasive (%) |
|---|---|---|
| Head and neck | 5 (50) | 12 (21.8) |
| Upper limb | 2 (2) | 10 (18) |
| Lower limb | 3 (3) | 25 (45.4) |
| Torso | – | 8 (14.5) |
| Total | 10 | 55 |
Location of in situ and invasive melanomas: most melanomas are located on limbs (59%); 50% of in situ melanomas were located on the head and neck, mainly on the face.
Ten patients were diagnosed with in situ melanoma, and 55 patients were diagnosed with invasive melanoma. The types of diagnosed melanomas included: lentigo malignant melanoma in 10 patients, superficial spreading melanoma in 20, and lentiginous acral melanoma in 35.
Lentigo malignant melanoma was located on the facial skin in 3 cases, on the auricular helix area in 2, on the hand dorso in 1, on the thenar eminence in 1, on the front of the thigh in 2, and on the back of the leg in 1.
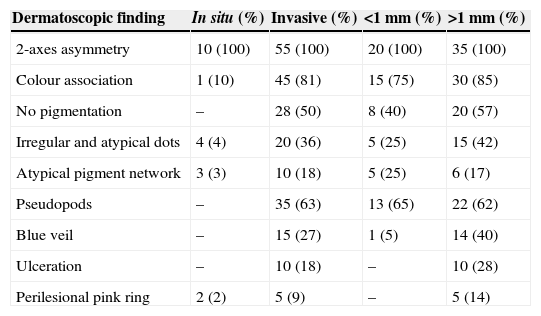
The most common dermis phototype was III in 50 patients and III in 15. The list of most common dermatoscopic findings is included in Table 2. The most frequent finding was 2-axes asymmetry for both in situ and invasive melanomas. It was present in all patients, followed by the association of 2 colours (91%) and pseudopods (63%).
Dermatoscopic findings.
| Dermatoscopic finding | In situ (%) | Invasive (%) | <1mm (%) | >1mm (%) |
|---|---|---|---|---|
| 2-axes asymmetry | 10 (100) | 55 (100) | 20 (100) | 35 (100) |
| Colour association | 1 (10) | 45 (81) | 15 (75) | 30 (85) |
| No pigmentation | – | 28 (50) | 8 (40) | 20 (57) |
| Irregular and atypical dots | 4 (4) | 20 (36) | 5 (25) | 15 (42) |
| Atypical pigment network | 3 (3) | 10 (18) | 5 (25) | 6 (17) |
| Pseudopods | – | 35 (63) | 13 (65) | 22 (62) |
| Blue veil | – | 15 (27) | 1 (5) | 14 (40) |
| Ulceration | – | 10 (18) | – | 10 (28) |
| Perilesional pink ring | 2 (2) | 5 (9) | – | 5 (14) |
The 2-axes asymmetry is the most frequent and consistent finding in all melanomas. Some characteristics, such as areas with no pigmentation, association of 2 colours, pseudopods, blue veil and ulceration, are more frequent in invasive melanomas. The presence of ulceration, blue veil and pseudopods are associated with melanomas greater than 1mm of Breslow's thickness.
In the in situ melanoma, the most frequent finding after the asymmetry was the presence of 2 colours (10%). Some findings were not present in any of the patients with in situ melanoma, such as areas with no pigmentation, ulceration, pseudopods and blue veil.
In the invasive melanoma, the third most frequent finding after the asymmetry and the association of 2 colours was the presence of pseudopods (63%), followed by areas with no pigmentation (50%) and atypical irregular dots (36%).
The presence of 2 or more colours, areas with no pigmentation, pseudopods, blue veil and ulceration were the most frequent findings in cases of invasive melanomas with a Breslow level above 1mm.
DiscussionIt has been demonstrated, with level 1 clinical evidence, that dermatoscopy has a higher sensitivity and specificity for the early detection of cutaneous melanoma than the “naked-eye” clinical assessment.1 It allows for the identification of microscopic findings that would not be noticed in clinical analyses, as well as lesions not only with suspected melanoma but also with a level of invasion higher than that of a superficial lesion, which allows the clinician to decide on the expedite treatment for this type of lesions.
The removal of the entire pigmented lesion even in risky subjects due to their physical characteristics (evidence of photo damage, phenotype I–II, skin types from 1 to 3) based solely on the clinical assessment leads to a high rate of false positives and to unnecessary surgical procedures and stress.5,6
The dermatoscopic assessment provides objective findings to determine which type of pigmented lesion is likely to be a melanoma and to identify which lesions are not superficial but rather have a significant degree of invasion, although this may not be clinically evident.7
Dermatoscopic findings depend on the type of in situ or invasive melanoma and, in invasive melanomas, findings vary according to the level of invasion.8,9 Some dermatoscopic characteristics indicate the presence of invasive melanomas greater than 1mm thick10,11; in the present series, these characteristics included the presence of 2 or more colours, ulceration, areas with no pigmentation, pseudopods (Fig. 3) and the presence of blue veil (Fig. 4).
Other characteristics of invasive melanomas, whether smaller or greater than 1mm thick, are 2-axes asymmetry and atypical network (Fig. 5).
In the in situ melanoma, the most significant finding was 2-axes asymmetry, although this melanoma shares some characteristics with invasive melanomas, such as the presence of atypical dots, atypical network and perilesional pink ring. Nevertheless, some characteristics, such as blue veil, ulceration and the presence of pseudopods, were not found. Any of these characteristics indicates the presence of an invasive melanoma greater than 1mm thick.
ConclusionDermatoscopy is a useful technique for the timely diagnosis of cutaneous melanoma. There are findings that allow for the identification of early-stage melanomas.
Dermatoscopic findings depend on the thickness of the lesion. In the case of in situ melanoma, the 2-axes asymmetry is the most important finding, while the presence of ulceration, blue veil, and association of 2 colours or more are more frequently related to invasive melanomas.
Ulceration and blue veil indicate the presence of a melanoma greater than 1mm thick.
Conflict of interestThe authors declare that there are no conflicts of interest.
Please cite this article as: Gallegos-Hernández JF, Ortiz-Maldonado AL, Minauro-Muñoz GG, Arias-Ceballos H, Hernández-Sanjuan M. Dermatoscopia en melanoma cutáneo. Cir Cir. 2015; 83: 107–111.