Mesenteric lymphangioma are rare tumours. They usually present early on in life, if congenital, or soon after trauma. The usual sites of presentation of lymphangiomas are in the neck, and axillae. In the abdomen they are more common in the mesentery, primarily of the ileum, or retroperitoneal.
ObjectiveA rare case is presented of a mesenteric lymphangioma.
Clinical caseIt involves an elderly African-American male, many years after trauma, and characterised with early satiety, causing weight loss, but without gastric outlet obstruction or vomiting. Its diagnosis, management and review of literature are presented.
ConclusionsMesenteric cysts are rare tumours that should be included as differential diagnosis in elderly patients with a history of previous abdominal trauma.
Los linfangiomas mesentéricos son tumores poco frecuentes que suelen presentarse temprano en la vida, si son congénitos, o poco después de un trauma. Los sitios habituales de presentación son en el cuello, en la axila o en la cavidad abdominal; dentro de esta, el sitio más común es en el mesenterio, principalmente del íleon, o retroperitoneal.
ObjetivoMostramos este caso clínico poco frecuente de un linfangioma mesentérico.
Caso clínicoMasculino afroamericano que presentó aumento de volumen muchos años después de un traumatismo, caracterizándose clínicamente por: saciedad temprana y pérdida de peso, pero sin obstrucción de la salida gástrica, náuseas o vómitos. Exponemos su diagnóstico, manejo y revisión de la bibliografía.
ConclusionesLos quistes mesentéricos son poco frecuentes; sin embargo, deben tenerse en cuenta como diagnóstico diferencial cuando un paciente presenta un cuadro clínico con aumento de volumen e historia de un trauma abdominal previo.
Cystic lymphangioma is a rare, benign lesion, classified as a hamartoma. It is formed by a single layer of endothelial cells, connective tissue and smooth muscle fibres.1 It generally occurs in areas surrounded by connective tissue.
They present most commonly in infancy, with an incidence of 1/20,000.2 Sixty-five percent are present at birth and 90% are diagnosed in children under 2 years of age. In adults, the incidence is between 1/100,000 and 1/250,000.3 Cystic lymphangioma can present in any part of the body, the neck being the most common (75%), the axillary region (20%) and the mediastinum, oesophagus, spleen, liver and other abdominal organs (4%).4 They present in the mesentery in approximately 1% of cases, and within this group they are most commonly found in the small bowel (85%), mesocolon (10%) and retroperitoneum (5%).5
In the adult population, cysts are generally asymptomatic, but they can present with different symptoms depending on their location, size and the organ affected. Paediatric patients present a clinical picture with a shorter duration and with more acute symptoms, and therefore they frequently require emergency surgery.
Because the most common location of cystic lymphangioma is the ileum, the main symptom is chronic abdominal pain and abdominal distension.6 However, cases have been described of acute pain and peritonitis due to rupture,7 torsion, infection, due to a volvulus or intestinal obstruction secondary to the cyst.8 In a study by De Perrot et al.9 the most common physical finding, present in up to 61% of patients, was a compressible abdominal mass.
ObjectiveWe present a case of a gastrocolic omental cyst in a male in the sixth decade of life.
Clinical caseWe present the case of a 67-year-old man, an African American war veteran with a previous history of exploratory laparotomy (37 years ago) for a liver injury secondary to a firearm wound in the upper right quadrant, for which a right subcostal incision was made. The patient did not know the details of this procedure, but stated that none of his abdominal organs had been resected.
He consulted with increased abdominal volume, which he presented many years after the liver injury, accompanied by early satiety and a feeling of gastric fullness after small meals, progressing to nausea without vomiting or diarrhoea, and significant weight loss of 10kg over 6 months. On physical examination the abdomen was soft, not painful and not distended. The increased volume was palpable in the upper right quadrant, below the subcostal incision. It had smooth edges and was not mobile on palpation. The laboratory tests that included viral hepatitis serology and alpha-fetoprotein were normal.
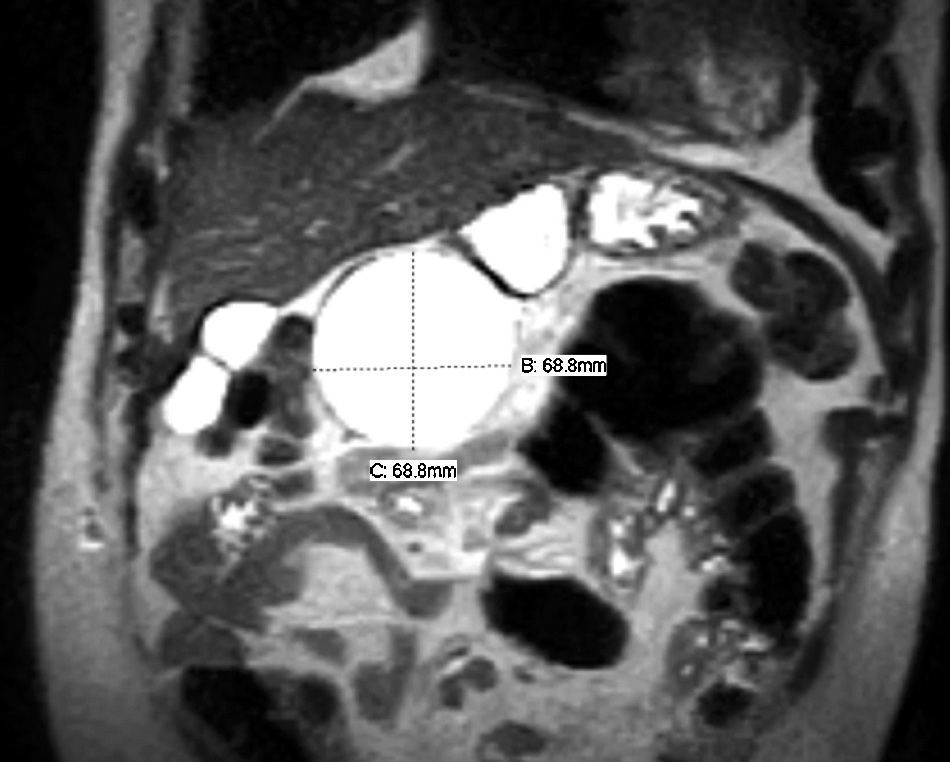
An abdominal CT scan was performed which revealed a cystic lesion contiguous to the lower face of the left liver lobe. This was confirmed by MRI, which showed a cystic lesion with a clear plane between it and the liver. The cyst was in front of the head of pancreas and the duodenum, and therefore an endoscopic ultrasound was performed which confirmed that it was not in continuity with the pancreas or the pancreatic duct. We attempted to take a sample of the fluid during this procedure, but this was not possible. Most of the results confirmed the diagnosis of a benign cyst; we therefore decided to observe the patient over 6 weeks. During this time the patient's symptoms persisted, he was therefore scheduled for laparotomy (Fig. 1) due to the history of previous surgery to the right hypochondrium, near the lesion in question. We decided that laparotomy provided better access than laparoscopy due to the adhesions and because little was known about the previous procedure.
With the patient under general anaesthetic, we palpated the right hypochondrium where the edges of the cyst were palpable and easily delineated. We decided to start with an 8cm incision in the midline.
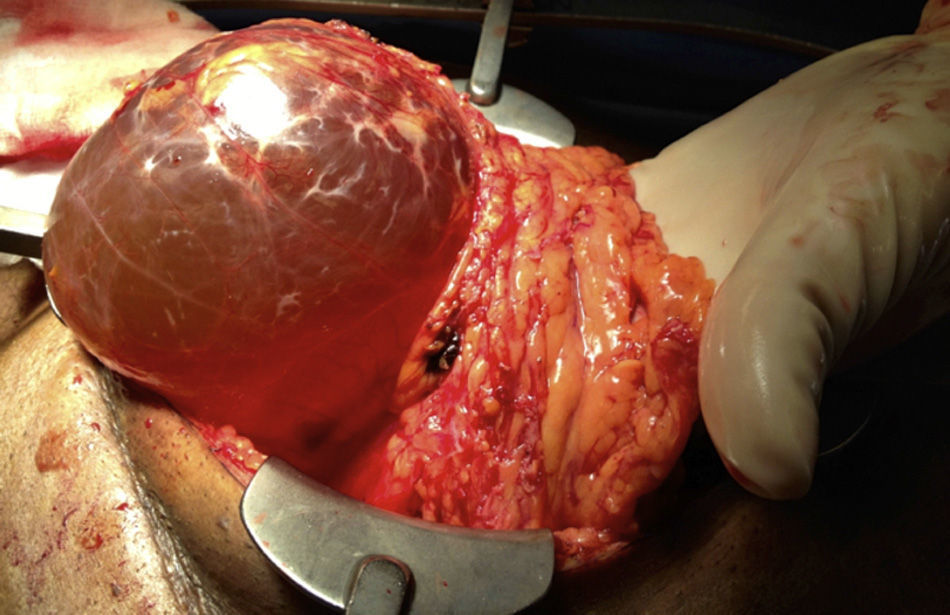
After extensive adhesiolysis, we observed a mobile, clearly translucent cystic lesion of 14cm×10cm×10cm under the liver, anterior and lateral to the pylorus in the area of the gastrocolic mesentery. After careful dissection, we ligated the vessels of the omentum near the surface of the cyst. A sample of the fluid was taken, which was translucent, slightly yellow and had no subnatant matter and no bile, blood, pus or mucus were found. Haemostasis was performed, and we examined the mesentery of the transverse colon that was found to be intact. No reduction in colon perfusion was observed, which confirmed that the lesion was not in continuity with its mesentery. No lesions to the adjacent organs were observed either (Fig. 2).
The histopathological report showed that the cells covering the cystic spaces were positive for CD34, factor VIII, WT-1, CD31 and D2-40, and negative for cytokeratine-5/6, calretinin and HBME-1. Based on the results of immunohistochemical analysis, the definitive diagnosis was benign cystic lymphangioma. Venous cystic lesion and mesothelial inclusion cyst were ruled out as differential diagnoses.
The patient recovered without incident after surgery. At 4 months’ follow-up he had recovered his appetite and gained weight.
DiscussionThe aetiology of mesenteric cysts is not clear. Some of the accepted theories include a benign lymphatic proliferation, which does not communicate with the rest of the lymphatic system, or a fault in fusion of the mesenteric layers.10 The lesions can have blood or lymphatic vessels, and therefore can contain serous, haemorrhagic or lymphatic material.
Traumatic or infectious cysts usually have a fibrous wall, foamy cells, cholesterol granuloma, and absence of epithelium and histologically they resemble pancreatic pseudocysts. They normally present within a couple of months to one year after traumatic injury. They can present through a mesenteric injury and cause a lymphatic vessel to rupture which will cause slow leakage of lymph fluid. In this case, the medical history of a firearm wound in the vicinity of the cyst made us consider trauma as the cause of the abdominal cyst formation, although the cyst formation time was much longer than that described in the literature.
In the case we present, the cyst wall has specific features of a congenital cyst, since it did not show changes suggestive of a traumatic cyst and it presented in an elderly patient, when 80% of these cysts present in children under the age of 5.11
Because the most common location is the mesentery of the ileum,12 the principal symptom is chronic abdominal pain and abdominal distension, which subsequently causes a total or partial obstruction of the small bowel. The presentation of this case is unusual, since patients rarely complain of weight loss and early satiety. This patient's symptoms could be attributed to the cyst being located in the gastrocolic omentum and the increased size caused compression to the stomach, affecting its emptying, and as a result the patient's satiety. In our review of the literature we found no record of a cyst in this region and with these symptoms.
Initially, the diagnosis was established in the operating theatre after exploratory laparotomy for non-specific symptoms. Preoperative imaging, ultrasound and computed axial tomography (CAT) are currently principally used to achieve a diagnosis. Ultrasound is useful for observing the content of the cyst. CAT is more sensitive in discerning cysts of neighbouring organs.13 Magnetic resonance is an auxiliary procedure to distinguish mesenteric cysts from other abdominal cystic tumours, and is more sensitive than ultrasound in classifying their content.14,15
The treatment of choice is enucleation of the lesion, which might require intestinal resection in specific cases when the cyst involves the intestinal mesenteric vasculature. An attempt at partial resection with marsupialisation of the cavity to avoid resection has been described in the literature, but in these cases this increases the possibility of a recurrence of the cyst.16 In a study by Prakash et al.17 41% of cases were completely enucleated, 2% required intestinal resection and marsupialisation was performed in 35%. In this case, we were able to enucleate the cyst completely, without damaging any of the surrounding structures.
Very many reports have been written on laparoscopic resection of a mesenteric cyst.18 In this case we decided to take an open approach because of the patient's prior surgery to the area and the scant information that we had about that procedure.
ConclusionsMesenteric cysts are rare and usually present early in life if they are congenital, or shortly after trauma. However they should be considered as a differential diagnosis in adults when the patient presents a clinical picture with increased abdominal volume and a history of abdominal trauma or with symptoms of increased volume causing compression.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors have no conflict of interest to declare.
Please cite this article as: Serrano-Rodríguez P, Desai CS. Quiste omental gastrocólico en un adulto: presentación de un caso y revisión de la bibliografía. Cir Cir. 2016;84:509–512.